![]()
1
Why Rapid Assessment Is Essential for Ward Staff
INTRODUCTION
There is an increasing emphasis in the modern health service on managing most illnesses in community settings and performing most surgery in day surgery units. Consequently, the number of inpatient beds has fallen by about 40% in the past 25 years, although in the same period numbers of hospital admissions have risen by 74% (NHS Confederation, 2006; Hospital Episode Statistics inpatient data, 2006–07). In addition, an increasing proportion of patients are admitted as emergencies: there were 4.7 million emergency admissions in 2006–2007, equating to 36% of all in-patient cases (Hospital Episode Statistics inpatient data, 2006–07). Therefore, hospital occupancy and throughput rates are generally high, and the relative numbers of acutely and critically ill patients have significantly increased. Furthermore, the proportion of older patients in hospital is also rising each year: 41% of adult inpatients were aged 65 years or more in 2006–2007 (Hospital Episode Statistics inpatient data, 2006–07), and this group often have one or more chronic conditions that increase the complexity of their care.
Factors contributing to increased acuity of general ward patients are:
- Faster throughput
- Increased numbers of emergency cases – more acute and critical illness
- Increased numbers of older patients – more complex, chronic disease
- More aggressive and invasive treatments.
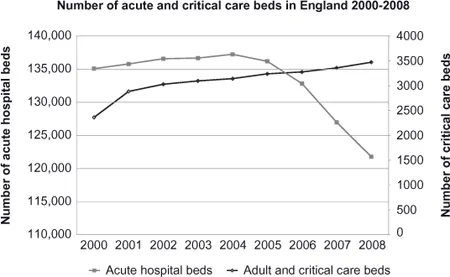
Fig. 1.1 Numbers of all acute care beds and critical care beds in England 2000–2008
Sources: www.performance.doh.gov.uk/hospitalactivity/data_requests/download/beds_open_overnight/beds_ts08_1.xls;
www.performance.doh.gov.uk/hospitalactivity/data_requests/download/critical_care_beds/ccbed_ts_jul08.xls
Despite these points, designated critical care beds in England make up less than 3% of all inpatient beds (Department of Health Performance Data and Statistics – Beds, 2008) (Figure 1.1). As a result, many patients with potential or actual serious illness are located in general wards; and the numbers of these patients continue to rise. It is difficult to gauge exactly how many patients may be in this category at any one time. In 2002, a snapshot review of 1873 ward patients in four Hospital Trusts found that 12.2% needed care over and above normal ward levels, while a follow-up audit in the same area in 2006 found that 21.3% required such care (Chellel et al, 2002; Smith et al, 2008).
LEARNING OBJECTIVES
By the end of this chapter you should be able to:
Outline reasons for the increased acuity and dependency of patients cared for in general ward areas
Understand/describe the definition of Level 1 care
Identify the priorities of rapid assessment and intervention in the acutely ill patient
Describe the common framework for assessment of the acutely unwell patient
Understand the importance of having/using an effective triggering system to ensure help is called at an appropriate time
Understand the importance of communication in ensuring that the patient receives timely and appropriate assistance.
LEVELS OF CARE (INTENSIVE CARE SOCIETY, 2009)
Descriptors of the levels of care needed by different patients have been published by the Intensive Care Society (2009) – Level 2 and Level 3 patients will usually be managed in a designated critical care area – if aggressive measures are appropriate. However, as has been noted above, there are many Level 1 patients on wards: these are patients at risk of deterioration or patients recently transferred from a higher level of care whose needs can be met on an acute ward as long as there is additional advice and support from the critical care team (Intensive Care Society, 2009). In this context, it is imperative that staff working in wards are able to recognise (and intervene effectively) when patients deteriorate.
Box 1.1 Level 1 patients
- Patients recently discharged from a higher level of care: e.g. needing at least 4-hourly vital sign observations.
- Patients in need of additional monitoring/clinical interventions, clinical input or advice: e.g. needing at least 4-hourly observations, or continuous oxygen therapy, or boluses of intravenous fluid, or epidural analgesia; or with a tracheostomy or chest drain in situ, or receiving an intravenous infusion of insulin; or needing physiotherapy to prevent or treat respiratory failure.
- Patients requiring critical care outreach service support: e.g. with abnormal vital signs but not (yet) needing a higher level of care; and those at risk of deterioration with a potential requirement for a higher level of care.
ARE WARD STAFF READY FOR THE CHALLENGE?
Nursing staff are the constant monitors of patients’ well-being. Nurses must ensure that their knowledge of the patient is not restricted to arm’s-length evaluation of data but is based on regular accurate assessments and a good understanding of the patient’s physical and mental state. In order to do this, nurses must have an appreciation of what is normal and what is not.
However, at the same time as the acute hospital patient population has changed – and generally become more challenging – there have also been a number of changes to the way that medical and nursing staff are trained and work. These developments have not helped staff to easily become competent in recognising and responding to sudden acute deterioration in patients.
Limited experience with sick patients for medical and nursing staff
Changes in the way that nurses are trained have led to a reduction in time spent gaining ‘hands-on’ experience with patients. The typical 3-year training for a nursing diploma or degree complies with the Nursing and Midwifery Council requirement for 50% theory and 50% practice (NMC, 2004). It is likely to include a maximum of 2300 hours of total practice experience – or 102 days per year (NMC, 2004) – which must cover all aspects of nursing, thus allowing only a limited time specifically with sick patients.
These changes mean that intuitive recognition of acute deterioration is likely to be less well-developed and will require teaching that is specific to subjective indicators (such as skin colour and behavioural changes) as well as better understanding of the more objective indicators (such as respiratory rate and blood pressure). Ruth-Sahd and Hendy (2005) found that novice nurses depended heavily on intuition and were unable to explain the reasoning behind their decisions. They were more likely to be correct if they were older and had a broad spectrum of social and personal experience. In a study of nurses who had called the emergency team because they were worried, Cioffi (2000) found that in the process of recognition, nurses relied heavily on past experiences and knowledge to detect differences in the patient’s condition.
Similar issues have arisen within the medical profession with concerns about the amount of clinical experience of trainee doctors and the impact of foundation year programmes and postgraduate training structures that result in far less time getting ‘hands-on’ exposure to patients (McManus et al 1998). Senior doctors are also likely to be less experienced than they used to be: a British Medical Journal editorial pointed out that it is now possible to become a consultant surgeon with 6000 hours of specialist experience, whereas previously a trainee might expect to work 30,000 hours (Chikwe et al, 2004).
Such deficits need to be addressed by focused teaching that develops and enhances the knowledge and skills required for the recognition and management of acutely ill patients. These include skills of assessment, problem and risk identification and knowledge of appropriate interventions.
PROBLEMS IN ACUTE CARE
Reports from around the world show major healthcare systems struggling to meet the challenge of providing consistently safe and effective care of acutely and critically ill patients (e.g. Australia – Wilson et al, 1995; USA – Kohn et al, 2000). In the United Kingdom, McQuillan et al (1998) examined the care of patients that had deteriorated to the point that they required transfer to intensive care. In a total of 100 patients from two hospitals, only 20 patients were judged to have been well managed, while 54 experienced sub-optimal care in the period before transfer. Outcomes were poor even among those patients considered well-managed, with a mortality rate of 35%; however, in the sub-optimal care group, the mortality rate was 56%. Importantly, the baseline characteristics of the two groups of patients were not significantly different and the difference in mortality can be attributed to the difference in quality of care rather than to differences between the patients themselves. Other studies have also shown the impact of sub-optimal ward care in prestigious teaching hospitals (McGloin et al, 1999; Vincent et al, 2001) and district general hospitals alike (Seward et al, 2003).
As recently as 2005; the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report of care in 1154 acute medical patients in 179 English hospitals found:
- Initial assessment was unacceptable in 10% of cases
- Initial treatment was delayed and inappropriate in 48% of cases
- Care was less than good practice in 47% of patients, and contributed to death in one-third of the cases.
It is important to emphasise that these problems are often the product of ineffective systems rather than individual lack of skill, knowledge or judgement. McQuillan et al (1998) found that failures of organisation and lack of supervision were significant factors, but also that failure to appreciate clinical urgency and seek advice played a part. Most often, poor patient outcomes are linked to delayed recognition and ineffective management of fundamental aspects of care, such as:
- Ensuring a clear airway
- Optimising breathing and giving oxygen
- Treatment of circulatory failure.
(McQuillan et al, 1998; McGloin et al, 1999)
Healthcare workers have an individual and collective responsibility to reflect on their own performance and address any deficits in knowledge or skills as well as to evaluate the strengths and weaknesses of the system as a whole. This approach can form the basis of a high-quality service that works to minimise variability and risk in patient care.
PRIORITIES OF ASSESSMENT AND INTERVENTION
It is essential that all staff are familiar with the clinical priorities in life-threatening situations in order to ensure that problems are identified and treated in the right order. The right order is one that identifies and treats problems that will harm or even kill the patient most rapidly. There is a very clear hierarchy for this.
Key Point
Identify and respond first to what will kill the patient first.
In all cases, problems causing hypoxia and hypotension are potentially life-threatening and should be identified and treated immediately. It is therefore not surprising that the A (Airway), B (Breathing), C (Circulation) format taught on basic and advanced life support courses (Resuscitation Council UK, 2006) and similar programmes equally applies to management of patients that are acutely unwell. Once these priorities have been addressed, other important assessments can be made.
Box 1.2 Definitions
Hypoxia = inadequate availability of oxygen for cell metabolism
Hypotension = low blood pressure (systolic BP <90 mmHg or decreased by >40 mmHg from normal)
Clearly, if the patient is not seen to be breathing through a clear airway, and/or there is no palpable pulse, a cardiac arrest call should be made and life support commenced.
Key Point
Unresponsive patient or patient with grossly abnormal (or no) breathing or no palpable pulse = Cardiac Arrest Call.
In an acute situation, assessment will initially focus on the patient himself, with most information obtained from a direct examination. However, once any life-threatening problems have been identified or excluded, a more thorough assessment can be made using information from other sources.
Additional sources of information include
- Observation charts
- Fluid balance charts
- Prescription charts
- Blood chemistry/haematology results
- Microbiology results
- Relevant x-rays and scans
- The patient’s medical team
- Other healthcare professionals
- The patient’s family.
USING AN ASSESSMENT FRAMEWORK FOR INITIAL ASSESSMENT
In an acute situation, it is important to have a simple structure to ensure that priorities are addressed and then that all other relevant issues are considered. A systematic approach should be used; it should highlight the life-threatening problems that must be recognised and responded to first. Most training programmes designed to improve capability in managing the sick patient use the A-B-C-D-E structure (see Table 1.1).
Key Point
Use a systematic approach when assessing a sick patient: this supports identification of the main priorities and ensures that the most important issues are assessed and addressed.
Table 1.1 A systematic framework for priority-driven initial assessment of the sick patient
| A | Airway | Patient is talking |
| | Stridor heard |
| B | Breathing | Chest movement is equal |
| | Respiratory rate |
| C | Circulation | Pulse rate |
| | Peripheral temperature or capillary refi ll |
| D | Disability | Level of consciousness Pain |
| E | Examination or Exposure | Obvious infl ammation Bleeding |
The chapters that follow will expand and explain each step of the assessment framework.
CALLING FOR APPROPRIATE ASSISTANCE
According to local arrangements, each organisation should ensure that there are clear guidelines for calling for help from the patient’s own medical team and a Critical Care Outreach service (where this exists). Such guidelines enable the patient to receive an appropriate level of timely, expert support: early interventions can minimise further deterioration and improve outcomes (Newby et al, 1996; Rivers et al, 2001). Conversely, delays in transfer to a critical care unit with the right staff, equipment and expertise...