![]()
Part 1
Haematology, Blood Transfusion and Immunology
Objectives and scope
The learning objectives for Part 1 are overleaf. The purpose of the Haematology Laboratory is to provide assistance in diagnosing, monitoring and treating patients. The Blood Transfusion Laboratory provides blood components (mostly red cells, but also coagulation factors and the blood protein albumin) for patients at risk of potentially life-threatening situations. The Immunology Laboratory is generally concerned with antibodies, often reacting with the patient’s own tissues, and so causing autoimmunity.
In order to provide clinical practitioners with the information they need, the components of the blood are analysed, almost always in custom-designed equipment. Of course, all blood tubes and forms must be fully labelled by those taking the blood in order to minimise the risk of (possibly fatal) error. Indeed, the laboratory will be well within its rights to decline to test a sample that is incorrectly or inadequately labelled.
There are three basic blood tubes that are used in these disciplines. A full blood count (FBC) is performed on blood that is anticoagulated with ethylenediamine tetra-acetic acid (EDTA). Coagulation tests are invariably done on plasma that is obtained from whole blood anticoagulated with sodium citrate. The erythrocyte sedimentation rate (ESR) may be assessed on blood that is held within its own dedicated glass tube: blood clotting in this tube is also prevented by sodium citrate. However, in some cases, the ESR can be measured using the same sample as is the FBC. For blood transfusion, an EDTA or a tube free of an anticoagulant (providing serum) is often used. Immunologists can work with serum or plasma, but for cell work the blood must be anticoagulated. Once more, if you are in even the slightest doubt about which vacutainer to take for whichever test – PHONE!!
Testing can only be performed on blood that is collected in the correct tube. Failure to do so will, at best, result in a polite phone call from the lab explaining the problem and its remedy. At worst, a report will be returned a day or so later with a comment such as ‘inappropriate blood sample received, please repeat’. To help this, many blood tubes have different-coloured tops to make this process easier and minimise errors.
Fortunately, haematology can be divided very easily into three different areas. These are the red blood cell, the white blood cell and coagulation. The most important aspects of each of these are, in turn, anaemia, infection and neoplasia, and thrombosis and haemorrhage. (Blood transfusion and immunology are addressed in their own chapters, where a transfusion reaction and autoantibodies, respectively, are key.)
Finally, it would be good if the reader could translate these concepts into ‘real-life’ interpretation, such as the implications of a haemoglobin count of 84g/L, with or without a white blood cell count of 15 × 109/L, the possible problems and benefits of INR of 4.0, the consequences of an incompatible blood transfusion, and a knowledge of autoimmunity, hypersensitivity and immunodeficiency.
Learning objectives – Haematology, blood transfusion and immunology
Having completed this section, the reader will:
1. Appreciate the importance of different anticoagulants and glass tubes for the different blood tests requested.
These are EDTA (for a full blood count) and sodium citrate (for coagulation) ESR may require its own special tube. The Blood Bank generally needs a sample of clotted blood or blood taken into EDTA.
2. Recognise the major areas of interest:
• The red blood cell
• The white blood cell
• Coagulation
• Blood transfusion
• Immunology
3. Describe major problems associated with each of these areas, e.g., respectively:
• Anaemia
• Infection/neoplasia
• Thrombosis/haemorrhage
• An incompatible blood transfusion
• Autoantibodies
4. Interpret simple haematological results such as:
• A haemoglobin of 8.4g/L
• A white cell count of 15 × 109/L
• A prothrombin time of 25 seconds.
• A high titre of antinuclear antibodies
5. Understand the importance of the Haematology Laboratory
The haematology ‘syllabus’
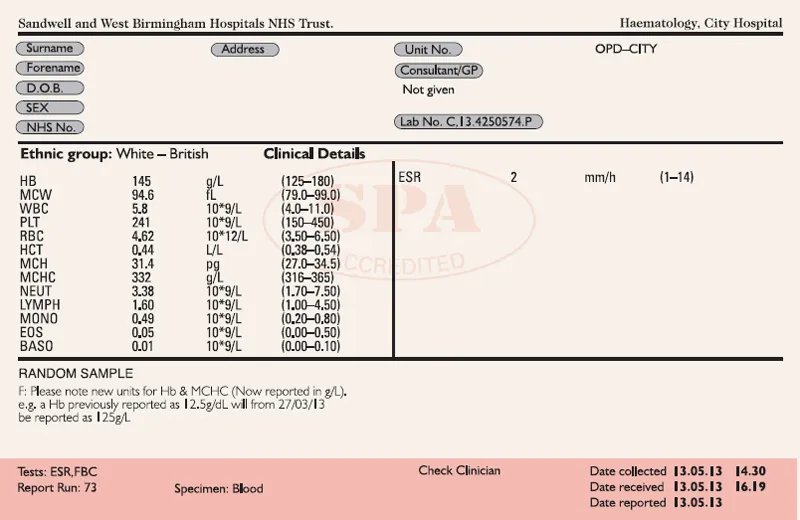
The form shown in Figure 1 is the full blood count (FBC). This is the most requested haematology test, and this example was produced by the author’s laboratory for the end user (i.e. the requesting practitioner). This form will generally end up in the patient’s notes. Apart from the usual demographic details (age, sex, hospital number, ward, consultant, etc.), the report offers (from left to right) a column of abbreviations (particular tests), a column of numbers (the result), another column of numbers and letters (units), and finally a column of numbers (the [male] normal or target range).
The FBC has details of red blood cells, white blood cells and platelets. The main objective of this section of the book is to explain to you what all of this means.
Figure 1: Haematology Report Form
![]()
1
The red blood cell
Key words:
Haemoglobin (Hb)
Red blood cell count (RBCC)
Haematocrit (Hct)
Red cell indices:
Mean cell volume (MCV)
Mean cell haemoglobin (MCH)
Mean cell haemoglobin concentration (MCHC)
Erythrocyte sedimentation rate (ESR)
Plasma viscosity (NB: not strictly to do with the red blood cell)
Key pathological expressions:
Anaemia
Polycythaemia
Thalassaemia
Sickle cell disease
An explanation of terms:
Haemoglobin (Hb)
Haemoglobin is undoubtedly the index most frequently referred to in clinical haematology. It is a protein designed to carry oxygen from the lungs to the tissues, where the oxygen is given up to participate in respiration, the process by which energy is obtained.
The reference range varies between the sexes. Lower levels in menstruating women seem obvious, but in post-menopausal women levels are still lower than in age-matched men, as the latter produce testosterone to stimulate red cell production. We know this because men who have lost their testes to accident or disease see their haemoglobin levels fall.
Red blood cell count (RBCC)
Red blood cells carry haemoglobin in the blood. Red blood cells are unusual as they lack a nucleus, thus providing additional flexibility to penetrate the smallest capillaries and so deliver oxygen to distant cells and tissues. They are the most abundant cell in the blood (often called erythrocytes), and numbers can also vary between the sexes for the same reason as haemoglobin.
Haematocrit (Hct)
The haematocrit index expresses that proportion, as a percentage (as above), or decimal (say 0.43) of whole blood, that is taken up by all the blood cells. Since there are approximately 1000 more red blood cells per unit volume than white blood cells, and 20 times as many (tiny) platelets, the red cells make up the major proportion of the haematocrit. Consequently, at the practical level, this index indicates the proportion of red blood cells that makes up the whole blood pool. The haematocrit also varies with age.
Red blood cell indices
The red blood cell indices are:
• Mean cell volume (MCV), which is the size of the average (mean) red blood cell. Note the stress is on ‘average’, as each index is the mean of millions of individual cells.
• Mean cell haemoglobin (MCH), which as the name implies, simply reports the average amount (mass) of haemoglobin in the cell. It does not take into account the size of the cell.
• Mean cell haemoglobin concentration (MCHC), which is the average concentration of haemoglobin inside the average size cell.
Error may easily be introduced. For example, an MCV of, shall we say, 90fL, may arise from cells with very diverse size, ranging from 70 to 110. Cells of such varying size must imply one or more pathological processes (such as alcoholism). But the same MCV of 90 may also be the sum of a very well-regulated population of cells that vary from, in this example, 87 to 93. For this reason, MCV is probably the most useful of the three indices, especially when investigating different types of anaemia, as we shall see.
Because several of the red cell values are mathematically derived from some of the others, it is entirely possible for any one of them to be outside the normal range whilst the other five are apparently normal. Thus one must consider all six red cell indices (and possibly some others) together to obtain a full picture. In the author’s laboratory, the haematology analyser provides the Hb, RBCC and MCV results directly from the blood provided, then (simply speaking) calculates the Hct from the RBCC times the MCV, the MCH by the Hb divided by the RBCC, and the MCHC by the Hb divided by the Hct, with adjustments (e.g. multiply or divide by 10 or 100).
Erythrocyte sedimentation rate (ESR)
The ESR is also a global score of physical aspects of the blood, and is simple to understand. The result is obtained by allowing a thin column of blood to settle down under the influence of gravity. As it does so, the red blood cells will separate from the plasma, so that after an hour, a band of clear plasma will sit atop the red blood cells. The fall in the level of the red blood cells is then recorded as mm/hour. The effects of platelets and white blood cells are minimal and are ignored. It is therefore unique in requiring no sophisticated machinery and few technical skills.
An increased ESR can be caused by many factors, including cancer, infections, anaemia, inflammation, renal failure, rheumatoid arthritis, multiple myeloma and tuberculosis. It is increased soon after myocardial infarction, and is also heavily influenced by plasma proteins.
Some laboratories have a more liberal normal range, e.g. <20mm/hour, especially in the elderly.
Plasma viscosity
Plasma viscosity does not really have much to do with red blood cells, but is in this chapter purely for convenience. This index provides an idea of how thick or thin the plasma has become – whether it is thinner, and more like water (tending towards a low result of less than 1.5), or thicker and more like treacle (tending towards a high result, over 1.72).
Viscosity records a global property of the plasma, not individual molecules. Indeed, the molecules that make up the major component of viscosity include fibrinogen, al...