This is a test
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Book details
Book preview
Table of contents
Citations
About This Book
The Care of Wounds addresses all aspects of holistic wound management. The fourth edition of this successful clinical text continues to reflect current research and evidence-based practice, while incorporating the considerable developments which have occurred in wound care practice since the previous edition. It includes chapters on the physiology of wound healing, general principles of wound management, wound management products, and the management of patients with both acute and chronic wounds. The title is an essential read for all nurses and healthcare professionals working in the field of tissue viability and wound healing.
- Comprehensive and clinically-oriented
- Examines best practice in wound management
- Incorporates national and international clinical guidelines where applicable
- Superbly illustrated with full colour throughout
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access The Care of Wounds by Carol Dealey in PDF and/or ePUB format, as well as other popular books in Medicine & Nursing. We have over one million books available in our catalogue for you to explore.
Information
Chapter 1
The Physiology of Wound Healing
Introduction
Wound healing is a highly complex process. It is important that the nurse has an understanding of the physiological processes involved for several reasons:
- understanding the physiology of skin assists in understanding the healing process;
- an understanding of the physiology of wound healing makes it possible to recognise the abnormal;
- recognition of the stages of healing allows the selection of appropriate dressings;
- understanding of the requirements of the healing process means that appropriate nutrition can, as far as is possible, be given to the patient.
Definitions Associated with Wounds
Any damage leading to a break in the continuity of the skin can be called a wound. There are several causes of wounding:
- traumatic – mechanical, chemical, physical;
- intentional – surgery;
- ischaemia – e.g. arterial leg ulcer;
- pressure – e.g. pressure sore.
In both traumatic and intentional injury there is rupture of the blood vessels, which results in bleeding followed by clot formation. In wounds caused by ischaemia or pressure the blood supply is disrupted by local occlusion of the microcirculation. Tissue necrosis follows and results in ulcer formation, possibly with a necrotic eschar or scab.
Wounds in the skin, or deeper have been labelled in various ways. Some of them can be described as follows.
(1) Partial- and full-thickness wounds
- A partial-thickness wound is one where some of the dermis remains and there are shafts of hair follicles or sweat glands.
- In a full-thickness wound all the dermis is destroyed and deeper layers may also be involved.
(2) Healing by first and second intention
- These definitions were first described by Hippocrates around 350 BC.
- Healing by first intention is when there is no tissue loss and the skin edges are held in apposition to each other, such as a sutured wound.
- Healing by second intention means a wound where there has been tissue loss and the skin edges are far apart, such as a leg ulcer.
(3) Open and closed wounds
- These are the same as healing by second and first intention respectively.
The Structure of the Skin
The skin is the largest and one of the most active organs of the body. It is composed of two layers: the epidermis and dermis with the epidermis forming the outer surface of the body and the dermis forming the deeper layer of the skin. The main structures of the skin can be found in the dermis. Figure 1.1 shows a cross-section of the skin.
Figure 1.1 A cross-section of the skin
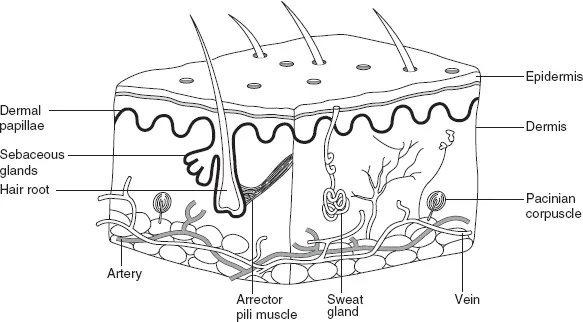
Dermis
Dermis is composed of connective tissue, both collagen and elastic fibres, which is both elastic and resilient and provides support for the structures in the dermis. Blood vessels, lymph vessels, sensory nerve endings, sweat and sebaceous glands and hair follicles can be found within the dermis. The ducts of the glands and hair shafts pass through the epidermis to the skin surface. Sweat glands have their own ducts opening on the skin surface, but sebaceous glands open onto the hair follicles. The base or bulb of hair follicles is sited deep into the dermis. They are lined with epithelial cells and can play a role in the healing of partial-thickness wounds.
The surface of the dermis where it interlocks with the epidermis is irregular with projections of cells called papillae. The base of the dermis is less clearly defined as it blends into subcutaneous tissue, which contains both connective tissue and adipose tissue and helps to anchor the skin to muscle and bone.
Epidermis
The epidermis comprises several layers of cells. The deepest layer is the stratum basale and it is constantly producing new cells by cell division. These cells are gradually pushed towards the skin surface taking about 7 weeks to reach the surface. The stratum spinosum contains bundles of keratin filaments, which hold the skin together. The top three layers of epidermis are the stratum granulosum, which produces the precursor to keratin, the stratum lucidum and the stratum corneum. As they move through the strata, the cells gradually flatten and the protoplasm becomes replaced with keratin. The cells in the stratum corneum are flat with no nucleus and are essentially dead cells. They are constantly worn away and replaced by new cells moving to the surface.
In addition the epidermis has cells called melanocytes, which contain melanin that gives skin its colour. A high concentration of melanin produces a dark skin colour. Ultraviolet light increases melanin production. This may occur naturally by sunlight resulting in a suntan or artificially such as a treatment in dermatology.
Wound Healing
The wound healing process consists of a series of highly complex interdependent and overlapping stages. These stages have been given a variety of names. They are described here as:
- inflammation;
- reconstruction;
- epithelialisation;
- maturation.
The stages last for variable lengths of time. Any stage may be prolonged because of local factors such as ischaemia or lack of nutrients. The factors that can delay healing are discussed in more detail in Chapter 2.
Inflammation
The inflammatory response is a non-specific local reaction to tissue damage and/or bacterial invasion. It is an important part of the body's defence mechanisms and is an essential stage of the healing process. The signs of inflammation were first described by Celsus, in the first century AD, as redness, heat, pain and swelling. The factors causing them are shown in Table 1.1.
Table 1.1 The signs of inflammation
| Signs and symptoms | Physiological rationale |
| Redness | Vasodilation results in large amount of blood in the area |
| Heat | Large amount of warm blood and heat energy produced by metabolic reactions |
| Swelling | Vasodilation and leakage of fluid into the wound area |
| Pain | May be caused by damage to nerve ends, activation of the kinin system, pressure of fluid in the tissues or the presence of enzymes, such as prostaglandins, which cause chemical irritation |
When there is traumatic or intentional injury that causes damage to the blood vessels, the first response is to stop the bleeding. This is achieved by a combination of factors. First, by vasoconstriction that reduces the blood flow and second by the release of a plasma protein called von Willebrand factor from both endothelial cells and platelets, resulting in platelet aggregation and formation of a platelet plug. The third factor is the initiation of the clotting cascade and the development of a fibrin clot to reinforce the platelet plug.
Hageman factor (factor XII in the clotting cascade) triggers both the complement and kinin systems. The complement system consists of plasma proteins, which are inactive precursors. When activated, there is a cascade effect that leads to the release of histamine and serotonin from the mast cells and results in vasodilation and increased capillary permeability. The complement system also assists in attracting neutrophils to the wound. The complement molecule, C3b, acts as an opsonin, that is, it assists in binding neutrophils to bacteria. Five of the proteins activated during the cascade process form the membrane attack complex, which has the ability to directly destroy bacteria.
The effect of the complement system is enhanced by the kinin system, which, through a series of steps, activates kininogen to bradykinin. Kinins attract neutrophils to the wound, enhance phagocytosis and stimulate the sensory nerve endings. The apparent delay in feeling pain after injury is explained by the short time lag taken for the kinin system to be activated.
As the capillaries dilate and become more permeable, there is a flow of fluid into the injured tissues. This fluid becomes the ‘inflammatory exudate’ and contains plasma proteins, antibodies, erythrocytes, leucocytes and platelets. As well as being involved in clot formation, platelets also release fibronectin and growth factors called platelet-derived growth factor (PDGF) and transforming growth factor alpha and beta (TGFα and TGFβ). Their role is to promote cell migration and growth at the wound site.
Growth factors are a subclass of cytokines, proteins that are used for cellular communication (Greenhalgh, 1996). The particular role of growth factors is to stimulate cell proliferation. There are a number of growth factors involved in the healing process, and they are listed in Table 1.2. Some growth factors have been isolated and used as a treatment for chronic wounds. This will be discussed in more detail in Chapter 4.
Table 1.2 Growth factors involved in the healing process
| Growth factor | Abbreviation | Action |
| Platelet-derived growth factor | PDGF | Chemotactic for neutrophils, fibroblasts and, possibly, monocytes. Encourages proliferation of fibroblasts |
| Transforming growth factor alpha | TGFα | Stimulates angiogenesis |
| Transforming growth factor beta | TGFβ | Chemotactic for monocytes (macrophages). Encourages angiogenesis. Regulates inflammation |
| Fibroblast growth factor | FGF | Stimulates fibroblast proliferation and angiogenesis |
| Epidermal growth factor | EGF | Stimulates the proliferation and migration of epithelial cells |
| Insulin-like growth factors | IGF-I, IGF-II | Promote protein synthesis and fibroblast proliferation. Work in combination with other growth factors |
| Vascular endothelial growth factor | VEGF | Critical for angiogenesis and the formation and growth of blood vessels |
The first leucocyte to arrive at the wound is the neutrophil. Fibronectin attracts neutrophils to the wound site, ...
Table of contents
- Cover
- Title Page
- Copyright
- Dedication
- Preface
- Chapter 1: The physiology of wound healing
- Chapter 2: The management of patients with wounds
- Chapter 3: General principles of wound management
- Chapter 4: Wound management products
- Chapter 5: The management of patients with chronic wounds
- Chapter 6: The management of patients with acute wounds
- Chapter 7: The organisation of wound management
- Index