eBook - ePub
Clinical Skills for Nursing Adults
Step by Step
Wendy Wright,Paul Newcombe,Fiona Everett
This is a test
- 176 pages
- English
- ePUB (adapté aux mobiles)
- Disponible sur iOS et Android
eBook - ePub
Clinical Skills for Nursing Adults
Step by Step
Wendy Wright,Paul Newcombe,Fiona Everett
Détails du livre
Aperçu du livre
Table des matières
Citations
À propos de ce livre
This pocket-sized book provides step-by-step instructions on how to carry outadvancedclinical skills such as medicine administration, giving transfusions, catheterisation, and other key skills across both acute and community settings. It is ideal forsecond and third year students and has been updatedforthe2018 NMC standards, including themost up-to-date evidencebase for the procedures. Each section features:
- Handy checklists detailing the essential equipment and things to consider before starting.
- Helpful tips and advice on what to watch out for and the relevant action to take for each skill.
- Care setting considerationsexploring patient requirements depending on where care is being given.
- Clear instructions guiding you step by step through each procedure.
Whether you are revising, practicing, or preparing for a clinical placement, this book will become a trusted companion and daily reference that will help to develop and improve your nursing skills.
Foire aux questions
Comment puis-je résilier mon abonnement ?
Il vous suffit de vous rendre dans la section compte dans paramètres et de cliquer sur « Résilier l’abonnement ». C’est aussi simple que cela ! Une fois que vous aurez résilié votre abonnement, il restera actif pour le reste de la période pour laquelle vous avez payé. Découvrez-en plus ici.
Puis-je / comment puis-je télécharger des livres ?
Pour le moment, tous nos livres en format ePub adaptés aux mobiles peuvent être téléchargés via l’application. La plupart de nos PDF sont également disponibles en téléchargement et les autres seront téléchargeables très prochainement. Découvrez-en plus ici.
Quelle est la différence entre les formules tarifaires ?
Les deux abonnements vous donnent un accès complet à la bibliothèque et à toutes les fonctionnalités de Perlego. Les seules différences sont les tarifs ainsi que la période d’abonnement : avec l’abonnement annuel, vous économiserez environ 30 % par rapport à 12 mois d’abonnement mensuel.
Qu’est-ce que Perlego ?
Nous sommes un service d’abonnement à des ouvrages universitaires en ligne, où vous pouvez accéder à toute une bibliothèque pour un prix inférieur à celui d’un seul livre par mois. Avec plus d’un million de livres sur plus de 1 000 sujets, nous avons ce qu’il vous faut ! Découvrez-en plus ici.
Prenez-vous en charge la synthèse vocale ?
Recherchez le symbole Écouter sur votre prochain livre pour voir si vous pouvez l’écouter. L’outil Écouter lit le texte à haute voix pour vous, en surlignant le passage qui est en cours de lecture. Vous pouvez le mettre sur pause, l’accélérer ou le ralentir. Découvrez-en plus ici.
Est-ce que Clinical Skills for Nursing Adults est un PDF/ePUB en ligne ?
Oui, vous pouvez accéder à Clinical Skills for Nursing Adults par Wendy Wright,Paul Newcombe,Fiona Everett en format PDF et/ou ePUB ainsi qu’à d’autres livres populaires dans Medizin et Pflegefähigkeiten. Nous disposons de plus d’un million d’ouvrages à découvrir dans notre catalogue.
Informations
Appendix 1 Blood Collection Needles
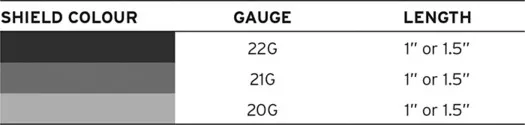
BD Vacutainer® needles are available with a 20, 21 or 22 gauge needle.
The higher the gauge, the narrower the diameter of the needle.
Colours are universal and can be applied to other vacutainer systems used in practice.
Appendix 2 Fluid Status Assessment
Patients requiring IV fluids should have a fluid or hydration assessment by senior medical or nursing staff at least once per 24 hours. Along with a physical examination, NICE (2013) recommends that their urea and electrolytes are checked daily.
Fluid status can be broadly categorised as euvolaemic (normal fluid status), hypovolaemic (dehydrated) and hypervolaemic (overloaded).
Euvolaemia: Patients with normal fluid status who are well hydrated and have no abnormal fluid losses.
Hypovolaemia: Also known as dehydration, hypovolaemic patients have too little circulating blood volume. The two broad causes of hypovolaemia are:
- output too high: losing too much fluid, e.g. diarrhoea
- input too low: inadequate fluid intake, e.g. swallowing difficulties.
Hypervolaemia: Commonly known as ‘overload’, patients experiencing hypervolaemia have too much fluid in their circulating volume. The two broad causes of hypervolaemia are:
- output too low: unable to make enough urine, e.g. chronic kidney disease
- input too high for body’s ability to handle the fluid, e.g. advanced heart failure.
Indications for IV fluids
Drinking is usually the preferred route for fluid intake; however, sometimes fluids require to be administered intravenously. The three main reasons for IV fluid administration are:
- routine maintenance
- replacement of fluid loss
- resuscitation.
Routine maintenance is for patients who are unable to meet their intake requirements orally. Adults require a routine fluid intake of 25–30 ml/kg/24 hours. Older or frail adults require less at 20–25 ml/kg/24 hours (NICE, 2013). Patients with hepatic, renal or cardiac impairment will have different requirements and should have their intake goals set and reviewed by senior medical staff.
Patients who are nil by mouth should be considered for routine maintenance if they are expected to be nil by mouth for longer than 8 hours.
Replacement fluids are given in addition to maintenance fluids to patients who have experienced either recent or ongoing fluid loss, e.g. high output stoma, vomiting and diarrhoea.
Resuscitation fluids are given in emergencies when rapid fluid administration is required to preserve the patient’s circulatory system, e.g. major haemorrhage.
Fluid Types
There are two types of IV fluids: crystalloids and colloids. Crystalloids consist of small molecules, which means that the fluid can leak out of the blood vessels into the surrounding tissues. Colloids have larger molecules that cannot leave the blood vessels so easily, which theoretically means that a smaller volume of infusion is required compared to crystalloid.
There is a move away from sodium chloride 0.9% towards increased use of balanced crystalloids, e.g. Hartmann’s solution. The contents of balanced crystalloids more closely resemble blood plasma than crystalloids such as sodium chloride 0.9% or glucose 5%.
Appendix 3 Intake/Output Charts
Traditionally known as fluid balance charts, the main purpose of these charts is the assessment of intake and output rather than just overall fluid balance. For example, a patient who has an intake of 400 ml and output of 400 ml in 24 hours has both an inadequate fluid intake and output but would have a neutral fluid balance.
- Identify people who would benefit from intake/output monitoring

- Ensuring only patients who require intake/output monitoring have charts completed means that time is not wasted on unnecessary charting.
- Patients who may need intake/output monitoring include the following:
- acutely ill or deteriorating:
- sepsis
- NEWS of greater than or equal to 5
- up to 48 hours post-discharge from Critical Care
- at risk of dehydration:
- temperature greater than or equal to 38°C
- frequent vomiting/high nasogastric aspirate
- diarrhoea
- high output stoma
- large open wound/vacuum-assisted therapy
- urine output <0.5 ml/kg/hours
- requires assistance to eat or drink
- nil by mouth for more than 8 hours
- receiving intravenous or enteral fluids
- requiring a fluid restriction
- part of routine post-operative management
- urinary catheter in place (acute setting)
- acute kidney injury.
- acutely ill or deteriorating:
- Please note this is not an exhaustive list and does not replace clinical judgement.
- Document the reason for commencing an intake/output chart in the nursing notes.
- Setting a fluid intake goal

- It is important to set a fluid intake goal so that the whole team, the patient and their families know what the aim is for the day and whether or not it is being achieved. Without a goal it can be difficult to realise promptly when a person doesn’t have a sufficient intake.
- NICE (2013) recommends that a person should have a total intake of 25–30 ml/kg/24 hours in the absence of any significant comorbidities. This volume is reduced to 20–25 ml/kg/24 hours for older and frail people.
- People with comorbidities such as cardiac failure, renal failure, head injury, etc. are likely to have different fluid requirements which must be assessed and set by senior medical staff.
- Remember that included in the total intake along with any oral intake are drug infusions, enteral feeding and total parenteral nutrition.
- Some patients require a fluid restriction due to comorbidities such as advanced heart failure or end stage kidney disease. As far as possible such restrictions should be managed in partnership with the patient and monitored throughout the day to ensure that their fluid restriction is well managed.
- The intake goal should be agreed with medical staff.
- It is important to set a fluid intake goal so that the whole team, the patient and their families know what the aim is for the day and whether or not it is being achieved. Without a goal it can be difficult to realise promptly when a person doesn’t have a sufficient intake.
- Know what you are recording on the intake/output chart

- As a general rule only beverages and soup are counted as oral intake. Enteral feeding and all IV therapy must also be documented on the chart.
- Check local policy about what is included on the intake/output chart to ensure consistency.
- Remember to document the drinks when patients are taking their medications!
- IV fluids should be documented either hourly or retrospectively at the end of every bag as per local policy.
- For patients who are set a fluid restriction, fluid intake may be more carefully documented and include items such as ice cream, yoghurt and custard.
- Remember that if the patient isn’t able to take large drinks but is wetting their mouth, this should be documented to ensure drinks continue to be offered and to highlight low intake rather than a potentially uncompleted chart.
- Documenting output

- Urinary output should be at least 0.5 ml/kg/hour.
- Please adhere to local policy relating to measurement of urinary output for patients experiencing incontinence.
- Other losses must also be documented accurately as close to the time of measurement as possible. Such losses may include drain or stoma outputs, vomiting, diarrhoea and nasogastric aspirate.
- Identifying patients at risk

- Intake/output charts must be totalled at least every 6 hours to allow continuous monitoring of fluid status and early detection of problems.
Totalling should take advantage of existing work patterns, e.g. before the ward doctor’s handover to the out-of-hours team, or before the day shift handover to the night shift, to help ensure prompt identification and resolution of issues.
Appendix 4 ECG Interpretation
Heart rate
To calculate the heart rate from a rhythm strip printed on ECG paper:
- Count the large squares between the peak of one R wave and the peak of the next R wave and then divide...
Table des matières
- Cover
- Half Title
- Publisher Note
- Title Page
- Copyright Page
- Contents
- Common Abbreviations
- Useful Prefixes And Suffixes
- Introduction and General Considerations
- Basic Airway Management
- Advanced Airway Management
- Lung Sounds
- Oxygen Therapy
- Nebulisers
- Venepuncture
- Peripheral IV cannulation
- Intravenous Fluids
- Blood transfusion
- Central Venous Access Devices
- ECG
- Resuscitation
- Neurological Examination
- Medicines Administration
- Bowel Sounds
- Gastric Aspiration
- Enteral Feeding
- Removal of Sutures and Staples
- Urinary Catheterisation
- Urinalysis Interpretation
- Sepsis
- Appendix 1 Blood Collection Needles
- Appendix 2 Fluid Status Assessment
- Appendix 3 Intake/Output Charts
- Appendix 4 ECG Interpretation
- References
Normes de citation pour Clinical Skills for Nursing Adults
APA 6 Citation
Wright, W., Newcombe, P., & Everett, F. (2019). Clinical Skills for Nursing Adults (1st ed.). SAGE Publications. Retrieved from https://www.perlego.com/book/3013343/clinical-skills-for-nursing-adults-step-by-step-pdf (Original work published 2019)
Chicago Citation
Wright, Wendy, Paul Newcombe, and Fiona Everett. (2019) 2019. Clinical Skills for Nursing Adults. 1st ed. SAGE Publications. https://www.perlego.com/book/3013343/clinical-skills-for-nursing-adults-step-by-step-pdf.
Harvard Citation
Wright, W., Newcombe, P. and Everett, F. (2019) Clinical Skills for Nursing Adults. 1st edn. SAGE Publications. Available at: https://www.perlego.com/book/3013343/clinical-skills-for-nursing-adults-step-by-step-pdf (Accessed: 15 October 2022).
MLA 7 Citation
Wright, Wendy, Paul Newcombe, and Fiona Everett. Clinical Skills for Nursing Adults. 1st ed. SAGE Publications, 2019. Web. 15 Oct. 2022.