This is a test
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Book details
Book preview
Table of contents
Citations
About This Book
Neurotrauma: Managing Patients with Head Injuries is a comprehensive, holistic, evidence-based approach to the primary, secondary and tertiary care of a person with neurotrauma.
Using a patient-centred needs approach to enhance the quality of care of head injured patients, family and carers, this multidisciplinary bookenables the reader to apply the knowledge, skills and attitudes learned to the practice of neurotrauma in all settings. It explores:
- Anatomy and physiology of the brain
- Pharmacology for neurotrauma patients
- Assessment of the patient with neurotrauma
- Management of neurotrauma in a range of settings including at the scene, in the emergency department, and at the hospital
- Neuro-rehabilitation
- Community care
- Nursing management of the patient
This practical resource includes activities, exercises, and ethical and legal considerations throughout, making it ideal reading for all staff working in neuroscience, emergency, critical and rehabilitation settings.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Neurotrauma by Nadine Abelson-Mitchell in PDF and/or ePUB format, as well as other popular books in Medicine & Nursing. We have over one million books available in our catalogue for you to explore.
Information
Section 1
FOUNDATIONS FOR PRACTICE
INTRODUCTION
This book has been designed to empower health and other professionals with applicable knowledge in neurotrauma practice, to support and manage patients, families, carers and communities throughout all stages of a patient’s journey to recovery. This is accomplished using a multidisciplinary approach to facilitate recovery and maximise potential, whatever this level may turn out to be.
The management of patients with neurotrauma has improved over the last decade. This has resulted in patients, who previously would not have survived, surviving their head injuries and requiring extensive rehabilitation (House of Commons 2001). This has had a major effect on the use of available resources (Christensen et al. 2008). Services, including rehabilitation, are neither equitable nor accessible to all neurotrauma patients (Aronow 1987; Beecham et al. 2009; British Society of Rehabilitation Medicine [BSRM] 2008a; Bulger et al. 2002; RCP 2010; United Kingdom Acquired Brain Injury Forum (UKABIF) 2004; Zampolini et al. 2012). Not all patients with moderate or severe head injuries are able to access neurosurgical centres (Treacy et al. 2005). The majority go home, some with a follow-up appointment or a GP referral, others without any follow-up, yet patients requiring rehabilitation should be able to access this at any stage within their journey (RCP 2010).
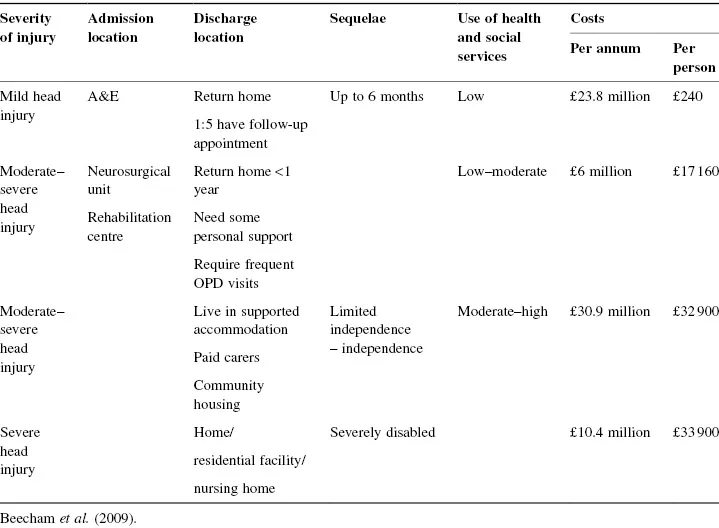
It is said that the costs for a person injured in a road traffic accident can vary between £35 000 and £60 000 per incident (Beecham et al. 2009) and costs for an injured pedestrian are estimated at £57 400 per incident (Crandall et al. 2002). The estimated cost per patient experience is presented in Table 1.
Table 1 Estimated costs for 18–25 year olds experiencing head injury.
People with neurotrauma may achieve a good recovery. However, a lack of recovery, or partial recovery, may be devastating for them, their families and communities. This book examines the journey related to health, illness and recovery, in particular for neurotrauma. In order to maximise outcome, cost-effectiveness, efficiency and quality of care, it is necessary to accompany the patient along the journey in the primary, secondary and tertiary settings.
Key Objectives
On completion of this section you should be able to achieve the following:
- Define neurotrauma.
- Define the patient’s journey.
- Describe factors that affect the patient’s journey.
- Determine how to ensure the patient has a seamless journey regarding neurotrauma.
- Evaluate the various care pathways for neurotrauma patients.
- Describe various models of wellness.
- Apply these models to neuroscience practice.
- Apply the Needs Approach Model in practice.
- Determine how using the Needs Approach Model will assist in providing holistic, patient-centred care in a multidisciplinary milieu.
- Describe effective multidisciplinary management.
- Describe the role of the neuropsychologist.
- Describe the techniques one can use to provide a therapeutic milieu.
- Manage difficult patients.
- Describe behaviour modification.
- Describe how to communicate with patients, families and carers.
Ethical/Legal Considerations
Debate the ethical issues related to this section.
Consider and apply the legal and ethical issues highlighted in these chapters to neurotrauma practice:
- Patient Charter.
- Human Rights.
- Accountability and responsibility.
- Consent.
- Confidentiality.
- Record-keeping.
Chapter 1
The Patient’s Journey
INTRODUCTION
A person is on a journey through life which runs from the ante-natal period to the time of death. It is to be anticipated that, through experience, a person can manage obstacles in their pathway and continue on their journey in a productive and positive manner. This life journey contains a number of pathways. These pathways, such as financial circumstances, interpersonal relationships and health, do not always run smoothly and may lead to various deviations. The health pathway is a continuum of wellness, illness, recovery or death and includes all occasions of ill-health.
Primary prevention is an important aspect of the patient’s journey. Preventing disease or ill-health through early education will decrease morbidity and mortality. A particular pathway along the patient’s journey commences once the patient has been diagnosed with a particular health condition/problem. Unfortunately, due to the nature of neurotrauma, there is seldom a pre-arranged plan in place as there is for elective surgery. This part of the health journey usually comes as a shock and ‘emergency resources’ may need to be called upon to be able to continue the journey. It is important to provide a smooth route throughout the patient’s journey in order to ensure that quality care is provided, decrease stress, increase compliance and decrease deviant or destructive behaviour. The patient’s journey takes place within a particular environment and involves the patient, family and the wider community. It is a journey that needs to be patient-centred and focused on the patient’s perspective, expectations, motivation and behaviour. When considering the journey the patient’s life experience, their strengths, abilities, capabilities and any fears or weaknesses must be considered. The patient’s health journey, interrupted by the neurotrauma, is influenced by a number of existing factors:
The patient:
- Age.
- Gender.
- Pre-existing conditions.
- Social practices.
- Health status.
The factors:
- Peri-natal care.
- Environment.
- Education.
- Family support.
- Community support.
Planning the patient’s journey may be referred to as ‘process mapping’ whereby the team and the patient work out the pathway a patient is expected to follow. This requires taking into account all aspects of holisitic, person-centred care that the patient may require, as well as the resources needed to achieve the proposed plan. The team is then able to examine the patient’s situation in terms of patient outcome and consider and identify potential challenges that may occur along the pathway that may hinder achievement of the patient’s goals.
CARE PATHWAYS: POLICIES AND GUIDELINES
Numerous care pathways have been developed to ensure cost-effective, efficient patient care to help create a seamless journey through this episode of altered health. Internationally, specific policies and standards have been developed that focus on neurotrauma throughout the patient’s journey (Espinosa-Aguilar et al. 2008; Seeley et al. 2006; Sesperez et al. 2001; Zampolini et al. 2012). The National Institute for Health and Clinical Excellence (NICE) (NICE 2007) has developed guidelines for the management of head-injured patients. The National Service Framework for Long-term Conditions (DH 2005a) has a particular focus on the needs of people with neurological disease and considers some of the generic issues, including rehabilitation, that are of relevance to people with long-term conditions and disabilities. The introduction of these policies addresses some of the inequities for patients requiring rehabilitation (Pickard et al. 2004).
Guidelines have been produced by a number of sources, nationally and internationally, to assist in clinical decision making, prevention, diagnosis and management, including rehabilitation, of patients with neurotrauma. Guidelines make specific practical recommendations based upon rigorous and available scientific data (RCP 2010).
The health professional is responsible and accountable for the quality of care a patient receives. Basic care in today’s climate is often protocol driven, particularly as many basic tasks are undertaken by non-professional personnel under the direct or indirect supervision of registered personnel.
INTEGRATED CARE PATHWAYS
Internationally (Espinosa-Aguilar et al. 2008; Seeley et al. 2006; Sesperez et al. 2001) and nationally (BSRM 2002; BSRM 2008a; 2009; NICE 2007; Royal College of Physicians [RCP] and BSRM 2003) interprofessional, integrated care pathways have been developed to improve the management of patients with neurotrauma and are useful in managing specific issues such as depression (Turner-Stokes et al. 2002).
The National Service Frameworks stress the importance of integrated care pathways in the development of quality healthcare. These pathways, if developed and implemented effectively, will increase interprofessional co-ordination, efficiency of healthcare, reduce sequelae of head injury and reduce healthcare costs (Coetzer 2009; Singh et al. 2012; Vitaz et al. 2001; Zampolini et al. 2012).
Figure 1.1 Care pathway for traumatic brain injury (RCP 2010: p. 28).
Reproduced from: Royal College of Physicians. Medical rehabilitation in 2011 and beyond. Report of a working party. London, RCP, 2010. Copyright © 2010 Royal College of Physicians. Reproduced by permission.
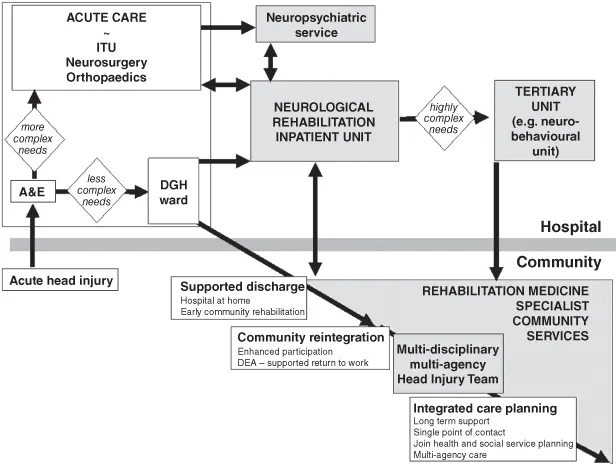
Figure 1.2 The ‘Slinky’ model of phased rehabilitation (RCP and BSRM 2003: p.10).
Reproduced from: Royal College of Physicians and British Society of Rehabilitation Medicine. Rehabilitation following acquired brain injury: National clinical guidelines (Turner-Stokes, L. ed). London, RCP, BSRM, 2003. Copyright © 2003 Royal College of Physicians. Reproduced by permiss...
Table of contents
- Cover
- Title page
- Copyright page
- Preface
- Dedication
- Acknowledgements
- Contributor Details
- Abbreviations
- List of Tables and Figures
- Section 1: FOUNDATIONS FOR PRACTICE
- Section 2: PRE-REQUISITE KNOWLEDGE
- Section 3: FEATURES OF NEUROTRAUMA
- Section 4: MANAGEMENT OF NEUROTRAUMA
- Section 5: NEUROREHABILITATION
- Section 6: APPENDICES
- Activity Answers
- Additional Resources
- Glossary
- References
- Index