
Clinical Governance
A Guide to Implementation for Healthcare Professionals
Robert McSherry, Paddy Pearce
- English
- ePUB (handyfreundlich)
- Über iOS und Android verfügbar
Clinical Governance
A Guide to Implementation for Healthcare Professionals
Robert McSherry, Paddy Pearce
Über dieses Buch
Clinical Governance: A Guide to Implementation for Healthcare Professionals provides a comprehensive overview of what is meant by clinical governance and how it can be implemented in practice. It explores the evolution of clinical governance, its key components, legal implications, the barriers to implementing it, and its impact.
Clinical Governance provides step-by-step practical advice, facilitating better understanding of the key principles of clinical governance. This third edition has been fully updated throughout to incorporate a more integrated approach to achieving clinical governance, with an additional chapter on education and training. Each chapter includes reflective questions, activities and case studies taken from clinical practice as well as a full list of references and further reading.
Häufig gestellte Fragen
Information
Chapter 1
Introduction and Background: Clinical Governance and the National Health Service
Introduction
Background
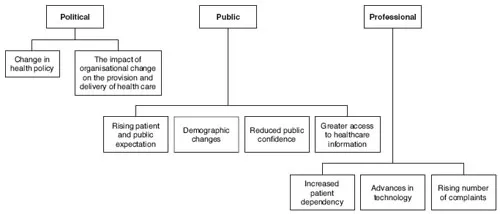
Why the need for clinical governance?
Activity 1.1 Reflective question.
to give citizens a stronger voice in how their health and social care services are delivered. Run by local individuals and groups and independently supported – the role of LINks is to find out what people want, monitor local services and to use their powers to hold them to account.
Political
politics with a small p makes the world go round. Getting things done, seeking support, building alliances, compromising – that’s all politics, and inescapable and natural. (p. 35)
Changes in health policy
that general managers should be appointed at all levels in the NHS to provide leadership, introduce a continual search for change and cost improvement, motivate staff and develop a more dynamic management approach. (Ham 1986, p. 33)
Absence of this general management support means that there is no driving force seeking and accepting direct and personal responsibility for developing management plans, securing their implementation and monitoring actual achievement. It means that the process of devolution of responsibility, includi...
Inhaltsverzeichnis
- Cover
- Table of Contents
- Dedication
- Title
- Copyright
- Foreword
- Preface
- Chapter 1: Introduction and Background: Clinical Governance and the National Health Service
- Chapter 2: What is Clinical Governance?
- Chapter 3: A Guide to Clinical Governance
- Chapter 4: Applying Clinical Governance in Daily Practice
- Chapter 5: Identifying and Exploring the Barriers to the Implementation of Clinical Governance
- Chapter 6: Clinical Governance and the Law
- Chapter 7: The Impact of Clinical Governance in the National Health Service
- Chapter 8: Education and Training for Clinical Governance
- Chapter 9: Conclusion: The Future of Clinical Governance for Healthcare Professionals
- Index
- End User License Agreement