![]()
Chapter 1
Historical Background and Book Contents
1.1Discoveries of the Circulation
That “blood moves in closed circle” was apparently known in the Far East, several millennia ago, about 2,650 B.C., as recorded in the book by the Yellow Emperor of China written in the Canon of Medicine (Nei Ching). Ancient Chinese practitioners customarily felt palpable wrist artery (radial artery) pulsations as a means of diagnosing the cardiac state of their patients. In this approach, the practitioners were able to obtain both the strength of the pulsation to infer the vigor of contraction of the heart, and the interval duration of the pulses, hence heart rate. This seemingly indicates that the importance of the rate-pressure product, now a popular clinical index of myocardial oxygen consumption, might even have been considered pertinent at that time. The supply and demand of oxygenation, as well as its proper utilization in terms of energy balance, or ying-yang, is center to achieving body harmony. Thus, this suggestion of an intrinsic transfer of the energy (Chi) generated by the heart to the peripheral arteries may have been known since antiquity, although the theoretical foundation was not established until much later.
In the West, the observation that man must inspire air to sustain life led ancient scientists and philosophers to toy with the idea that arteries contained air rather than blood. This was the notion originally attributed to Erasistratus in the third century B.C., following the teaching of Aristotle. Aristotle and later Herophilus performed numerous anatomical studies and the latter discovered the connecting arteries to the contracting heart. That arteries themselves contract and relax thus was known in Aristotle’s time. Arterial properties in terms of elastic stiffness, distensibility and compliance, as we know now, were not fully described. Galen’s (130-200) description of the ebb and flow of blood in arteries, though lasted for centuries, was grossly inaccurate. Additionally, in the Galenic view, blood was passed from the right side of the heart to the left side through pores, which was later shown to be incorrect as they do not exist within the inter-ventricular septum, as demonstrated by Columbus (1516-1559), a Belgian anatomist. Otherwise, this would be known as the septal defect. Columbus, during his many dissections, confirmed that venous blood of the right ventricle passed into the left ventricle through the lungs. This was concluded a few years earlier by Servetus (1511-1553), a Spanish theologian and physician. Thus, the open-circuit interpretation of the circulation by Galen cannot accurately describe the “circulation of blood”.
In his many teachings, though some aspects were later known to be erroneous, Galen was nevertheless the first to recognize that the walls of arteries are thicker than those of the veins, and that arteries were connected to veins. It was the Persian physician Ibn al-Nafis (1210-1288) who claimed that venous blood of the right ventricle is carried by the artery-like vein into the lungs, where it mixes with the air and then into the left ventricle through vein-like artery.
Galileo Galilei (1564-1642) in his “Dialogue of the Two Sciences”, which appeared in 1637, suggested the circulation of blood in a closed system. Centuries later today, the idea of the circulation of blood was credited to William Harvey (1578-1657), a contemporary of Galileo, in his now famous “De Motu Cordis and De Circulatione Sanguinis” (1628) presented to King Charles of England. He described in his “Anatomical Exercises” that “blood does continually passes through the heart” and that “blood flow continually out the arteries and into the veins”. Harvey’s work indicated the pulsatile nature of blood as a consequence of intermittent inflow, during roughly one-third of the heart cycle, now known as systole, in combination with essentially steady outflow through the periphery during the remaining cardiac period, the diastole.
Harvey’s work was completed before Malphighi who worked with the aid of a compound microscope. He reported in 1661 the discovery of the capillaries linking the arterial circulation to the venous circulation, while he was working with the microscopic anatomy of the pulmonary parenchyma in the frog, an uni-ventricular amphibian. Dutch anatomist Van Leeuwenhoek (1632-1723) confirmed the capillaries in different organs of several animal species and established the concept of the capillary bed. Bypassing the capillaries are the arterio-venous anastomoses, which are now known to perform the function of controlling blood flow.
German anatomist Henle discovered the smooth muscle cells in small arteries in 1841. Thus, this provided the first evidence that smooth muscle contributes to arterial contraction. But it is not until almost a century later in 1937 that Zweifach showed that active contractility of the micro-vessels is confined to those vessels with smooth muscle cells.
In the investigation of the microcirculation, credit was given to Hall, an English physiologist, first to differentiate the capillaries from arterioles. The fact that capillaries transfer water and water-soluble substances from the blood stream to the surrounding tissues, were shown by Starling (1866-1927) and is now known as the Starling’s hypothesis governing fluid exchange. The measurement of capillary blood pressure by cannulation was first performed in 1930, by Landis, in the nail microvascular bed (Mayrovitz, 1998). The ultra-structure of the microcirculation has now been established from electron microscope studies.
French physiologist Claude Bernard in 1852 showed that stimulation of sympathetic nerves induces vasoconstriction and the concept of controlling blood flow by vasomotor nerves. Neural control of the circulation is recognized as an important aspect in the regulation of vascular function.
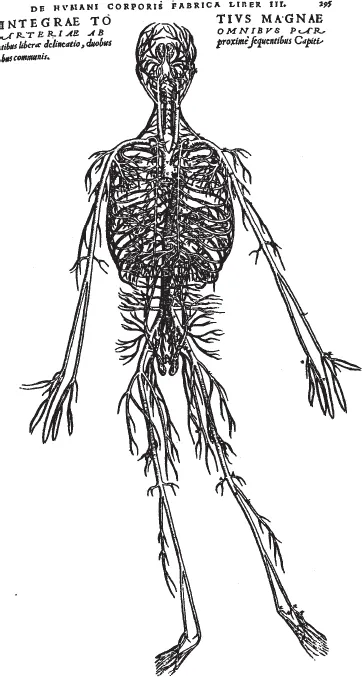
Fascinated by anatomic structure of the vascular tree, as an art, Leonardo da Vinci (1452-1519) made many detailed drawings of the constituent parts of the circulatory system. He apparently already knew that both the contraction and resting periods are necessary for the heart to function with a normal rhythm. His anatomic drawings of the heart and the perfusing arteries are, to a large extent, amazingly accurate. This includes drawings of the heart and the great vessels, together with the main, anterior descending and circumflex coronary arteries and their major branches. Several drawings of the heart valves, demonstrating how well the leaflets are arranged when the valves are closed, as well as the detailed anatomic drawing of the neck arteries in man with its branching morphology were also shown (Li, 2000). In these, both the length and angle of branching arteries are incredibly accurate. Vesalius (1514-1564), an anatomist, later provided a detailed drawing of the entire human vascular tree (Fig. 1.1.1).
Fig. 1.1.1: Anatomic drawings by Vesalius. The extensiveness of the vascular tree is well appreciated.
Italian physician Caesalpinus apparently identified the pulmonary circulation and its associated two types of blood vessels: vena cava and pulmonary vein and pulmonary artery and aorta. Hooke (1635-1703; of Hooke’s law of elasticity), an assistant of the English chemist Boyle (1627-1692; of Boyle’s law of gases), recognized that respiration was necessary. But it was the English physiologist Lower (1631-1691) who continued the investigation to show the importance of ventilation-perfusion, i.e. exchange of gases between the lungs and blood. Gas transport in blood was reported by Magnus in 1837. He demonstrated that there was greater oxygen content in arterial blood and greater carbon dioxide content in the venous blood. Other formed elements, such as hemoglobin (Hb) were discovered by Funke in 1851 and has been shown as an important oxygen transporter. Neural effect was shown by Haldane (1860-1936), that carbon dioxide is a normal physiologic stimulus for the respiratory centers. The Haldane effect is now well appreciated in respiratory function and in oxygen therapy applications.
Lack of instrumentation, the measurements of the magnitudes of blood pressure and flow took considerably longer than the interpretation of the circulatory function. Hales in 1733 had incidentally already registered the magnitude of the blood pressure level about which blood oscillates. His initial measurement of blood pressure with a glass tube in a horse has been well illustrated in many publications. Thus, the magnitude of the mean arterial pressure and the amplitude of oscillation, or pulse pressure, were already known at that time. This forms the basis of modern day oscillometric measurement of blood pressure. Hales’ measurements however, did not induce recognition of the great importance of blood pressure magnitude for many decades. We now know that significantly increased magnitudes of mean blood pressure and pulse pressure, the difference between systolic pressure and diastolic pressure, are major contributors to hypertension and many forms of cardiovascular diseases.
The shape of the pressure pulse became known only in the 19th century when Ludwig came up with the kymograph which inscribed blood pressure waveforms. His instrument provided information within a single beat which was a truly a technological advance at the time. Its accuracy was not comparable to present day instrument, although not an issue at the time. Blood pressure recording with the sphygmographs by Marey and his contemporary Mahomed has led to the clinical assessment of arterial diseases, such as hypertension. Incidentally, Chaveau and Marey (1863) also recorded cardiac chamber pressures. Both, shortly later, measured blood flow with an instrument they developed, now known as the bristle flowmeter.
Modern understanding of pressure-flow relationships came with the inventions of fluid-filled catheter-manometer system and the electromagnetic flowmeter. The simultaneous measurements of blood pressure and flow have led to considerable advancement of hemodynamics, or the studies of blood flow. The catheter was introduced in man by Forssmann in 1929, and later advanced for catheterization of the right heart for pressure measurement by Cournand and Range in 1941 (Li et al., 1976). Cournand and Forssmann (together with Richards) shared the Nobel prize for medicine in 1956 for the invention leading to the advancement of modern day catheterization for visualization of blood pressure waveforms in various anatomical sites throughout the circulation. The electromagnetic flowmeter was introduced by Kolin in 1936. But ultrasonic transit-time and Doppler flow velocity probes have taken center stage in modern research and routine clinical measurements, mostly for their noninvasive monitoring capabilities.
In an attempt to understand the function of the arterial system as a whole, Hales (1733) concluded that in order for the arteries to accept the large amount of blood ejected, or the stroke volume, the arteries must behave like a temporary storage reservoir. Since the size of the aorta is considerably smaller than that of the ventricle, the receiving aorta must be elastic in order to perform the function as a reservoir. This interpretation of the reservoir function of arteries became known later as the Windkessel theory which was vigorously pursued a century later by a German physician Frank towards the end of the 19th century. The emphasis on the storage properties of the arteries modeled by Frank as a single elastic tube implied that all pressure fluctuations in the arterial tree should occur synchronously. In other words, the blood pressure pulse should propagate with infinite velocity. The peripheral vessels, on the other hand, are assumed rigid as stiff tubes. This gives rise to the lumped compliance-resistance model of the arterial circulation. This Windkessel model lacks the description of the propagation characteristics of the pressure pulse, but has remained the most popular model describing the arterial system and interpreting its physiological properties even until this day.
Blood pressure pulse propagation with finite wave velocity in a blood vessel was considered over two centuries ago by Euler in 1775. He attempted to develop a formula for its calculation. The well-known physicist Young in 1816, and also the Weber brothers in 1866, apparently solved for the propagation velocity in an elastic tube (Noordergraaf, 1969). Incorporating the elastic properties and geometry of the blood vessel, Moens (1878) and Korteweg (1878) separately developed what is now known as the Moens-Korteweg formula for the pulse wave velocity, or PWV:
where E is, appropriately at the time, defined as the Young’s modulus of elasticity of the blood vessel, h and r are the wall thickness and inner radius of the uniform cylindrical vessel, respectively, and ρ is the density of blood. Pulse propagation velocity is seen to be related to the mechanical and geometrical properties of the blood vessel.
1.2Importance of the Vascular System
In terms of the dynamics of the vascular system, the function of the heart is to provide energy and perfuse organ vascular beds. For the heart to accomplish this efficiently, the vascular system plays a central role as the distributing conduits. As such, both the distributing arteries and the peripheral vascular beds present the load to the pumping heart. Peripheral resistance has been popularly viewed in the clinical setting as the principal vascular load to the heart. This applies mainly to steady flow conditions. This description is naturally inadequate, because of the pulsatile nature of blood flow which remains throughout the microcirculation. Pulsatility implies that there is an oscillatory or pulsatile contribution to the vascular load to the heart. The significance of pulsations has been a popularly debated topic in the clinical settings where perfusion to organs is considered pertinent.
The vascular system provides a seamless illustration of an efficient transport system. This can be seen from the function of, for instances, the coronary circulation in perfusing the heart, the renal circulation in perfusing the kidneys, the cerebral circulation in perfusing the brain and the pulmonary circulation in perfusing the lungs. By virtue of the distributing arterial trees, oxygen, humoral agents, and nutrients be transported to the vital parts of the body, and at the same time, removal of biological waste materials is also accomplished.
1.3Newer Concepts
Modern development of the theory related to blood flow in the vascular system has included multi-faceted aspects, such as, fluid mechanics, fluid-vessel interface, vascular tissue engineering, pulse wave transmission and mathematical modeling.
The mathematical formulations of blood flow through visoelastic arteries have been well established and documented in many texts (e.g. Noordergraaf, 1978, 2011; Li, 1987, 2000, 2004; Nichols and O’Rourke, 1998). These texts also provided experimental measurement methods and quantitative approaches to the assessments of the state of the arterial circulation. There are also several texts in describing the microcirculation and associated biomechanical behavior in greater detail (e.g. Lee and Skalak, 1989; Fung, 1997).
In the application to clinical situations, the interpretation of the morphology of blood pressure and flow waveforms in relation to underlying diseased conditions has attracted the most attention. The introduction of new groups of drugs beyond vasodilators, beta adrenergic blockers, calcium channel blockers and angiotensin-converting enzyme inhibitors that includes local targeted vascular drug delivery, as well as the introduction of gene therapy and regenerative medicine, to improve vascular perfusion and in the treatment of diseases, has become more avant garde.
Not only the arteries, the microcirculatory vessels are no longer viewed merely as resistance vessels, but are compliant with viscoelastic properties that vary with frequency. The classical elastic description of blood vessels has been modified to include viscosities of the blood and the vessel wall. The viscosities give rise to energy dissipation. Thus, the energy utilization and dissipation in relation to blood flow is now considered pertinent. Regarding Chi, or energy, the amount of the work that the heart has to generate during each beat has generated considerable attention. This included the steady energy dissipation through peripheral resistance vessels in different parts of the body, as well as energy required to overcome pulsations which persist even in the microcirculation.
Clinical applications of modern development of dynamics of the vascular system have initiated both invasive and noninvasive technological development and improvement in the accuracy of assessing the vascular structure and function. These include laser-Doppler velocimeter, multi-sensor pressure-velocity catheter, phase contrast magnetic resonance imaging (PC-MRI) and intravascular ultrasonic system (IVUS). There are also advancements in the development of interventional devices, such as local drug delivery catheter, laser- or balloon-angioplasty catheter, vascular stents and grafts. Many of these have been used for the assessment and treatment of vascular hypertrophy, stenosis and aneurysm, hypertension and atherosclerosis.
1.4Book Contents
This book deals primarily with the dynamic behavior of the components of the vascular system and methods and techniques for their quantitative measurements. The book is written applying fundamental physical principles in conjunction with physiological measurements to the analysis of the structural and functional aspects of the vascular tree that includes the arterial circulation, the venous circulation, and the microcirculation, inclusive of arterioles, c...