To provide person-centred care (PCC) for any patient or client means that they are included in decision making about their care. PCC in the older person cannot be successful unless the ethos of the wider MDT is one of a shared partnership with each other and the patient.
In order for PCC to be effective for all concerned, nurses involved in caring for the older person need to be aware of a number of factors. This involves not only looking at the needs of the patient and considering their definition of satisfaction, but also, fundamentally, staff considering their understanding of older people and PCC itself.
It is important that nurses have an awareness of their own attitudes regarding older people. The media often portrays older people as being dependant on others and it is inevitable that this will have an unconscious effect on our attitude (Koskinen et al., 2014) and affect our interpersonal skills that are fundamental to effective PCC. In not acknowledging the diversity of the older population, in terms of their ability and capacity, we are reducing them to a homogeneous group incapable of being asked about or making decisions of their own, for themselves (Phelan, 2011). By becoming aware of culturally influenced attitudes about the older person and how these outlooks are mirrored in the ways older people are observed, treated and cared for in society, the nurse and the MDT can better understand the premise from which to provide high-quality PCC.
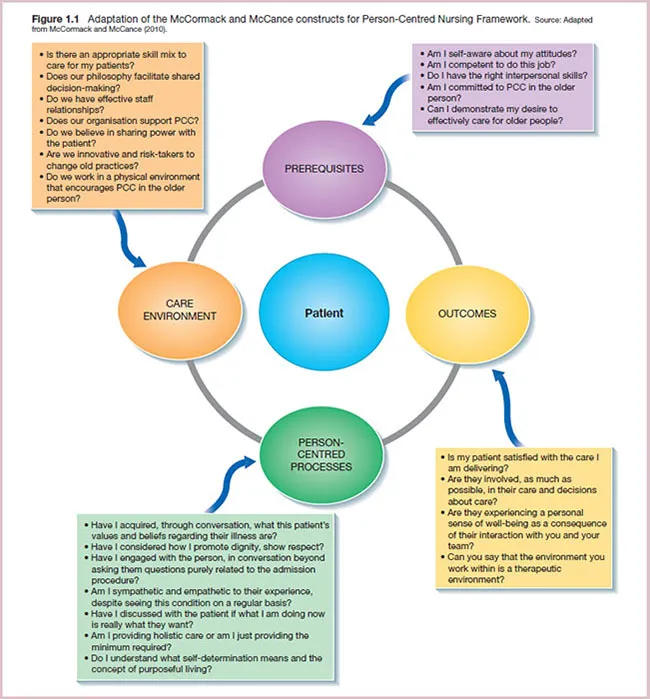
McCormack and McCance (2010) developed a ‘Person-Centred Nursing Framework’ and this framework has four constructs that are fundamental to delivering PCC in the older person effectively. They are:
- Prerequisites
- The care environment
- Person-centred processes
- Outcomes.
These constructs are presented in Figure 1.1 with examples of the questions the nurse might consider when delivering PCC in the older person.
Having taken into consideration the constructs above as fundamental to delivering effective PCC, the nurse, due to cultural differences, also needs to appreciate those intrinsic factors that will affect what can be called the ‘intergenerational conversation’ that occurs between the patient and nurse.
Bochner (2013) asserted that intersubjective values such as power, hierarchy, status, subordination and perceptions of equality affect intergenerational conversation more than previously imagined. Bochner emphasises that any contact between professional and patient can affect the communication and behaviour of both parties due to the interaction being a heavily differing value-oriented encounter. Intergenerational communication does not just include the entire range of communication skills across boundaries of age groups but also takes into account gender and cultural factors.
An awareness of these factors is important if the patient is going to be comfortable to express their needs and for the nurse–patient relationship to be mutually beneficial. It is important for the nurse to be aware of the intergenerational implications of both verbal and non-verbal aspects of conversing with those who are of a different age group, and perhaps, feeling vulnerable in a care setting. As mentioned at the beginning of this chapter, it is essential that the nurse be aware of his or her own socialised prejudices or prejudgements that may affect their interpersonal behaviour. Both these traits affect the tone and values of conversation that follows, in which the patient comes to recognise the identity that the nurse is now giving them, be it positively or negatively (Samovar et al., 2013).
The notion of PCC is complex and multi-dimensional. For it to be successful, the MDT needs to work at sustaining a reflective and honest planned culture change, which is necessary to embed the values of PCC of older people in daily practices. Good nurse leadership and the care environment are key influencing factors on the way that person-centredness is experienced by patients, their families and the MDT. For PCC to be experienced in a consistent and continuous way by these patients, the culture of practice has to support a compassionate, humanistic and creative way of practising, that enables care teams to flourish or achieve patient satisfaction. In adopting this change in culture, ultimately, the nurse is working towards promoting those notions around self-determination and purposeful living, often taken for granted when we are young.
References
- Bochner, S. (2013) Cultures in Contact: Studies in Cross-Cultural Interaction. Oxford: Pergamon Press.
- Koskinen, S., Salminen, L. and Leino-Kilpi, H. (2014) Media portrayal of older people as illustrated in Finnish newspapers. International Journal of Qualitative Studies on Health and Well-being. doi: 10.3402/qhw.v9.25304.
- McCormack, B. and McCance, T. (2010) Person-Centred Nursing: Theory, Models and Methods. Oxford: Blackwell Publishing.
- Phelan, A. (2011) Socially constructing older people: Examining discourses which can shape nurses’ understanding and practice. Journal of Advanced Nursing 67: 893–903.
- Samovar, L.A., Porter, R.E. and McDaniel, E.R. (2013) Intercultural Communication: A Reader, 11th edn. London: Thompson Learning.