
eBook - ePub
Clinical Responsibility
Jane Lynch, Senthill Nachimuthu
This is a test
Share book
- 228 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Clinical Responsibility
Jane Lynch, Senthill Nachimuthu
Book details
Book preview
Table of contents
Citations
About This Book
Clinical Responsibility provides practical legal advice by highlighting real-life healthcare case studies and workplace examples. It looks specifically at the areas of accountability, the legal process, what constitutes a legal claim brought by the patient, and the duty of care and how it is measured. It assists and guides health professionals in understanding their legal and professional obligations and the implications for managing risk.
Frequently asked questions
How do I cancel my subscription?
Can/how do I download books?
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
What is the difference between the pricing plans?
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
What is Perlego?
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Do you support text-to-speech?
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Is Clinical Responsibility an online PDF/ePUB?
Yes, you can access Clinical Responsibility by Jane Lynch, Senthill Nachimuthu in PDF and/or ePUB format, as well as other popular books in Medicine & Public Health, Administration & Care. We have over one million books available in our catalogue for you to explore.
Information
CHPATER 1
Introduction
Over the recent past the ethos in healthcare has changed. Gone are the days when a doctor was put on a pedestal and not to be challenged, when it was routine to simply say to a patient ‘nice to see you, fix you tomorrow’, when health records were marked ‘not to be handled by the patient’!
Now, of course, we live in a very different world. Patients are much more aware of their rights. Access to the internet has opened a huge arena for exchange of information, allowing patients to be more informed.
There is the law relating to consent. The health professional has an obligation to obtain consent of the patient before they can treat them. If they fail to comply with the rules of consent, they are in danger of committing a criminal offence.
Patients now have a legal right to access to their records and indeed we now have patient-held records. Health professionals have a legal obligation to keep patient information confidential. This causes practical problems for the health professional when sharing information. If they do not comply with the issues of confidentiality they will be accountable.
For health professionals this means that the law has become part of their role and is now an everyday concern. The complexities of the law do not make this an easy task for them. In a healthcare setting, it leaves the health professionals vulnerable. In practice, they go about their daily routines, making decisions about patient care, planning and treatment and it is hoped that the right decisions are made and that the employer will stand by them and courts will uphold their decisions.
Health professionals have concerns about who is responsible when a patient suffers harm. Can a health professional be held accountable where they have no control over resources or they are ignorant through lack of training?
Health professionals are often heard in the witness box saying, ‘Staff were under pressure, but I meant well. I acted in good faith.’
Of course health professionals do not intend to cause harm; they may have no control over resources; they may be ignorant of procedures through lack of training. But this does not exonerate health professionals from their responsibility. So when something goes awry they are accountable.
It is important for health professionals not only to be aware of their legal and professional obligations, but also to put them into perspective, to get the balance right. Often health professionals have an unhealthy fear of the law, causing unnecessary anxiety. This approach is balanced by an unrealistic view that it will never happen to them; that someone else or something else is responsible, ‘but not me’. Often a defensive approach is adopted. ‘I don’t have the time’; ‘it’s because of financial constraints’; ‘it’s my manager’s responsibility’; or ‘it’s the consultant’s responsibility’. The health professional cannot simply pass responsibility onto someone else. They will be accountable for their actions.
My intention in writing this book is not to alarm the health professional unduly, but to impart the information realistically in a way that a balance may be struck and so remove the spectre of the court.
We shall look at how the court process works: the different types of court processes, the difference between the civil and criminal process and how a health professional might become involved in those court processes.
We will look at a legal claim: how a patient may sue for clinical negligence; what the patient needs to prove in order for any claim to succeed; what the duty of care is, how the duty of care is measured, what constitutes a breach of duty of care and to whom is the duty of care owed. What are the consequences for the health professional when a patient sues for clinical negligence? Who pays the compensation?
Then there are the professional implications: when and how the health professional is accountable to the professional bodies and what the consequences are.
There are issues in the course of employment: governance and risk management, a breach of contract of employment, accountability for team decisions, following orders, following guidelines and protocols, waiting lists, prescribing, lack of resources and poor record-keeping, amongst other things.
It is important that the health professional understands the separate areas of accountability as this is the underlying premise of their responsibility and all that flows from it.
The High Cost of Litigation
The NHS litigation authority (NHSLA) in their annual report (November 2008) stated that as of March 2008, it estimated that it had potential liabilities of £11.9 billion relating to clinical negligence claims.1 This staggering figure does not include the cost of staff and management time in dealing with these complaints or the additional cost of bed space. So the true cost is far higher. This figure represents something in the region of 10% of the annual budget. If you compare this with the prescription budget, which is around 8%, you can see how much litigation is costing the Trusts.
One of the major causes of a clinical accident is a breakdown of communication, often through poor record keeping and system failures. We will look at these specifically later in the book.
If a clinical accident occurs then all of the health professionals involved in the care will be accountable and there may be both legal and professional implications. Clinical responsibility cannot be passed like a hot potato. The health professional must take responsibility for all actions that they take and will have to justify the steps taken. It is this foundation that must be grasped at the outset. They cannot avoid responsibility because, for example, they are being supervised, nor can the health professional assume that a consultant in charge of the ward will have to carry that responsibility alone. These complex areas of accountability will be explored in detail later.
In recent years, I have heard that some Trusts advocate a ‘no blame’ culture. When something has gone wrong the individuals concerned will not carry any blame. Whilst to some extent this may remove the difficulties surrounding the reluctance of staff to come forward to whistle blow and the lack of openness when something has gone wrong, I do not believe that the law would uphold such a culture, as this would remove from the equation the health professional’s accountability. My own view is that a more sensible approach would be a ‘fair blame’ culture. So that those responsible are held to account, but there is not a culture of passing the buck and blaming those who are not responsible. To adopt a ‘no-blame’ culture may result in inadvertently turning a blind eye to matters of importance and ultimately risk management.
Reference
1 National Health Service Litigation Authority. Report and Accounts: fact sheet 2, financial information. London: National Health Service Litigation Authority; 2008.
CHPATER 2
Accountability
‘I was following my orders. My boss told me to do it.’
The concept of ‘accountability’ is one which is familiar to all health professionals. It is a word that they all know and use and forms part of their working day vocabulary. But how can it be defined?
TASK
- Before you read further try to define ‘accountability’.
- List the areas where you think you are accountable.
Accountability in a Legal Context
In a legal context, there is no distinction between responsibility and accountability. Responsibility can be defined as being accountable for, answerable for or liable to be called to account.
As a health professional, patients must be able to trust you with their lives and health. To justify that trust, care must be the health professional’s first concern, providing a good standard of care. Health professionals are personally accountable for their professional practice and must be able to justify their decisions, actions and omissions.
The reality of the situation is that a health professional is, on a personal level, answerable and can be called to account. Once that premise has been accepted, the inevitable and consequent enquiry that must flow from it is to whom and how is that accountability discharged?
It is the courts that determine whether or not a health professional has discharged their duty. The law, by its nature, is reactive and is invoked after the event. It is only when a real case is presented that the judges will deliberate and deliver judgment. It follows then that issues are debated with the benefit of hindsight. Thus, we cannot go to the courts with hypothetical questions or scenarios: ‘If I do it in particular way, will I be in trouble?’ The usual sequence is that something will have happened to trigger an investigation. This will raise the question of accountability. When the health professional appears before the court his acts or omissions will be weighed up and judgment will be delivered. The practical effect is that health professionals make decisions about patient care and it is hoped that the courts will ultimately support them.
Accountability has now been put into its legal context. The next question then is: to who is the health professional accountable?
TASK
- ■ To whom are you accountable?
List them
The Four Areas of Accountability
There is not just a single individual or body to whom the health professional is accountable, but four separate and distinct areas where they are answerable. In the widest sense, the health professional is answerable to society. Perhaps, and more importantly from the health professional’s perspective, he must be accountable and answerable to the patient. Equally, the health professional will be answerable to their employer and last, but certainly not least, the health professional will also be accountable to his profession.
There is one other area of accountability that might be considered and that is that the health professional is accountable to themselves. This is a moral obligation and one that is not enforced by law, but might be considered as being at the centre of professional practice and skill. However, these moral and ethical considerations are not within the ambit of this book.
Having established that the health professional can be accountable in four quite separate and distinct respects, we need next to examine how that impacts in practice.
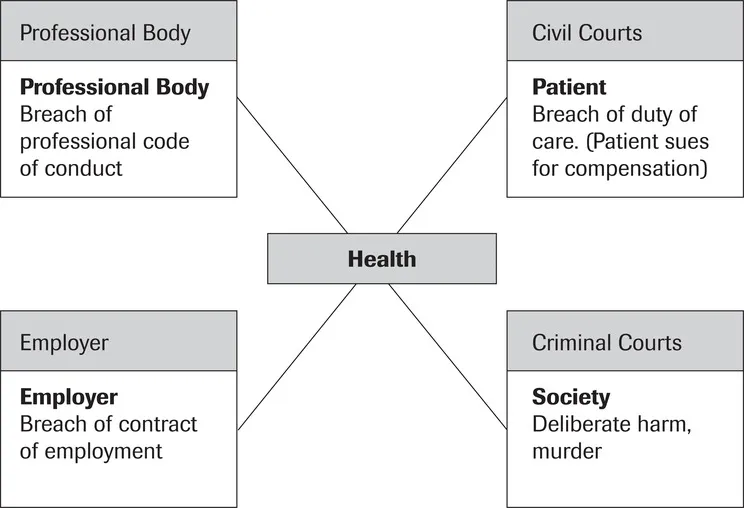
FIGURE 2.1 Four areas of accountability
Society
Health professionals are accountable to society for issues that are in the public interest. Society dictates the kind of behaviour they will or will not tolerate. If someone is murdered, society says this is wrong and the murderer must be punished. Society’s view is then enshrined in criminal law. We have seen manslaughter charges brought against school teachers where a child has died on a school trip. These charges ...