eBook - ePub
Inflammatory Mechanisms in Asthma
Stephen Holgate, Stephen Holgate
This is a test
- 1,090 pagine
- English
- ePUB (disponibile sull'app)
- Disponibile su iOS e Android
eBook - ePub
Inflammatory Mechanisms in Asthma
Stephen Holgate, Stephen Holgate
Dettagli del libro
Anteprima del libro
Indice dei contenuti
Citazioni
Informazioni sul libro
This timely volume brings together the latest basic and clinical insights on the cellular and mediator mechanisms involved in the induction and persistence of airway dysfunction of asthma by over 90 experts in the field-paving the way for developing novel and more effective antiinflammatory therapeutic agents and strategies.
Furnishing a comprehensive and up-to-date view of the expanding and interrelated components underlying asthma pathogenesis, Inflammatory Mechanisms in Asthma
- describes how evidence on airway inflammation is obtained with invasive and noninvasive procedures, such as bronchoalveolar lavage and sputum analysis
- reviews the complex interactions of inflammatory cells that contribute to chronic inflammation and bronchial hyperreactivity, including eosinophils, basophils, neutrophils, fibroblasts, epithelial cells, and macrophages
- considers mast cells, cytokines, neural factors, leukotrienes, kinins, and other mediators that regulate the development, establishment, or resolution of asthma exacerbations
- presents new information suggesting that airway changes in asthma can lead to remodeling or airway fibrosis
- and more!
Enhanced with over 4700 references, tables, drawings, and photographs, this compelling investigation into the pathophysiology of asthma is an indispensable resource for pulmonologists, physiologists, immunologists, allergists, epidemiologists, biochemists, molecular biologists, and graduate and medical school students in these disciplines.
Domande frequenti
Come faccio ad annullare l'abbonamento?
È semplicissimo: basta accedere alla sezione Account nelle Impostazioni e cliccare su "Annulla abbonamento". Dopo la cancellazione, l'abbonamento rimarrà attivo per il periodo rimanente già pagato. Per maggiori informazioni, clicca qui
È possibile scaricare libri? Se sì, come?
Al momento è possibile scaricare tramite l'app tutti i nostri libri ePub mobile-friendly. Anche la maggior parte dei nostri PDF è scaricabile e stiamo lavorando per rendere disponibile quanto prima il download di tutti gli altri file. Per maggiori informazioni, clicca qui
Che differenza c'è tra i piani?
Entrambi i piani ti danno accesso illimitato alla libreria e a tutte le funzionalità di Perlego. Le uniche differenze sono il prezzo e il periodo di abbonamento: con il piano annuale risparmierai circa il 30% rispetto a 12 rate con quello mensile.
Cos'è Perlego?
Perlego è un servizio di abbonamento a testi accademici, che ti permette di accedere a un'intera libreria online a un prezzo inferiore rispetto a quello che pagheresti per acquistare un singolo libro al mese. Con oltre 1 milione di testi suddivisi in più di 1.000 categorie, troverai sicuramente ciò che fa per te! Per maggiori informazioni, clicca qui.
Perlego supporta la sintesi vocale?
Cerca l'icona Sintesi vocale nel prossimo libro che leggerai per verificare se è possibile riprodurre l'audio. Questo strumento permette di leggere il testo a voce alta, evidenziandolo man mano che la lettura procede. Puoi aumentare o diminuire la velocità della sintesi vocale, oppure sospendere la riproduzione. Per maggiori informazioni, clicca qui.
Inflammatory Mechanisms in Asthma è disponibile online in formato PDF/ePub?
Sì, puoi accedere a Inflammatory Mechanisms in Asthma di Stephen Holgate, Stephen Holgate in formato PDF e/o ePub, così come ad altri libri molto apprezzati nelle sezioni relative a Medizin e Lungenheilkunde & Thoraxmedizin. Scopri oltre 1 milione di libri disponibili nel nostro catalogo.
Informazioni
1
The Pathology of Fatal Asthma
Sir Charles Gairdner Hospital
Nedlands, Western Australia
I. | Introduction |
Descriptions of the macroscopic findings in the lungs of individuals with fatal asthma date back as far as the seventeenth century. In 1883 spirals of mucus occluding airways in such cases were described by Curschmann (1). In their comprehensive review of asthma pathological characteristics and mechanisms, Huber and Koessler (2) in 1922 identified 15 cases in which the microscopic findings in fatal asthma had been described and added 5 cases of their own. In the first quantitative study of asthma pathological features, they compared these cases to a nonasthmatic group using a stratified technique of sampling large and small airways and even considered the confounding effects of muscle spasm on measured airway dimensions. They documented the classic pathological findings in fatal asthma, including overinflated lungs, mucus plugs occluding airway lumens and containing shed epithelial cells and Charcot-Leyden crystals, variable epithelial damage, dilated mucus gland ducts, thickening of the “basement membrane,” infiltration of round cells and eosinophils into the airway wall, and greater thickness of the epithelium, smooth muscle, and airway wall compared to those of nonasthmatics.
A number of qualitative studies (3,4,5,6,7,8,9,10,11,12), including over 550 cases of fatal asthma with postmortem findings, have since been reported and confirm the pathological abnormalities described. Descriptions from the first half of this century have also reported the presence of peripheral edema, right ventricular hypertrophy, emphysema, atelectasis, bacterial and tuberculous infection, and bronchiectasis. Some of these changes probably reflect long-standing severe airway obstruction, the lack of antibiotics and corticosteroids, and the unrecognized effects of smoking cigarettes. Gough (13) showed that although the lungs were hyperinflated in cases of fatal asthma, emphysema, characterized by destuction of alveolar walls, was not present.
The precise definition of subdivisions of the bronchial wall is confounded by the lack of uniformity among groups of anatomists, pathologists, and physiologists (14). For the purposes of this review the airway will be partitioned as follows: the lumen, which includes the mucus layer; the epithelium (or mucosa); the submucosa, which includes all structures bound by the subepithelial basement membrane and the smooth muscle; and the adventitia, which includes structures between the smooth muscle and the outer limit of the loose connective tissue surrounding the airway.
II. | Lumen |
Plugging of airway lumens with tenacious mucus is an almost constant macroscopic and microscopic finding at autopsy in cases of fatal asthma and may extend from the central airways (Fig. 1a–c) to the small airways (Fig. 1d) as far as the respiratory bronchioles (2,3,4,5,6,7,8,9,15,16,17,18,19,20). Cases in which mucus is not found in the airways are rare (15,21). The mucus plugs in fatal asthma contain shed epithelial cells, inflammatory cells, and proteinacious exudate (Fig. 1). The formation of Charcot-Leyden crystals from the degeneration of eosinophils and the presence of lamellae (Fig. 1c) in the mucus (22) suggest that the mucus accumulates over a period of time. Sudden attacks of asthma, severe enough to require intubation, can occur in the absence of intraluminal mucus (23). These episodes are presumably due to excessive airway smooth muscle shortening. It has been estimated that a single outpouring of mucus gland contents is unlikely to cause significant airway obstruction in the absence of any airway smooth muscle shortening (24). Therefore it is likely that pooling of mucus or gradual accumulation of mucus in the airway lumen would be necessary to cause significant airway narrowing. Shortening of the airway smooth muscle greatly exaggerates the effect of intraluminal mucus in causing airway narrowing (24).
Mucus is produced by the goblet cells of the epithelium and by the mucus glands in the deeper layers of the airway wall. The number of goblet cells and the area of mucus glands are increased above normal in cases of fatal asthma (5,25). Aikawa and colleagues (25) found that the degree of mucus plugging of the airway lumen and the number of goblet cells were greater in patients dying of acute, severe attacks of asthma than in those dying of asthma after a long period of hospital admission. The amount of mucus plugging was related to the area of goblet cells within the airway epithelium, but the area of airway wall mucus gland tissue was similar in both groups. The relative contribution of goblet cells and mucus glands to the mucus in the airway lumen is difficult to assess from such studies because the rate and volume of mucus production from these two sources in patients with asthma are poorly understood.
The mucus in cases of fatal asthma is characteristically thick and tenacious, protruding from the cut surface of the lung at postmortem. This property has been attributed to abnormal mucins of high molecular weight, which are not found in normal individuals or in individuals who have cystic fibrosis (26). The mucus does not seem to derive its physical properties from epithelial glycoprotein or large amounts of deoxyribonucleic acid (DNA) (27).
III. | Epithelium |
Epithelial damage and desquamation (Fig. 2) have been described as characteristic features of asthmatic airways at autopsy (2,3,4,5,6,7,8,9,15,16,17,18,20,28,29). However, the degree of epithelial damage that is present is variable and subject to postmortem effects, and the reliability of assessing epithelial structure in autopsy cases remains unclear (30). That epithelial shedding is a feature of asthma is supported by a number of observations. Naylor (31) found clumps of columnar epithelial cells (which he called by the “euphonious and succinct” eponym “Creola bodies”) in the sputa of 42% of 100 asthma patients. They were more frequently seen during an asthma attack and occurred in only 3% of 100 nonasthmatic patients. Shed epithelial cells are found mixed in the deep layers of intraluminal mucus, and their presence in airways where the epithelium is still intact also suggests they have originated elsewhere in the bronchial tree (9) (Fig. 2c). Thomson (32) observed epithelial shedding in addition to thickening of the “basement membrane” and eosinophil infiltration in ciliated respiratory-type epithelium found in an ovarian teratoma of a patient who died of asthma with typical pathological changes observed in the lung.
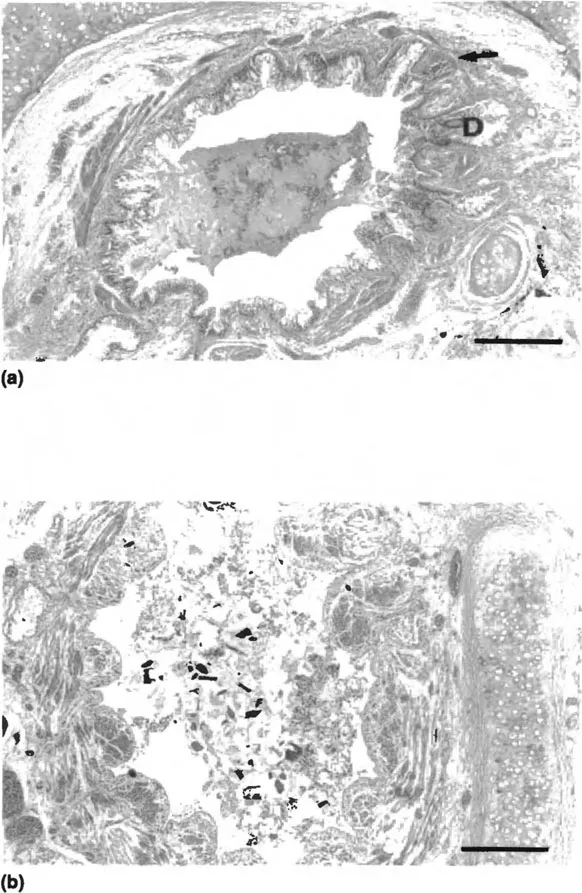
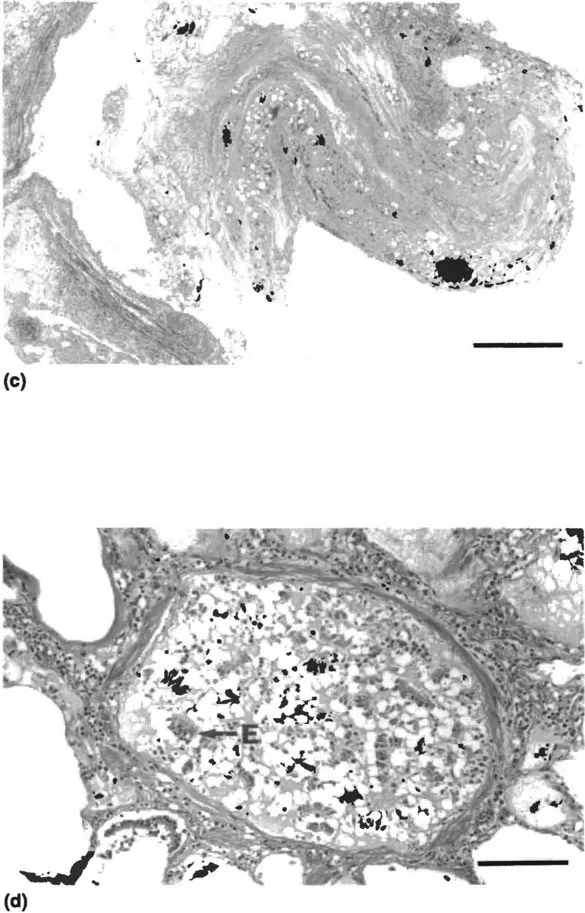
Figure 1 Photomicrographs of airways from individuals with fatal asthma with intraluminal mucus plugs: (a) intact epithelium, thickened “basement membrane,” dilated mucus gland ducts (D), and few cells in the mucus plug, bar = 0.5 mm; (b) loss of epithelium with inflammatory and epithelial cells and cellular debris in the mucus, bar = 0.5 mm; (c) organization and lamination of the mucus plug, bar = 0.2 mm; (d) obstruction of the lumen of a membranous airway with mucus, epithelial cells (E), and inflammatory cells, bar = 0.05 mm.
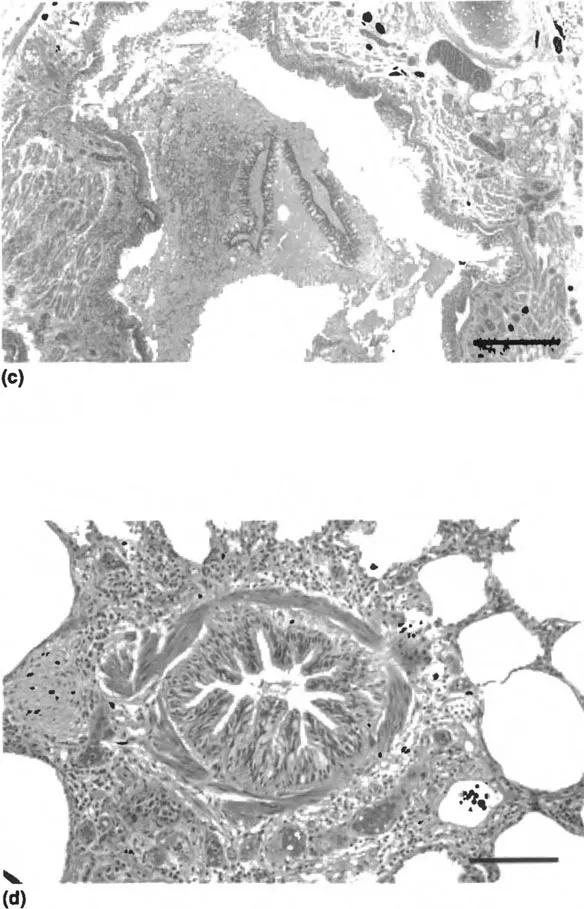
Figure 2 Photomicrographs: (a) normal pseudostratified columnar epithelium from a nonasthmatic individual, bar = 0.05 mm; (b) airway section from case of fatal asthma...
Indice dei contenuti
- Cover
- Half Title
- Title Page
- Copyright Page
- Table of Contents
- Introduction
- Preface
- Contributors
- 1. The Pathology of Fatal Asthma
- 2. Bronchoscopy
- 3. Bronchoalveolar Lavage in Studies of Asthma
- 4. Evidence from Induced Sputum
- 5. Mast Cell Proteases in Asthma
- 6. Mast Cell Cytokines in Allergic Inflammation
- 7. Airway Responses to Antigen in Asthmatic and Nonasthmatic Subjects
- 8. The Role of the Basophil in the Inflammatory Mechanisms of Asthma
- 9. Eosinophils: Granule Proteins
- 10. Eosinophil Activation in Asthma
- 11. Eosinophil Autacoids
- 12. Eosinophil Cytokines
- 13. Eosinophils in Asthma
- 14. Interactions Between Eosinophils and the Airway Epithelium
- 15. Neutrophils and Asthma
- 16. Allergen Recognition Sites in Immunoglobulin E from Patients with Asthma
- 17. Τ Cells in Asthma
- 18. Macrophages and Macrophage Diversity in Asthma
- 19. Antigen Presentation in the Asthmatic Lung
- 20. Macrophage and Dendritic Cell Populations in Airway Tissues
- 21. Fibroblasts and the Extracellular Matrix in Asthma
- 22. Mediator Functions of Epithelial Cells
- 23. Epithelium as a Target
- 24. Airway Neuropeptides and Their Role in Inflammation
- 25. Neuroimmune Interactions in Airway Inflammation
- 26. Microvascular–Epithelial Exudation of Bulk Plasma in Airway Defense, Disease, and Repair
- 27. Neuroregulation of Mucosal Vasculature
- 28. Leukocyte–Endothelial Adhesion
- 29. Prostanoids
- 30. Leukotrienes
- 31. Adenosine: Its Contribution to Our Understanding of Asthma
- 32. Chemotaxis and Mechanisms of Cell Migration
- 33. Kinins
- 34. The Early and Late Asthmatic Response to Allergen
- 35. Inflammatory Mechanisms of Aspirin-Sensitive Asthma
- 36. Inflammatory Mechanisms in Nocturnal Asthma
- 37. Inflammatory Mediators and Exercise-Induced Asthma
- 38. Mechanisms of Airway Hyperresponsiveness
- 39. Transcription Factors as Activators and Repressors of Gene Transcription: NF-κB and Glucocorticoid Receptors
- 40. Lower Airway Responses to Viruses
- Index
Stili delle citazioni per Inflammatory Mechanisms in Asthma
APA 6 Citation
[author missing]. (2018). Inflammatory Mechanisms in Asthma (1st ed.). CRC Press. Retrieved from https://www.perlego.com/book/1615527/inflammatory-mechanisms-in-asthma-pdf (Original work published 2018)
Chicago Citation
[author missing]. (2018) 2018. Inflammatory Mechanisms in Asthma. 1st ed. CRC Press. https://www.perlego.com/book/1615527/inflammatory-mechanisms-in-asthma-pdf.
Harvard Citation
[author missing] (2018) Inflammatory Mechanisms in Asthma. 1st edn. CRC Press. Available at: https://www.perlego.com/book/1615527/inflammatory-mechanisms-in-asthma-pdf (Accessed: 14 October 2022).
MLA 7 Citation
[author missing]. Inflammatory Mechanisms in Asthma. 1st ed. CRC Press, 2018. Web. 14 Oct. 2022.