![]()
Part 1
Understanding osteoporosis
![]()
Chapter 1
What is osteoporosis?
You may not think of your bones as being alive, but they are. Every day, your body breaks down old bone and replaces it with new. As you get older, however, the ratio becomes unequal: You lose more bone than you gain. If you lose too much, you can develop the bone disease osteoporosis.
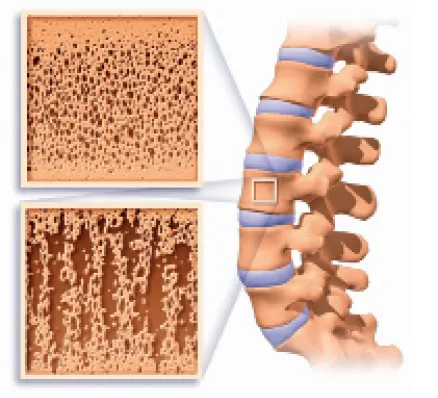
Osteoporosis causes bones to become weak, brittle and prone to fracture. The word osteoporosis means “porous bones.” It’s an apt description of what happens to your skeleton if you have the disease. Due to loss of bone tissue, bones that were once dense and strong may be unable to withstand the stress of even normal activity, such as bending over or twisting to look behind you.
Until recently, osteoporosis was considered a natural part of aging, similar to getting gray hair or developing wrinkles. But there’s nothing natural, or healthy, about losing 4 inches of height. And it certainly isn’t natural to break a bone from coughing or receiving a hug.
But that’s precisely what can happen if you’re one of the more than 40 million Americans who have osteoporosis or are at high risk due to reduced bone mass.
The good news is the disease is as preventable and treatable as it is common. The keys to successfully avoiding osteoporosis are building a strong skeleton when you’re young and slowing the rate of bone loss as you age. Even if you already have osteoporosis, good nutrition, exercise and medications can slow, or even reverse, its progression. It’s never too late to do something about your bone health.
Osteoporosis risks
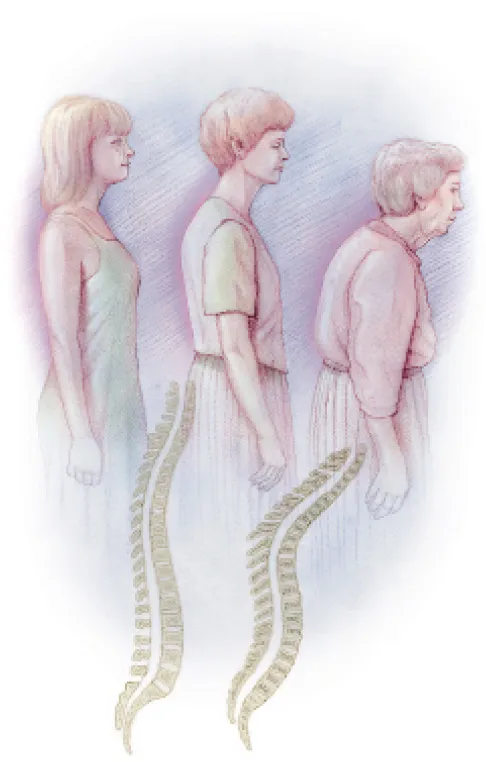
Each year osteoporosis is responsible for more than 2 million fractures. Typically these fractures occur in the spine, hip or wrist, but they may happen in other bones as well. A compression fracture of the spine causes your vertebrae to collapse and may lead to lost inches of height and a stooped posture. Fractures of the hip can change lives. Only about one-third of those who break a hip return to being as active as they were before the fracture. And nearly one-third go to a nursing home permanently. As if that’s not enough, add chronic pain and feelings of anxiety and depression to the mix of problems that osteoporosis can cause.
Osteoporosis is most common among postmenopausal women. If you’re a female age 50 or older, you have an eye-opening 50 percent chance of breaking a bone during your remaining lifetime. Statistics indicate your risk of breaking a hip is about the same as your combined risk of developing breast, uterine or ovarian cancer. Although fewer men than women get osteoporosis, men have a higher risk of death after breaking a hip.
Many people have weak bones and don’t even know it. That’s because bone loss typically happens over a long period of time and it doesn’t hurt. Oftentimes, a broken bone is the first and only indication that a person may have osteoporosis. Unfortunately, by the time a fracture occurs, the disease is often well-established. A bone density test is the best way to predict fracture risk.
Changes with age Three generations from the same family illustrate how osteoporosis can slowly lead to changes in posture and cause gradual loss of height.
• • • • •
Osteoporosis through the ages
Ancient Egyptian mummies with the telltale evidence of hip fractures suggest that osteoporosis has been a problem for humankind through the millennia. But until quite recently, osteoporosis wasn’t considered a disease. It was thought to be an inescapable part of aging. Stereotypes from literature, art and even television reinforced this idea. From the old woman who lived in a shoe (of nursery rhyme fame) to Granny on the television series The Beverly Hillbillies, older female characters were often portrayed with a tottering walk and stooped over with the so-called dowager’s hump.
In the 1830s, a French doctor studying the effects of disease on the human body observed that some people’s bones were honeycombed with large holes that greatly weakened the bone structure. He was the first person to describe this condition, which he termed osteoporosis. Unfortunately, the French doctor didn’t consider this to be a sign of disease and continued his investigation along different paths.
In the 1940s, Fuller Albright, M.D., of Massachusetts General Hospital, made the connection between the hormone estrogen and osteoporosis. He noticed that many of his patients who had problems with weak bones and fractures were older women past menopause. Dr. Albright believed the sharp drop in estrogen that occurs during menopause was causing the abnormal loss of bone. He correctly identified the condition as postmenopausal osteoporosis.
Still, old notions continued to prevail. Until just the past few decades, women were often told to take calcium and “live with it.” But new discoveries have transformed doctors’ understanding of the disease. Osteoporosis isn’t just an issue for older women. Bone building when you’re young and growing is just as important as slowing bone loss as you age.
• • • • •
Your bone bank
Think of your skeleton as a bone bank. Just as your financial health benefits from funds that you put aside and can draw on in times of need, your bone health benefits from a fund of calcium and other minerals that you store in your skeleton. Good bone health depends on keeping your bone bank account amply supplied with minerals that are able to meet all of your body’s needs.
Lots of transactions take place in your bone bank account. That’s because throughout your life, new bone is constantly being formed and deposited, while old or worn-out bone is constantly being broken down and withdrawn. By way of this process, your skeleton refurbishes and maintains itself. For adults, the ideal account ledger has as many deposits as it does withdrawals.
Bone Normal bone is strong and flexible (top left). Osteoporotic bone is more porous, weaker and subject to fracture (bottom left).
Here are some key terms that relate to the bone bank concept. Bone mass is the total amount of bone tissue you have in your skeleton. Think of it as the total assets in your account at any time. Bone density refers to how tightly that tissue is packed — how mineral-rich your bones are. Envision dollar bills crammed into a safe deposit box. Bone strength refers to the ability of bone to withstand stress and is dependent on bone quality, including mass and density. You might compare this to your bank account’s ability to handle large daily transactions.
In other words, the more bone you have and the denser it is, the stronger your skeleton — the more plentiful your bone bank account. Strong bones make it less likely that you’ll develop osteoporosis or experience fractures.
Not enough bone in the bank
During your younger years, you’re constantly making deposits to your bone bank account. But around age 30 things begin to change. Withdrawals from your account begin to exceed your deposits. You gradually start losing bone mass and bone density. This is normal. What’s not normal is when withdrawals exceed deposits at such a rate that portions of your skeleton become weak and brittle. Researchers have yet to learn all of the reasons why this occurs. Many factors are likely involved.
Of course, bone loss doesn’t mean that you actually lose whole chunks of bone. It’s the mineral content of your bones that’s depleted. The outer shell of bone becomes thinner, and the interior becomes more porous. This action bankrupts your skeleton of its strength. Under a microscope, a bone affected by osteoporosis looks like a steel bridge with many girders missing. Like a weakened bridge, it may no longer be able to endure the everyday stresses and strains placed on it.
Your risk of osteoporosis doesn’t depend only on your current rate of bone loss. It also depends on how much bone you banked in your account when you were young and growing. This makes the disease equally concerning to a younger person as it is to an older adult.
• • • • •
Osteoporosis is not osteoarthritis
Osteoporosis and osteoarthritis are different conditions with very different signs and symptoms, but people sometimes confuse the two. Osteoporosis weakens your bones. Osteoarthritis affects your joints, the locations where bones join to one another. It wears away the cartilage that cushions your bones and keeps them from rubbing against each other. Painful and deformed joints are common signs of osteoarthritis. Osteoporosis often goes unnoticed until a bone is broken.
• • • • •
Signs and symptoms
Osteoporosis is often referred to as a silent thief because the bone loss it causes occurs painlessly over many years. And even in instances when the loss is abnormally rapid, during the early stages you may not experience signs or symptoms.
Then, one day, you break a bone while doing a routine task — maybe you crack a rib while lifting the laundry basket or fracture a vertebra while bending down to tie your shoes. At this point, the disease may already be well-established and parts of your skeleton may already be quite weak and susceptible to fracture.
Other signs and symptoms may occur if you’ve experienced a compression fracture of the spine, including:
- Back pain
- Loss of height
- Stooped posture
Remember that back pain, loss of height or stooped posture doesn’t mean you have osteoporosis. Only if you’ve experienced a compression fracture does the disease generally produce back pain. The most common causes of back pain are muscle strain and disk injury. However, because there’s the possibility that back pain could stem from an osteoporosis-related fracture, it’s important to see a doctor to determine the cause and take appropriate action.
Because, in its early stages, there are no clues that you may be developing osteoporosis, it’s important to be aware of factors that put you at increased risk (see Chapter 4). If you’re concerned that you may be at increased risk of the disease, have a bone density test before your skeleton becomes weakened. Remember, the best t...