![]()
1 Why Nurses, Midwives and Health Visitors need Health Psychology
Key Learning Objectives
At the end of this chapter you will be able to explain:
Introduction
Across all age groups and conditions, nurses, midwives and health visitors are helping patients and their relatives to adjust to diagnoses, to cope with treatment regiments and other disease-related life changes, to manage symptoms and to make healthy choices.
This book takes an evidence-based approach to inform and explore how health psychology theories and techniques are useful to us as clinicians in this work. Throughout the book, practical examples of health psychology in action will be given for you to relate to your practice. Research evidence will be critically appraised so you can decide if a particular health psychology approach will help you and your patients.
This chapter will provide an overview of what is meant by ‘health psychology’ and how it informs the way we deliver holistic and person-centred care. The health psychology theories described in this chapter will be referred to in further chapters.
Evidence-Based Practice
First a word about what research evidence is. For determining the effectiveness of an intervention, it is well established that randomised controlled trials (RCTs) provide the best evidence concerning whether or not an intervention works. This is because of their ability to control for bias and for both known and unknown variables which may have an effect on outcomes above and beyond the intervention being tested.
However, any trial has the potential for bias (e.g. through problems in the way it is conducted) and there may be many variables which cannot all be considered by an individual trial. Hence systematic reviews of RCTs which identify, appraise and bring together, or ‘synthesise’, all available RCTs are likely to provide the most useful and concise evidence for clinicians: in a well conducted systematic review the evidence is critiqued and all available evidence is brought together to save you reading through multiple papers. In this book, when considering whether an intervention works or not, systematic reviews of RCTs will be presented as the first line of evidence and individual RCTs only cited where there is no systematic review or when the search date of the latest systematic review was so long ago that the review may be out of date.
When interpreting a body of evidence, it is important to remember that a finding of weak evidence or of a lack of evidence is not the same as a finding of no effect. That may sound obvious, but it is important to be clear that a lack of evidence simply means that insufficient, good-quality trials have been conducted to determine whether or not an intervention works. A finding of no effect, on the other hand, would result from good-quality trials demonstrating that an intervention did not work. When confronted with a lack of evidence, or evidence that is weak, we have to apply our clinical judgement and think critically whether or how a particular theory or intervention may be useful to us in our clinical practice. This is the science and art of evidence-based practice.
Of course, RCTs are only useful for determining whether an intervention works or not. We will rely on different types of research evidence, such as quantitative, observational studies or qualitative studies, to tell us whether ideas or theories are useful or not. Whether research evidence is valid and reliable will depend on two factors: 1) was the research design appropriate to answer the research question? and 2) was the study well conducted? In this book, the strengths and weakness of cited research evidence will be discussed as far as possible, but all healthcare professionals need to be able to critically appraise research in order to make evidence-based decisions; there are many excellent resources available to help you develop this skill (see Further Reading). Finally, healthcare practice is often informed by guidelines produced by government or professional bodies. Critical appraisal skills will help you to understand whether or not a guideline is evidence-based and hence how or whether it should be implemented. Now let us consider how health psychology can help our clinical practice.
Health Psychology and How it can Help us as Nurses, Midwives or Health Visitors
Psychology is the scientific study of people, the mind and behaviour. Health psychology is the application of psychological knowledge to the study of people’s experience of health and illness. Health psychology research typically tries to predict or change how people will behave when they have a given illness, with the aim of improving physical and mental health outcomes and general wellbeing. These aims are shared by nurses, midwives and health visitors for their patients or clients.
Nurses, midwives and health visitors, of course, also conduct research. Combining what we know from nursing and health psychology enhances this research. This is especially the case in the field of behaviour change, which is important in the management of long-term conditions and health promotion – key areas of practice and research for many nurses, midwives and health visitors.
Specialist health psychologists may be part of the clinical team. Their role is to help people with the psychological and emotional aspects of illness or treatments and to support people with long-term conditions. This links closely with what nurses, midwives and health visitors do. At times we may need to provide very basic care, but a key part of our role is to ensure that patients or clients can self-manage in order to increase their independence, quality of life and their ability to cope in future. Health psychology theories and research, which predict how people may respond to illness and explain what is needed for people to manage their health, can help nurses, midwives and health visitors to do this.
Theories of Health and Behaviour
To help you judge their value, as you read about theories of health and behaviour, bear in mind the information in Box 1.1 which summarises the properties of a good theory in social science.
Most nurses, midwives and health visitors will be familiar with the biomedical and the biopsychosocial models of health.
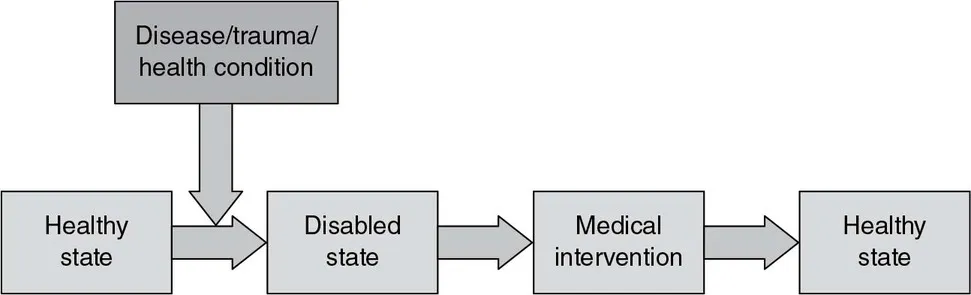
The Biomedical Model
This model, or way of thinking about health, was dominant through most of the 20th century. It is a linear, unidirectional model where health is considered simply to be the absence of disease. Illness is seen as within the body, causing bodily symptoms that lead on to disability and restrictions on social life (Figure 1.1). The body can therefore be mended like a machine: removing part of a body or adding chemicals to it will lead to cure or avoidance of death.
However, the model was soon recognised as too simplistic and an alternative model – the biopsychosocial model – was proposed by psychiatrist George Engel (Engel, 1977) who advocated its use in research, teaching, and the provision of healthcare.
Figure 1.1 The Biomedical Model
Adapted from a figure produced by Paul Leimkuehler for the American Academy of Orthotists and Prosthetists.
Box 1.1: What makes a good theory in social science?
- Parsimony – explains a phenomenon in few terms as simply as possible
- Breadth – can be applied to a range of situations
- Accuracy – can produce testable predictions
- Falsifiable – it can be disproved
- Known moderators – specifies variables that tell you when relationships can and can’t be expected
- Known mediators – specifies variables that tell you how or why a relationship occurs
- Fruitfulness – leads to new ideas
The Biopsychosocial Model
This model recognises the contribution of biomedical, psychological and social factors to health (Figure 1.2). Biomedical factors include our genes, anatomy, physiology, bacteria and viruses; psychological factors may be our personality, behaviours and beliefs; social factors include social class, gender, ethnicity and socio-economic status.
How the Biopsychosocial Model Improves on the Biomedical Model
The biomedical model predicts an external cause of disease, but none may be found. For instance, in ‘medically unexplained syndromes’ such as irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia and chronic low back pain, a person may experience very real and disabling symptoms but no medical reason can be identified. A biological cause for many severe mental illnesses has yet to be found.
Figure 1.2 The Biopsychosocial Model: a holistic model
Adapted and reproduced with kind permission of the American Academy of Orthotists and Prosthetists.
The biopsychosocial model does not focus solely on cause, but recognises that beliefs and behaviours around illness can influence symptoms. We will look at this in more detail when we consider specific psychological theories.
The biomedical model also cannot explain individual variation in illness experience. For instance, two people with the same disease severity may report wide variation in their quality of life. The biopsychosocial model would predict that variation in psychological factors such as personality or cognition, or in social factors, such as available resources, are important. Compared to the other, one of the individuals may be more ‘resilient’ or able to distract themselves from symptoms, or they may have more family or practical support (someone to do the shopping) so that symptoms have less impact.
The ‘placebo effect’, where simply the expectation of cure can be beneficial, would fit with the biopsychosocial model which considers the impact of psycho...