- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
General Practice at a Glance
About this book
Awarded First Prize, in the Primary health care category, at the 2013 BMA Medical Book Awards.
Following the familiar, easy-to-use at a Glance format, this brand new title provides a highly illustrated introduction to the full range of essential primary care presentations, grouped by system, so you'll know exactly where to find the information you need, and be perfectly equipped to make the most of your GP attachment.
General Practice at a Glance:
- Is comprehensively illustrated throughout with over 60 full-page colour illustrations
- Takes a symptoms-based approach which mirrors the general practice curriculum
- Offers 'one-stop' coverage of musculoskeletal, circulatory, respiratory, nervous, reproductive, urinary, endocrine and digestive presentations
- Highlights the interrelations between primary and secondary care
- Includes sample questions to ask during history taking and examination
- Features 'red flags' to highlight symptoms or signs which must not be missed
This accessible introduction and revision aid will help all medical students and junior doctors develop an understanding of the nature and structure of primary care, and hit the ground running on the general practice attachment.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
1
The 10-Minute Consultation: Taking a History
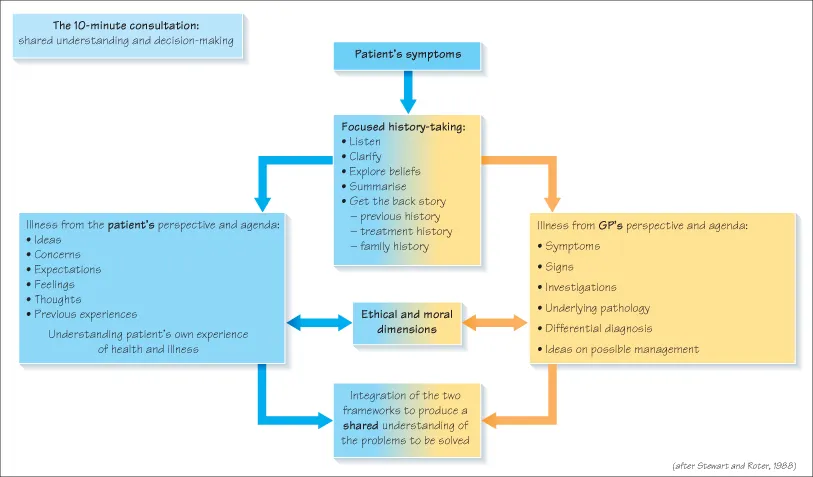
At finals you could spend 20–40 minutes clerking your patient. So how can a 10-minute consultation in general practice produce an adequate assessment?
- Continuity of care means the patient and their history are often familiar.
- The 10-minute consultation is an average. A quick consultation, like a repeat medication request, saves time which can be spent on trickier problems.
- You don’t need to do everything in one consultation. It can help to watch a problem develop over several visits.
- Making diagnoses is honed through practice, enabling GPs to recognise patterns of illness quickly. This is not ‘taking short-cuts’: it’s about the expertise to focus on key areas.
As a student, don’t rush to assess a patient in 10 minutes. Take the time you need to understand your patient’s problem fully. Speed comes with experience.
What’s the Difference between a Focused History and a Traditional One?
- Traditional history-taking is useful when you first learn to interview patients as it teaches you a structure and a list of questions to ask.
- You’ll notice senior doctors often ask surprisingly few questions, yet get a better view of the problem.
- This ‘focused history’ requires judgement about what to explore and what to set aside. Judgement is based on many things including knowledge and experience.
- Learning focused history-taking is an important transition between student and doctor. General practice is the ideal setting to practise this because you will see many undiagnosed patients on whom to hone your skills.
Focused History-Taking in a Nutshell
Listen
- ‘What can I do for you today?’ Students often hope to save time by getting straight to the point with direct questions. The opposite happens. You get a better foundation for exploring the problem if you give the patient the time to tell their story from their perspective: start with an open question and then listen.
- The ‘golden minute’ (give the patient a minute to speak without interruption) gives your patient time to frame their problem in their own way.
- ‘Go on … tell me more …’ If the patient falters, encourage them to carry on. Use non-verbal encouragement through head nodding and eye contact.
- ‘You were saying the pain is worse at night …’ Reflection can get help your patient going again.
- Don’t fear silence, particularly in emotionally charged situations. Give the patient space to formulate their thoughts.
Clarify
- ‘When were you last completely well?’ Establish the timetable of the patient’s symptoms.
- ‘Can you describe the pain?’ Analyse each symptom. Mnemonics can help, such as SOCRATES: Site, Onset, Character, Radiation, Associated factors, Timescale, Exacerbating/relieving factors, Severity.
- ‘What do you mean by indigestion?’ Understand what the patient means, especially if they use medical terms. ‘Migraine’ often means ‘bad headache’, ‘blood pressure’ may mean dizziness, headaches or almost anything else.
- Ask red flag questions to detect serious underlying conditions. In back pain, ask about incontinence and urinary problems, history of cancer and TB.
Explore Beliefs
- ‘What are your thoughts about this?’ The patient may have a very good idea of their diagnosis, ‘It’s just the same as my aunt had.’ Equally, they may have a very misleading idea, ‘This website said it’s typical of Candida infection.’ Knowing your patients’ ideas may help you diagnostically, or help your patients away from incorrect formulations.
- ‘In your darkest moments what do you think this might be?’ Look for hidden agendas and explore your patients’ concerns. Patients with headaches often worry about brain tumours or meningitis. They rarely volunteer this for fear of looking foolish, maybe because they’re afraid they may be right. Your diagnosis and treatment may be spot on, but if you haven’t uncovered these concerns and put your patient’s mind at rest, you send away a worried patient.
- ‘What are you hoping we can do?’ What are your patient’s expectations for treatment. When you come to plan management, taking your patient’s expectations on board will help you achieve concordance with your patient (see Chapter 2).
- Above all, don’t try to guess what your patient is thinking. There’s no point reassuring your patient about something that never worried them. Their real concerns (which might seem bizarre to you or to the next patient) may be life and death to them.
Summarise
‘Let me see if I’ve got this right …’ Once you have grasped the patient’s problem, summarise it back. This checks your own understanding, and reassures the patient that they’ve been understood.
The Past Medical History
- The past medical history is essential background to the presenting problem. The GP may not need to explore it in a familiar patient, or if the records are to hand.
- ‘Have you had any serious illnesses?’ ‘Have you seen a specialist or been in hospital?’ Don’t list random diseases, ask general questions about the past, and …
- Ask specific questions relevant to the presenting complaint. Ask ‘Ever had migraine?’ to the patient with headaches.
The Treatment History
- ‘Can you bring all your medicines to the surgery with you?’ Drug side effects and interactions cause huge amounts of iatrogenic illness and many hospital admissions. A secure drug history will allow you to spot current problems and prevent your own prescribing causing future ones.
- The drug history is a back door...
Table of contents
- Cover
- Table of Contents
- Preface
- Introduction: how to make the most of your GP attachment
- 1 The 10-minute consultation: taking a history
- 2 The 10-minute consultation: managing your patient
- 3 Continuity of care and the primary healthcare team
- 4 Why do patients consult?
- 5 Preventive medicine
- 6 Significant event analysis, audit and research
- 7 Communication between primary and secondary care
- 8 Principles of good prescribing in primary care
- 9 Prescribing in children and the elderly
- 10 Law and ethics
- 11 Child abuse, domestic violence and elder abuse
- 12 The febrile child
- 13 Cough and wheeze
- 14 Asthma
- 15 Abdominal problems
- 16 Common behaviour problems
- 17 Childhood rashes
- 18 Child health promotion
- 19 Musculoskeletal problems in children
- 20 Common sexual problems
- 21 Sexually transmitted infections and HIV
- 22 Contraception
- 23 Subfertility
- 24 Termination of pregnancy
- 25 Menstrual disorders
- 26 The menopause
- 27 Common gynaecological cancers
- 28 Breast problems
- 29 Antenatal care
- 30 Bleeding and pain in pregnancy
- 31 Other pregnancy problems
- 32 Acute confusional state and dementia
- 33 Fits, faints, falls and funny turns
- 34 Chest pain
- 35 Stroke
- 36 Peripheral vascular disease and leg ulcers
- 37 Preventing cardiovascular disease
- 38 Breathing difficulties
- 39 Cough, smoking and lung cancer
- 40 Asthma and chronic obstructive pulmonary disease
- 41 Diabetes
- 42 Thyroid disease
- 43 Acute diarrhoea and vomiting in adults
- 44 Dyspepsia and upper gastrointestinal symptoms
- 45 Lower gastrointestinal symptoms
- 46 The acute abdomen
- 47 Back pain
- 48 Hip and lower limb
- 49 Neck and upper limb
- 50 Inflammatory arthritis, rheumatism and osteoarthritis
- 51 Upper respiratory tract infection (including sore throat)
- 52 Ear symptoms
- 53 The red eye
- 54 Loss of vision and other visual symptoms
- 55 Eczema, psoriasis and skin tumours
- 56 Other common skin problems
- 57 Depression
- 58 Anxiety, stress and panic disorder
- 59 Alcohol and drug misuse
- 60 Eating disorders
- 61 Psychosis and severe mental illness
- 62 Headache
- 63 Tiredness and anaemia
- 64 Insomnia
- 65 Allergy and hay fever
- 66 Urinary tract disorders
- 67 Chronic pain
- Further reading and resources
- Index
- Advertisement
- End User License Agreement
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access General Practice at a Glance by Paul Booton,Carol Cooper,Graham Easton,Margaret Harper in PDF and/or ePUB format, as well as other popular books in Medicine & Family Medicine & General Practice. We have over one million books available in our catalogue for you to explore.