![]()
Chapter 1
Epidemiology of Chronic Pain
Blair H Smith and Nicola Torrance
Medical Research Institute, University of Dundee, Dundee, UK
Overview
Chronic pain persists beyond normal wound healing, with around one in four adults suffering from chronic pain
The majority of patients with chronic pain will be managed in the primary care setting, but complex cases will require specialist input
Chronic pain, especially neuropathic pain, has a major impact on all aspects of general health
Factors predisposing to chronic pain include those not amenable to intervention, such as increasing age and female gender, and also those that can be targeted, such as deprivation, or poor acute pain control
Early identification and management of chronic pain are essential in order to minimise long term suffering and disability
Introduction
Pain is an individual experience, whose subjective nature makes it difficult to define, describe or measure, yet which is common to all human beings. As description and measurement are nonetheless essential, so, therefore, is a definition that suits both patients and professionals. Pain is helpfully, therefore, defined by the International Association for the Study of Pain (IASP) as ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described by the patient in terms of such damage’.
Chronic pain is defined by the IASP as ‘pain that persists beyond normal tissue healing time’. A range of factors may be involved, including physical and biological factors, and also behavioural and cognitive factors, and these may dominate the experience of chronic pain, which is ultimately primarily subjective (Box 1.1).
Box 1.1 Acute and Chronic Pain
| Acute pain | → → → → → → | Chronic pain |
| Physiological | | Pathological |
| Health preserving | | Maladaptive |
| Warns of damage | | Dysfunctional healing |
| Allows evasive action | | Abnormal response to injury |
What is Chronic Pain?
There are many similarities in the symptoms and impact of chronic pain between most individuals who experience chronic pain, irrespective of its cause. Consequently, there are also many similarities in approaches to preventing or managing chronic pain of different aetiological or diagnostic backgrounds. This has led some to propose the existence of a ‘chronic pain syndrome’, and certainly for many clinical and research purposes, there is considerable merit in regarding chronic pain as a single, global, clinical entity (while also paying suitable attention to individual, treatable causes of chronic pain).
Why is Epidemiology Important?
Epidemiology is ‘the study of the distribution and determinants of health-related states or events in specified populations and the application of this study to control health problems’.
(Last RJ. (2001) A Dictionary of Epidemiology, 4th edn. Oxford: International Epidemiological Association.)
It is the latter part of this definition that makes it such an important science in clinical medicine. The last twenty or so years have seen the publication of many good quality epidemiological studies of chronic pain that have enhanced our understanding of its causes, impact and approaches to management. Good epidemiological research on chronic pain can, and does, provide important information on its classification and prevalence and factors associated with its onset and persistence. This can inform the design and targeting of treatment and preventive strategies (Box 1.2).
Box 1.2 How Does Epidemiology Help Us with Chronic Pain?
1. Identifies factors associated with chronic pain and those which lead to or favour chronicity
2. Aids development of interventions to prevent chronicity or to minimise its impact
3. Improving understanding of associated factors in development will inform the clinical management of the condition, thereby possibly limiting severity and minimising disability
4. Understanding how chronic pain impacts on quality of life and what associated factors have greatest adverse effect (e.g. physical, psychological or social)
5. Understanding the distribution of chronic pain can help to target appropriate management strategies at the subgroups most likely to benefit, and individuals with less severe chronic pain might be identified with a view to prevention of exacerbation
6. Evaluation of treatment strategies: Until the distribution, determinants, impact and natural history of chronic pain are understood, it is impossible to evaluate properly any intervention aimed at improving chronic pain
7. Allocation of health service resources: Ideally this should be informed by robust epidemiological data. With a condition of the importance of chronic pain, it is crucial that research information is available for health service planning
8. Allocation of educational resources: As with financial and clinical resources, appropriate education of professionals and patients can be greatly assisted by epidemiological study
Source: Adapted from Smith, BH, Smith, WC & Chambers, WA. (1996) Chronic pain – time for epidemiology. Journal of the Royal Society of Medicine, 89, 181–183
How Common is Chronic Pain?
The prevalence of chronic pain depends on exactly where, when and how it is measured. There is no universally agreed cut-off point between acute and chronic pain, but in the absence of other information, three months is often taken as the point beyond which ‘normal tissue healing’ should have taken place, and when pain therefore becomes chronic. Around one in four or five adults is currently experiencing chronic pain. A comprehensive literature review found a weighted mean prevalence of chronic pain of 25.9%. This is broadly similar to a large European study of over 46 000 people using a 6-month cut-off point (19.0%), and other systematic reviews.
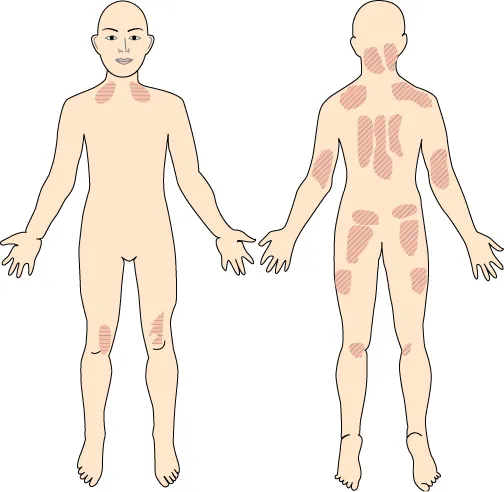
Some studies have examined more severe, perhaps more clinically relevant, chronic pain. For example, ‘chronic widespread pain’ (bilateral pain above and below the waist, including the axial skeleton) has consistently been found to affect at least 5% of adults, and perhaps more than 11% (Figure 1.1).
A similar prevalence (5%) has been found for ‘severe chronic pain’ (intense, highly disabling, severely limiting pain). Pain with neuropathic features (which is often more severe and harder to treat than other pain) probably affects at least 6–8% of the population. These figures are similar to the prevalence rates of well-recognised conditions such as ischaemic heart disease and diabetes, for which health service resources are readily found. Chronic pain, however, generally attracts less attention and resource (perhaps because it is often regarded as a heterogeneous group of conditions, or as a symptom, rather than as a global entity requiring a global response) (Figure 1.2).
The commonest location of chronic pain is in the back, followed by the large joints (kne...