![]()
1
Cell injury and cell death
Adone Baroni, Eleonora Ruocco, Maria Antonietta Tufano, and Elisabetta Buommino
When cells are damaged, as often occurs during trauma and metabolic stress, the organism has to choose whether to repair the damage by promoting cell survival or to remove irreparably injured cells. Cell injury occurs when an adverse stimulus reversibly disrupts the normal, complex homeostatic balance of the cellular metabolism. In this case, after injury the cells attempt to seal breaks in their membranes, chaperone the removal or refolding of altered proteins, and repair damaged DNA. On the contrary, when cell injury is too extensive to permit reparative responses, the cell reaches a “point of no return,” and the irreversible injury culminates in programmed cell death (PCD). Specific properties or features of cells make them more or less vulnerable to external stimuli, thus determining the kind of cellular response. In addition, the characteristics of the injury (type of injury, exposure time, or severity) will affect the extent of the damage.
We present a short overview of the best-known PCD pathways. We emphasize the apoptotic pathway, considered for years the hallmark of PCD, and the different stimuli that produce cell injury.
CELL INJURY
The survival of multicellular organisms depends on the function of a diverse set of differentiated cell types. After development is complete, the viability of the organism depends on the maintenance and renewal of these diverse lineages. Within each lineage homeostasis is maintained through a delicate balance between cell proliferation and cell death.1 Disorders of either process have pathologic consequences and can lead to disturbed embryogenesis, neurodegenerative diseases, or the development of cancer2; therefore, the equilibrium between life and death is tightly controlled, and faulty elements can effectively be eliminated by PCD, a term that well defines the planned sequence of physiological cellular autodestruction, which requires both energy expenditure and a specific enzymatic network. Cell death is an essential strategy for the control of the dynamic balance of the living system, and it is the ultimate result of most physiological as well as pathological processes. Skulachev aptly described the concept of cell death using the metaphor of the “Samurai law of biology” (i.e., it is better to die than be wrong), showing that the suicide program is a way to purify cells of damaged organelles and tissues of unwanted cells that use up valuable substrates and nutrients.3,4 Cell death thus appears as the unique solution to eliminate what is unwanted or dangerous to the “community.”3,5
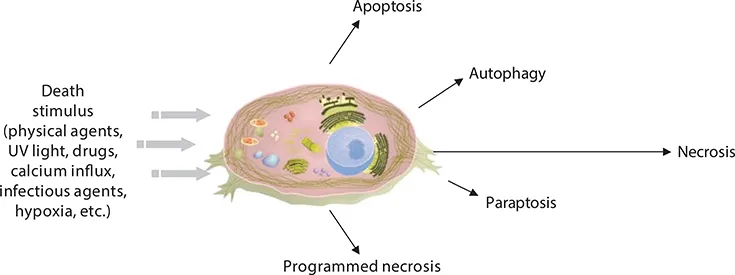
In the past, PCD was mainly associated with apoptosis, a death process characterized by morphologic changes such as shrinkage of the cell, condensation of chromatin, and disintegration of the cell into small fragments (so-called “apoptotic bodies”) that are removed by phagocytosis. On the contrary, necrosis was considered as an alternative passive cell death occurring in an accidental, violent, or chaotic way.6 Necrosis, however, has been recognized as a specific form of cell death with distinct morphological features.7,8 It is now known that cell death cannot readily be classified as “apoptosis” or “necrosis,” and alternative types of PCD have been described.9–11 Different PCD pathways exist, either mediated by caspases (a specific family of cysteine proteases, as in apoptosis) or caspase-independent (such as autophagic cell death [ACD], paraptosis, and programmed necrosis).1 Death patterns may overlap or integrate, reflecting the high flexibility in cell responses to various circumstances and stimuli (Figure 1.1).
Cell injury occurs as a result of physical, chemical, or biologic insults or as a result of vital substrate deficiency. The cellular response to injury can be adaptive, when it is designed to restore homeostasis and protect the cell from further injury. In this context, the gene transcription activity is modified in favor of vital genes.5 If the genetic and metabolic adaptive responses are inadequate for a given injury, or if injury accumulation reaches a critical level, the damaged cells commit suicide.3 Cell injury can, therefore, be reversible (sublethal) or irreversible (lethal). Cells may be reversibly injured, but if severely injured, they may be unable to recover and cell death will occur. The death stimuli are diverse and include normal physiologic signals, such as hormones that trigger deletion of cells during differentiation or involution of tissues and organs, maturation of organ systems as, for example, in the immune system, and removal of cells that have sustained some form of damage.2 Alternatively, cells already may be primed to undergo cell death, with the withdrawal of important extracellular components, such as serum or growth factors, providing the signal.12 Other death stimuli also are important from a biomedical perspective. These include physical (ultraviolet [UV] light causing damage to the skin, hyperthermia, cold, and trauma), cytotoxic drugs, calcium agents influx, glucocorticoids, infectious agents (bacteria, virus, yeast), and hypoxia. The stimuli that initiate the death pathways vary widely with the affected cells.13 In particular, various stimuli (e.g., cytokines, heat, irradiation, pathogens) can cause both apoptosis and necrosis in the same cell population (Figure 1.1). Apoptosis can be induced by a lower concentration or level of almost all the stimuli that cause necrosis.14 This means that the mechanism of self-destruction can be activated by a relatively mild stimulus. Whereas mild hypoxia produced symptoms of apoptosis, severe hypoxia produced infarction and necrosis15; similarly, exposure to temperatures between 37°C and 43°C induced apoptosis in lymphocytes, and exposure to higher temperatures induced necrosis.16 Therefore, the character of the injury will determine the pattern of cell death evoked. The three main features of injury are type of injury, exposure time, and severity.
Type of Injury
The injury can be, for example, physical, chemical, or toxic, but the response will be different for different cell types. In fact, some cells will be more susceptible than others to agents (heart muscle cells are more susceptible than connective tissue cells to oxygen depletion).
Exposure Time
The length of exposure to a particular stimulus will affect the chances of cell survival. Relatively resistant cells will be damaged if the duration of exposure is prolonged.
Severity
The ability of a cell to survive an injury also will depend on its severity; if the withdrawal of growth factor is partial, the cell is still able to survive for a long period (depending on cellular resistance), but if it is complete, cell death occurs in a very short time with modalities that vary from cell to cell.
We now describe some models of cellular death, taking into consideration that a clear-cut definition cannot be given due to the overlapping of the different programs of cell death.
Apoptosis
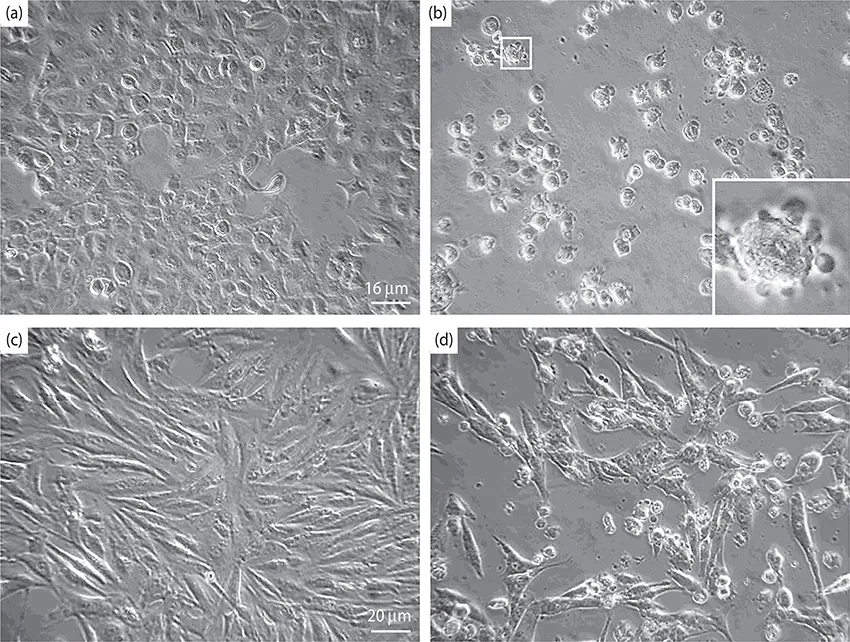
Cells have different ways of committing suicide and may select the fastest and most effective of the options available. Apoptosis has been considered for years as the PCD paradigm and is still considered one of the main pathways activated during stressful conditions. The term “apoptosis” derives from the ancient Greek word used to describe the “falling off “ or “dropping off” of petals from flowers or leaves from trees, to emphasize the normal physiological nature of the process.17 As part of the immune response, apoptosis allows the elimination of virally infected and cancer cells or the deletion of unnecessary or potentially dangerous lymphocytes.18 Defects of apoptotic cell death may promote tumor or autoimmune disease development. The apoptotic process has been shown to proceed via a number of discrete steps. Cells undergoing apoptosis are characterized morphologically by cell shrinkage, chromatin condensation, loss of contact with neighboring cells and the extracellular matrix (Figure 1.2),19 actin cleavage,20 and biochemically by DNA laddering (Figure 1.3).19 The last is a peculiarity of most apoptotic pathways. The double-stranded linker deoxyribonucleic acid (DNA) between nucleosomes is cleaved at regularly spaced internucleosomal sites, giving rise to DNA fragments representing the length of nucleosomes (180–200 base pairs).13 Molecular characterization of this process identifies a specific DNase (caspase-activated DNase) that cleaves chromosomal DNA in a caspase-dependent manner.21 Other features of apoptosis are early depolymerization of cytoskeletal proteins, loss of phospholipid symmetry in the plasma membrane with the outer layer exposure of phosphatidylserine (PS) residues, and the appearance of a smooth-surfaced protuberance of the plasma membrane with its preserved integrity. The fragmentation of both nucleus and whole cell then produces membrane-bound bodies in which the organelles are intact to form apoptotic bodies (Figure 1.2 [inset]).22 This is also called the “budding phenomenon” and should not be confused with blebs, fluid-filled structures typically devoid of organelles.6 The apoptotic bodies are cleared from tissues by professional phagocytes, such as macrophages, but also epithelial cells and even fibroblasts have been shown to clear apoptotic bodies.23 Phagocytosis is initiated by the exposure of the PS receptor located on the membrane of the phagocytes and vitronectin receptors, resulting in a cell-signaling response.22 The apoptotic pathway and the engulfment process are part of a continuum that helps ensure the noninflammatory nature of this death paradigm.23
The suppression of proinflammatory factors, during apoptotic body clearance, is accomplished at least in part by the release of antiinflammatory factors, such as transforming growth factor β and IL-10, by macrophages engaged in corpse engulfment. Regulatory mechanisms help ensure that, when phagocytozing dendritic cells present peptides from apoptotic bodies to T cells, no immune reaction against self-peptides is initiated. Defects in the clearance of corpses may predispose to autoimmune disorders.
A cascade of genes is activated as a consequence of the induction of a defined genetic program in which caspases have a prominent role. Caspases are cysteine proteases (preexisting as inactive zymogen precursors in the cell) that cleave substrates at critical aspartic acid residues.18 Activation of caspases is the central event in apoptosis, leading to the cleavage of numerous proteins involved in the cell structure, cell-cycle control, and DNA synthesis and repair. The initiator caspases (caspase-2, -8, -9, and -10) are activated by interaction with caspase adapters, whereas the effector caspases (caspase-3, -6, and -7) are downstream of the activator caspases and act to cleave various cellular targets and substrates and induce cell death.18 The enzyme poly(adenosine diphosphate [ADP]-ribose) polymerase, or PARP, was one of the first proteins identified as a substrate for caspases. PARP is involved in the repair of DNA damage. It functions by catalyzing the synthesis of PARP and by binding to the DNA strand breaks and modifying nuclear proteins.24 The ability of PARP to repair DNA damage is prevented following cleavage of PARP by caspase-3. The inflammatory caspases are involved in cytokine activation and are represented by caspases-1, -4, -5, -11, -12, -13, and -14.