eBook - ePub
Orthodontic Functional Appliances
Theory and Practice
Padhraig S. Fleming, Robert T. Lee, Padhraig S. Fleming, Robert T. Lee
This is a test
Buch teilen
- English
- ePUB (handyfreundlich)
- Über iOS und Android verfügbar
eBook - ePub
Orthodontic Functional Appliances
Theory and Practice
Padhraig S. Fleming, Robert T. Lee, Padhraig S. Fleming, Robert T. Lee
Angaben zum Buch
Buchvorschau
Inhaltsverzeichnis
Quellenangaben
Über dieses Buch
Comprehensive specialist manual covering the science and practice of functional appliance therapy
- Integrates clinical and academic elements with emphasis on evidence-based research and its clinical application
- Suitable for trainee and practicing orthodontists
- Includes more than 600 photographs to enhance clarity of topics covered
- Features contributions from top clinicians and researchers in the field
Häufig gestellte Fragen
Wie kann ich mein Abo kündigen?
Gehe einfach zum Kontobereich in den Einstellungen und klicke auf „Abo kündigen“ – ganz einfach. Nachdem du gekündigt hast, bleibt deine Mitgliedschaft für den verbleibenden Abozeitraum, den du bereits bezahlt hast, aktiv. Mehr Informationen hier.
(Wie) Kann ich Bücher herunterladen?
Derzeit stehen all unsere auf Mobilgeräte reagierenden ePub-Bücher zum Download über die App zur Verfügung. Die meisten unserer PDFs stehen ebenfalls zum Download bereit; wir arbeiten daran, auch die übrigen PDFs zum Download anzubieten, bei denen dies aktuell noch nicht möglich ist. Weitere Informationen hier.
Welcher Unterschied besteht bei den Preisen zwischen den Aboplänen?
Mit beiden Aboplänen erhältst du vollen Zugang zur Bibliothek und allen Funktionen von Perlego. Die einzigen Unterschiede bestehen im Preis und dem Abozeitraum: Mit dem Jahresabo sparst du auf 12 Monate gerechnet im Vergleich zum Monatsabo rund 30 %.
Was ist Perlego?
Wir sind ein Online-Abodienst für Lehrbücher, bei dem du für weniger als den Preis eines einzelnen Buches pro Monat Zugang zu einer ganzen Online-Bibliothek erhältst. Mit über 1 Million Büchern zu über 1.000 verschiedenen Themen haben wir bestimmt alles, was du brauchst! Weitere Informationen hier.
Unterstützt Perlego Text-zu-Sprache?
Achte auf das Symbol zum Vorlesen in deinem nächsten Buch, um zu sehen, ob du es dir auch anhören kannst. Bei diesem Tool wird dir Text laut vorgelesen, wobei der Text beim Vorlesen auch grafisch hervorgehoben wird. Du kannst das Vorlesen jederzeit anhalten, beschleunigen und verlangsamen. Weitere Informationen hier.
Ist Orthodontic Functional Appliances als Online-PDF/ePub verfügbar?
Ja, du hast Zugang zu Orthodontic Functional Appliances von Padhraig S. Fleming, Robert T. Lee, Padhraig S. Fleming, Robert T. Lee im PDF- und/oder ePub-Format sowie zu anderen beliebten Büchern aus Medicine & Orthodontics. Aus unserem Katalog stehen dir über 1 Million Bücher zur Verfügung.
Information
CHAPTER 1
Biological basis for functional appliance therapy
A functional appliance is one that uses the facial muscles and masticatory muscles to produce changes in the position of the individual teeth or arches. Any oral appliance causing a change in the forces of occlusion and alteration in muscular activity is likely to produce displacement of individual teeth or arches. Therefore such appliances can be either removable, inducing a displacement of the mandible by a process of interference or by stimulating an avoidance reflex, or fixed, involving the use of a mechanism causing the mandible to be held in a different position for function.
Facial growth
Maxillary growth occurs primarily by intra-membranous ossification with surface remodelling, resulting in a downward–forward displacement of the maxilla at an angle of approximately 40 degrees to the cranial base.1 Growth of the maxilla is complex and may be affected by alterations in the sutures of the maxillae. Resorption on the superior surface and the apposition of bone on other surfaces affect the position of the maxillary dento-alveolar complex, with resorption of the anterior surface being typical during the downward–forward growth of the basal bone. However, while apposition of bone occurs on the inferior surface of the palate, resorption occurs on the superior surface, resulting in a net downward displacement (Figure 1.1).
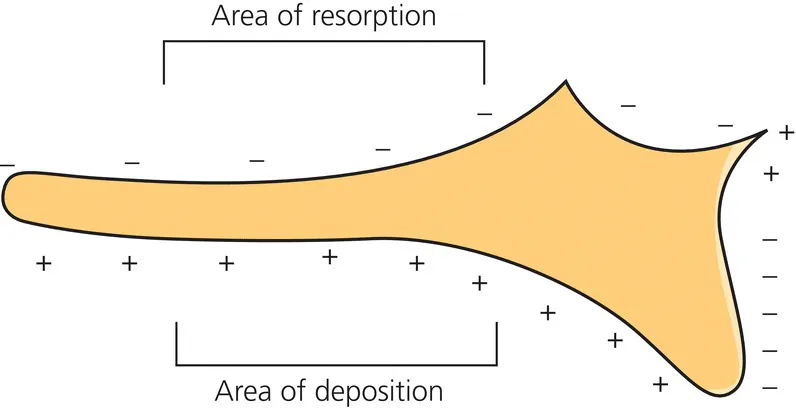
Figure 1.1 Resorption on the superior surface of the maxilla accompanied by deposition on the palate surface leads to an inferior displacement.
Björk and Skieller’s tantalum implant studies have shown that mandibular growth in children and adolescents occurs mainly as a consequence of an increase in condylar length in a posterior and superior direction due to endochondral ossification.2 Elsewhere mandibular growth is a product of surface apposition and remodelling. Appositional growth does not occur anteriorly at the chin, with chin growth being expressed chiefly at the lateral aspects. Mandibular growth otherwise manifests as remodelling of the alveolus and of the bony areas with muscular attachments. Growth of the ascending ramus primarily occurs posteriorly, with resorption on the anterior aspect (Figure 1.2).
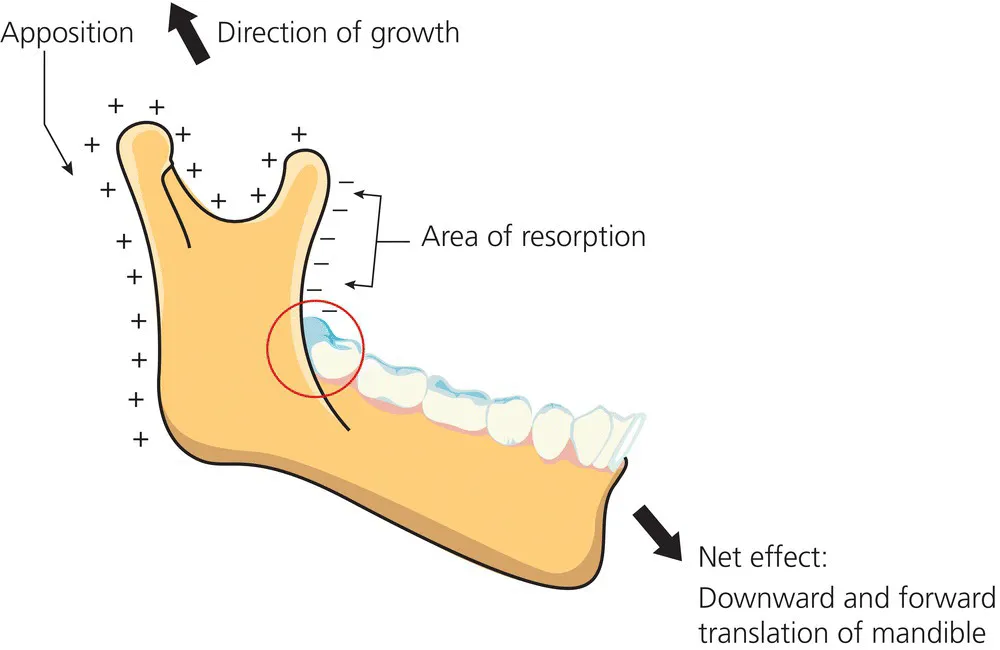
Figure 1.2 Mandibular growth occurs via condylar growth in a posterior and superior direction resulting in downward and forward displacement. Resorption on the anterior surface of the ascending ramus combined with resorption on the posterior surface leads to forward movement of the ramus.
The mandible is not directly attached to the skull, but rather held in position by the muscles, ligaments and tendons, with the condylar head of the mandible being placed in the glenoid fossa within the temporal bone. The synovial articulation between the condyle and the temporal bone is classified as a ginglymoarthroidal joint, as both a ginglymus (hinging) and arthroidal (sliding) element exist, permitting the required mandibular opening and excursive movements during function. Changes in the position of the glenoid fossae will have consequent effects on the position of the mandible.
Orthodontic therapy involving functional appliances therefore might be expected to produce changes in the position of both the maxilla and the mandible, and combinations of growth restraint and growth induction would result in clinical changes in three dimensions. Detailed information on facial growth has been presented by Enlow1 and Björk and Skieller.2
While increases in the absolute mandibular dimensions outstrip those of the maxilla during adolescence, this does not normally result in occlusal improvement in Class II malocclusion without active orthodontic intervention.3 Based on longitudinal data from growth studies, some straightening of the profile and reduction in facial convexity may occur during the pubertal growth phase,4 although this has not been a universal finding5 and little change in the skeletal profile occurs in late adolescence.6 Foley and Mamandras7 noted that twice as much mandibular as maxillary growth arose in Class II males and females from 14 to 20 years old based on a North American Caucasian sample. However, a greater increase in absolute mandibular length is to be expected, as its overall dimension is greater than that of the maxilla, with the percentage difference in the increase between mandibular and maxillary less significant; mandibular length also incorporates a profound vertical element, while maxillary growth is usually measured from ANS (anterior nasal spine) to PNS (posterior nasal spine) and is therefore essentially horizontal. Positive occlusal interdigitation may also limit changes in inter-arch relationships. Moreover, in an analysis of patients with skeletal 2 patterns aged 8 to 18 years and increased overjet who had no orthodontic treatment, 4 mm more forward growth of the mandible than the maxilla was observed, but the occlusion and overjet remained unchanged into adulthood; this lack of change was attributed to the cuspal interdigitation.8
The rate of craniofacial growth, particularly of the maxilla and the mandible, is believed to undergo a pre-pubertal peak. The rate of growth is generally limited prior to this period, although a transient juvenile peak in growth rate has been described in females. Riolo et al.9 described an annual rate of increase in the length of the mandibular body (Gonion–Pogonion) of 1.7 mm and 2.5 mm, respectively, in 8-year-old males and females. The corresponding figures at 13 years were 2 mm and 1.8 mm. Intuitively, therefore, treatment involving growth modification is ideally timed during a period of maximal growth. However, while this sounds relatively simple, a range of techniques directed at timing treatment have been developed and trialled, with limited success (Chapter 4). For example, while the rate of mandibular growth is thought to mirror increases in statural height, there is significant variation.10
Arbitrary use of chronological age, typically 10 to 13 years in females and 11 to 14 years in males, continues to be an accepted method of estimating the timing of most efficient and effective growth modification in Class II subjects. However, little difference has been demonstrated in the relative skeletal effectiveness of functional appliances in subjects of mean age 10 years relative to a group treated just after the onset of puberty (mean age 12 years 11 months).11 Moreover, Pancherz et al., who in earlier research highlighted an increase in condylar growth rate in harmony with increases in statural height,12 have since reported on the use of the Herbst appliance in skeletally mature patients with demonstrable, albeit limited, skeletal changes based on magnetic resonance imaging of the temporo-mandibular joints.13
Function and craniofacial morphology
Craniofacial growth is believed to be capable of a certain degree of morphological adaptation subject to functional requirements, with function known to be required for normal homeostasis and cellular turnover.14 This theory is based on the work of Van der Klaauw, subsequently popularized by the American anatomist Melvin Moss.15 According to the functional matrix theory, facial growth, final shape and dimensions are governed by the role of resident organs and tissues, specifically the senses, and essential functions including eating, cognition and breathing. Moss believed that the properties of important organs were related to underlying skeletal components. In particular, two major functional elements (cerebral and facial) were described with unique tissues and spaces. Moss hypothesized that expansion of each capsular matrix was accompanied and facilitated by bone growth via endochondral and intra-membranous ossification to preserve functional spaces. These hypotheses were supported by experimental evidence demonstrating altered skeletal growth following separation from soft tissue elements, while the presence of enveloping soft tissues led to the observation of normal growth patterns. Applying Moss’s concepts to the potential for modification of growth with functional appliance therapy, it could be argued that postural changes with associated soft tissue alteration may be accompanied by a redirection or indeed acceleration of skeletal growth. Moreover, correction of abnormal soft tissue patterns and behaviour was a tenet for the pioneers of functional appliance therapy, many of whom advocated its use to restore normal function and development. Moreover, in animal models altered masticatory function and associated changes in muscular loading have been shown to affect condylar cartilage thickness and chondroblast differentiation.16, 17
The malleability of cranial shape following the application of continuous forces during the process of cerebral growth and skull development has been demonstrated in tribal groups. This is apparent in the skulls of indigenous people in South America, where the bandaging of the skull from shortly after birth resulted in significant alteration in the shape of the cranium (Figure 1.3). It would appear that the overall size of the brain has been maintained while the shape of the supporting cranium is significantly altered. Similarly, dramatic changes have been observed in long bones and as a result of other local practices including foot binding, which reduces foot size to an extent by repositioning the bony elements.

Figure 1.3 An example of the effects of cranial binding in a South American female from the Atacama desert. Typically, binding is undertaken for a relatively short period (approximately 6 months) in infancy; the effects are marked and persist into adulthood.
Orthodontists involved in changing the facial shape of those with malocclusion would wish to alter similarly the directional growth of the mandible in relation to the maxilla. Positional change in these relationships could be sufficient to correct sagittal, vertical and transverse occlusal discrepancies. It has been recognized that skeletal II discrepancies are primarily related to the position of the mandible relative to the maxilla rather than the overall size of the underlying bones (Figure 1.4).18–20 McNamara, in an analysis of...