This is a test
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Book details
Book preview
Table of contents
Citations
About This Book
Offering a balance of theory and practice, with guides for further reading, this is a clinical guide for the practitioner in the widest sense: physicians, nurses, occupational hygienists, safety officers, environmental, health officers and personnel managers. With coverage of both medicine and hygiene, and including sections on OH law, it is a primer for appropriate courses and provides all that the interested medical student would need to know.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Occupational Health by Tar-Ching Aw, Kerry Gardiner, J. M. Harrington in PDF and/or ePUB format, as well as other popular books in Medicine & Public Health, Administration & Care. We have over one million books available in our catalogue for you to explore.
Information
1
Introduction
1.1 What is occupational health?
1.2 Who is involved in occupational health?
1.3 The world of work
1.4 The world of people at work
1.5 The roles of the occupational health professional
1.6 Industrial processes and health outcomes
1.7 Summary
1.8 The future
1.1 What is occupational health?
Occupational health is a multifaceted and multidisciplinary activity concerned with the prevention of ill health in employed populations. This involves a consideration of the two-way relationship between work and health. It is as much related to the effects of the working environment on the health of workers as to the influence of the workers’ state of health on their ability to perform the tasks for which they were employed. Its main aim is to prevent, rather than cure, ill health from wherever it arises in the workplace.
A joint International Labour Organization/World Health Organization (ILO/ WHO) Committee defined the subject back in 1950 as: ‘the promotion and maintenance of the highest degree of physical, mental and social wellbeing of workers in all occupations’.
The relationship between the worker and the world of work is, necessarily, complex (Fig. 1.1). The worker brings to the place of work a pre-existent health status influenced by many factors—only some of which are under the workers’ direct control. Any illness that occurs in the employed worker has to be viewed in this context. The health outcome could be caused by work, modulated by work or unrelated to it. Such a view of occupational health is, however, predominantly a medical model. The situation is much more complex nowadays.
1.2 Who is involved in occupational health?
Traditionally, occupational health has been viewed as a clinical subject, implying that the dominant roles in prevention should be played by the physician and the nurse. The ILO/WHO definition from nearly half a century ago suggests that a broader view is necessary.
Thus, the list of relevant professionals is extensive and includes:
- physicians;
- nurses;
- occupational hygienists;
- sociologists;
- toxicologists;
- psychologists;
- health physicists;
- microbiologists;
- epidemiologists;
- ergonomists;
Fig. 1.1 The problems facing the practitioner attempting to establish a link between work and health. The new employee brings a legacy of genetic, social, dietary and environmental factors affecting health to the new workplace, which may influence his or her response to workplace hazards.
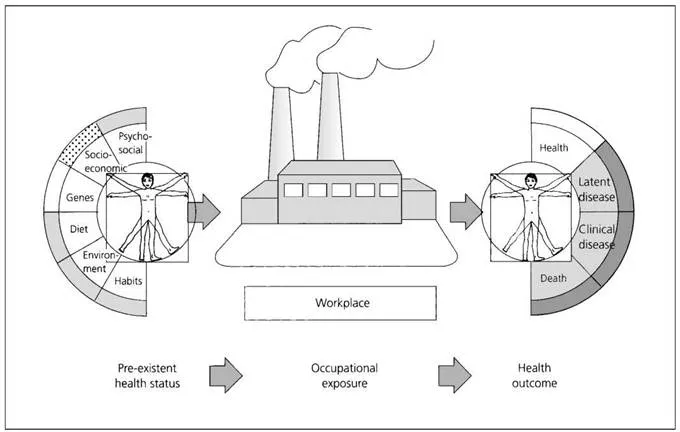
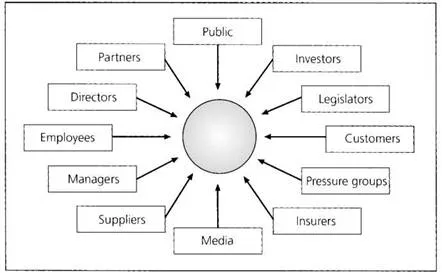
Fig. 1.2 The occupational health stakeholders.
- safety engineers;
- work organisation experts;
- lawyers.
Yet, the ultimate responsibility for maintaining the health of the workforce rests with the employer, and, to a lesser extent, with the employee. This is the way most health and safety law is formulated. On the basis of this model, one can begin to view those involved as an even broader group. The ‘stakeholders’ would thus include a number of groups who, although they may not be professionally responsible for ensuring the wellbeing of the workers, do have a crucial interest in the outcome (Fig. 1.2).
1.3 The world of work
The changing patterns of employment in world industry will have important implications for the future style and thrust of occupational health, as well as for the competence needed to deliver the goods. Across the world, the days of full-time, long-term employment in one industry for a worker with one set of skills are rapidly disappearing. The main features for the future seem to be:
- fragmented industry;
- smaller workforces;
- more mobile employees;
- multi-skilled workers;
- greater use of subcontracted tasks;
- less job stability;
- less job security;
- more part-time work;
- more flexible hours of work;
- more mechanised (and therefore possibly more dehumanised) workplaces.
1.4 The world of people at work
Today, certainly in the developing world, occupational physicians see more illness but less disease. Whilst musculoskeletal disorders and stress-related complaints dominate the scene, they too are interrelated and both are subject to ‘somatising tendencies’ (presenting as physical symptoms related to different target organ systems). Thus, the new ‘age of existentialism’ is dominated by such conditions as:
- stress;
- non-specific effect modifiers;
- post-traumatic stress disorder;
- chronic fatigue syndrome;
- multiple chemical sensitivity;
- diffuse pain syndromes;
- a combination of psychological, neurological, and immunological issues.
1.5 The roles of the occupational health professional
In developed countries, many of the older occupational diseases have been controlled—or, at least, the means for controlling them are known. In such settings, the delivery of an effective occupational health service to employed people will become more complex and more difficult in the future—although with greater emphasis on control, there should be less to do in dealing with the injured or sick. These, after all, represent the ‘failings’ of an effective preventive programme.
Moreover, the influences of the stakeholder and the complexities of the employment scene have shifted the traditional emphasis away from the structure of ‘see the health effect, diagnose the illness, find the cause’ to the more proactive stance of ‘control the exposure and monitor the effects’. In this model, the roles of the safety engineer and the occupational hygienist become more central, and now sit alongside the clinical aspects rather than being secondary to them. One further aspect of occupational health services is worth mentioning: in the market economies, there has been a shift towards demonstrating to employers the economic value to them of such a service. A UK Faculty of Occupational Medicine brochure listed the ways in which occupational physicians can help the employer to ‘meet their obligations’ under European health and safety legislation. These included:
- helping with company compliance with the law;
- advising on health and safety policy;
- assisting in the control of sickness absence;
- reviewing the fitness of employees’ post-sickness absence;
- managing rehabilitation;
- advising on fitness to work;
- managing access to first aid services;
- organising health promotion initiatives;
- designing and managing substance abuse programmes at work;
- advising on the management and alleviation of stress;
- advising employees about overseas travel on company business;
- assessing employees’ eligibility for long-term disability benefits or retirement on health grounds.
The order of these functions is probably not random, and many might dispute the contents of this list and certainly the order. Nevertheless, it demonstrates the move towards delivering an economically attractive package to the employer. Whether this is what the employee needs is another matter. Indeed, one can dispute whether this medical model has real validity for the twenty-first century.
In developing countries, an occupational health service often starts with the provision of medical care for the workforce (akin to a general practice at the worksite, and often with provision for the workers’ dependants) (see Chapter 2). In the newly emerging countries of Eastern Europe, the ‘prophylactic’ medical examination remains at the heart of the health-care system in the workplace. Even in Poland, which is among the more advanced of this group of countries, their 1997 Occupational Health Services Act places medical examinations at the core of service activities. Recent updates of the legislation have tended, however, to stress the importance of the preventive role of the medical input.
Many of these functions are often performed by an occupational health nurse, who frequently works in isolation from any form of direct medical advice. Both physicians and nurses, however, have to be aware of their clinical limitations (either by training or by the fact that the employee is another physician’s patient), and both also must see the workplace in the context of what goes on at the worksite (see Section 1.6).
Such a knowledge of the workplace activity and process is a central feature of the work of the occupational hygienist, the ergonomist, and the expert in work organisation. These professionals are in short supply, and few businesses employ their own. Yet, their role is to recognise and understand the complexities of the work process, the nature of the materials used, produced, and disposed of and the methods of production. In addition, the hygienist is an expert in identifying the sources and measuring the concentrations and emissions of workplace contaminants to ensure that appropriate controls can be put in place.
The investigation of a putative link between a hazard and health effect requires a study of the populations exposed (a task for the epidemiologist), as well as a knowledge of the toxicological effects (a task for the toxicologist) with the necessary accompaniment of a risk assessment (a task for the occupational health and safety professional with experience in risk management).
Safety is often considered separately from health. This is inappropriate and counterproductive to the development and execution of an integrated health and safety strategy to protect health in the workplace. The key functions of safety management are:
- policy and planning—determining safety goals and a plan of work to achieve these goals;
- the provision of a clear basis of responsibility and communication to achieve control;
- the identification and assessment of risks and the control measures necessary to counter such risks;
- the monitoring and review of these policies and practices.
While safety engineers tend to concentrate on the mechanical aspects of the workplace process, a similar structure of activity and function could be established for all occupational health professionals.
Who does what then comes down to the resources available to the employer, as well as the hazards and risks inherent in the process. As industry becomes more fragmented, the large, company-financed, multidisciplinary teams will disappear as well. The role of independent consultant advisers will then come to the fore, but the integrated activity of several professional groups working together to achieve long-term goals could be lost. In this context, the corporate control of the company may need to take the coordinating role.
Every professional providing occupational health advice and service must ensure that they have had the relevant training by the professional bodies of their specialty which are responsible for overseeing competence. Training and education schemes are available for the main groups listed in Section 1.2 above. Furthermore, many of these bodies now insist upon programmes of continuing professional development for the career lifetime after successful completion of the examinations for competence.
1.6 Industrial processes and health outcomes
Although there has been a dramatic rise in service industries in most developed countries, manufacturing industries remain a vital part of the economy. These industries, together with the extractive process and power generation enterprises, remain the main source of concern regarding workplace exposures leading to ill health and injury.
The main industries and their health effects are summarised in Table 1.1.
Whatever the workplace activity and whoever is responsible for managing health and safety, the means of protecting the workforce can be summarised as:
- hazard identification;
- risk assessment;
- management intervention;
- control procedures;
- review and audit effectiveness.
1.7 Summary
The health of the employee at a place of work is the concern of many professional groups. There is a need to identify hazards be they physical, chemical, biological or psychosocial. Once identified, the risks to the workforce must be assessed and measures to control these risks must be instituted. Measuring the effectiveness of this process involves the monitoring of the workplace environment and the health status of the employees. Auditing the effectiveness of these measures and improving the control are never-ending processes.
The bottom line remains the health of the worker. This is what both the workers and employers desire—a healthy workforce at work. It follows that the culture of good health and safety policy and practice must pass from the professionals—and the management—to the workforce. When everyone at the workplace believes that such policies and practice are part of their responsibility, occupational health can be considered to have achieved its main goal.
1.8 The future
Such an ideal of the total ‘ownership’ of health and safety by all, managers and managed alike, may be some time distant—if it is achieved at all. Nevertheless, occupational health professionals need to be looking for the newer emphases that will emerge in the next decade, as these will influence the content and style of their work. Apart from the shifts in workforce size, skills, and structure mentioned in Section 1.3, several other influences are now beginning to emerge, which could necessitate yet more shifts in the job content of the occupational health practitioner. These are some to start thinking about:
- public safety/consumer protection;
- public risk perceptions (and effective public risk communication);
- environmental impact of workplace process;
- leisure industry risks....
Table of contents
- Cover
- Contents
- Title page
- Copyright page
- Acknowledgements
- Foreword
- 1 Introduction
- 2 Occupational Health Services—an International Perspective
- 3 Occupational Diseases
- 4 Occupational Infections
- 5 Occupational Toxicology
- 6 Occupational Hygiene—Gases, Vapours, Dusts and Fibres
- 7 Physical Hazards—Light, Heat, Noise, Vibration, Pressure and Radiation
- 8 Musculoskeletal Disorders
- 9 Psychosocial Aspects of the Workplace
- 10 Risk Assessment
- 11 Control of Air-borne Contaminants
- 12 Personal Protection of the Worker
- 13 Special Issues in Occupational Health
- 14 Legal Aspects of Occupational Health
- 15 Sources of Information
- Index