
eBook - ePub
Antiplatelet Therapy in Cardiovascular Disease
This is a test
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Antiplatelet Therapy in Cardiovascular Disease
Book details
Book preview
Table of contents
Citations
About This Book
Edited by a team of the world's leading interventional cardiologists and educators, this new book is created with an eye to giving the reader a solid, practical, and clinically focused understanding of this important class of drugs, from basic science to a clear-headed discussion of complex topics such as combination therapies, drug-to-drug interactions, and resistance to antiplatelet agents.
This important new book:
- Begins with a concise but thorough discussion of platelet biology and pathophysiology so that readers understand how antiplatelet agents work and why they produce such a varied range of complications, from minor GI upset to potentially life-threatening conditions such as neutropenia, a critical shortage of white blood cells.
- Thoroughly covers platelet function testing, including novel techniques.
- Clarifies current best practice regarding the use of antiplatelet agents in both chronic and acute cardiovascular disease.
- Reviews all types of antiplatelet agents – from aspirin to recently approved drugs – including indications, clinical outcomes, and side effects.
Written by an international "who's who" of experts in the field, Antiplatelet Therapy in Cardiovascular Disease also includes an entire section covering the use of antiplatelet drugs in PCIs, including percutaneous valve repair, which makes this text particularly essential to interventional cardiologists.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Antiplatelet Therapy in Cardiovascular Disease by Ron Waksman, Paul A. Gurbel, Michael A. Gaglia in PDF and/or ePUB format, as well as other popular books in Medicine & Cardiology. We have over one million books available in our catalogue for you to explore.
Information
Section III
Antiplatelet pharmacology
13
Aspirin
Karsten Schrör and Thomas Hohlfeld
UniversitätsKlinikum, Heinrich-Heine Universität Düsseldorf, Düsseldorf, Germany
Aspirin is the first-choice antiplatelet agent in cardiocoronary prevention and an essential constituent of dual antiplatelet therapy. The reasons are its unique pharmacological mode of action; the long-lasting, more than 60 years, experience with its use as an antiplatelet agent; and the reliability of its pharmacological action in more than 95% of patients.
Mode of antiplatelet action
Aspirin, in contrast to most other antiplatelet drugs, is not a platelet-specific agent but exhibits a broad spectrum of biological activities on many cellular targets [1]. At low doses (≤300 mg), aspirin inhibits platelet-dependent prostaglandin-endoperoxide (PGEP) formation via irreversible acetylation of COX-1. This results in downstream inhibition of thromboxane A2 (TXA2) formation, the only significant PGEP end product in platelets. This COX-1-mediated inhibition of prostaglandin formation is the generally accepted mode of antiplatelet action of aspirin [2, 3].
Consequently, measurement of platelet-dependent thromboxane formation, for example, by determining thromboxane-forming capacity in serum ex vivo or in vitro, is a simple and specific means to determine the pharmacological potency of aspirin as an antiplatelet drug on an individual basis. Because of the nonlinearity between thromboxane levels and thromboxane-related platelet stimulation, this inhibition has to be apparently complete, that is, >95% in terms of serum capacity, to become effective. This degree of inhibition is obtained in the vast majority of patients, while only 1–2% remain pharmacologically “resistant” against aspirin. Thus, the much more variable clinical efficacy of aspirin in preventing atherothrombotic cardiovascular events is due to variable environmental conditions of circulating platelets including platelet stimuli, which might or might not require platelet-dependent thromboxane formation as an amplifying event.
Accordingly, the antiplatelet potency of aspirin in vivo is critically determined by the significance of thromboxane generation for platelet activation. This largely depends on the stimulus. Aspirin does not modify ADP-induced platelet aggregation and alpha-granule secretion in native blood. Nor does it prevent platelet aggregation induced by thrombin, shear stress, or other thromboxane-independent pathways of platelet activation.
The initial “explosion” of platelet-dependent thromboxane formation after appropriate stimuli starts platelet activation, secretion, and aggregate formation. However, the subcellular targets of thromboxane in platelets and their interactions are still not completely understood. At least theoretically, it is likely that thromboxane per se rather acts as a platelet-derived amplification factor for further platelet recruitment and activation than being a direct stimulus for platelet secretion [4, 5]. There is considerable clinical and experimental evidence for aspirin-sensitive, thromboxane-dependent thrombin formation, which occurs at the surface of activated platelets and connects platelet activation with the plasmatic clotting process [6, 7, 8, 9].
Time dependency of inhibition of platelet function by aspirin
If rapid inhibition of platelet function is required, that is, as an emergency first-line treatment in acute coronary syndromes, a loading dose of 250–500 mg soluble aspirin, for example, as lysine salt, can be administered IV. This results in sufficient (≥99%) inhibition of thromboxane formation within 5 min. For oral dosing of 500 mg, at least 40 min is required for a comparable effect [10] (Figure 13.1). After oral administration, more time is necessary to obtain the required pharmacological effect. At least two to three daily doses (e.g., 75–325 mg) of standard aspirin are necessary to obtain sufficient inhibition of thromboxane formation. Once sufficient acetylation is obtained, only a maintenance dose of aspirin per day is necessary.
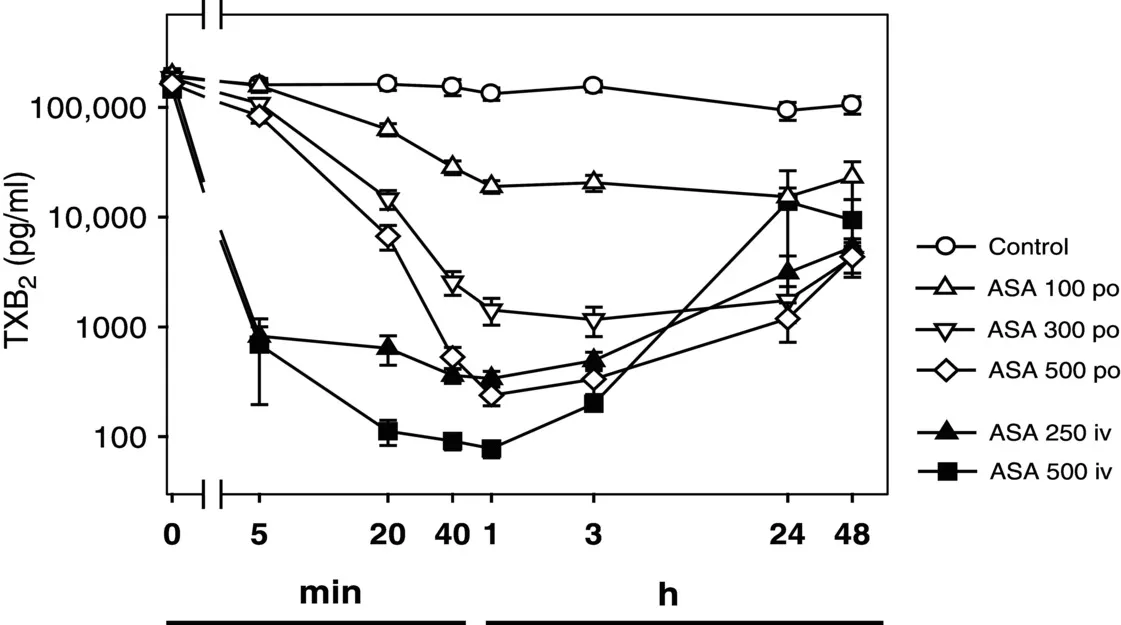
Figure 13.1 Time-dependent inhibition of thromboxane (TXB2) formation by aspirin, depending on dose (mg) and route of administration. Data were obtained from 21 healthy subjects treated in a crossover design. Note that both axes are in logarithmic scale.
(Source: Adapted from Schrör, K 2009 [1]. Reproduced with permission of John Wiley & Sons Ltd.)
The inhibition of platelet COX-1 and platelet function by aspirin is functionally antagonized by the 10–15% fresh platelets that enter the circulation every day from the bone marrow. In certain clinical conditions with a more rapid platelet turnover rate, that is, diabetes or extracorporeal circulation, the efficacy and duration of the antiplatelet effect of aspirin might be reduced. A nearly complete recovery of (arachidonic acid-induced) platelet aggregation is seen about 3 days after aspirin withdrawal, but more than 10 days are required to fully restore plasma thromboxane levels [11]. This confirms that a small recovery, that is, 10–15%, even a small recovery of thromboxane formation is sufficient for a functionally significant thromboxane-induced platelet response.
Dose-dependent inhibition of platelet function by aspirin
No other issue in aspirin research has been discussed more intensively than the question of the optimal antithrombotic dose – frequently though not necessarily correct – considered to be equivalent with the antiplatelet dose. Oral single doses of 325, 162, and 75 mg aspirin result in peak plasma aspirin levels of 10.7, 6.8, and 0.3 μM, which are sufficient for inhibition of platelet function [12]. Currently, there is general agreement that daily doses of 100 mg aspirin are sufficient to inhibit platelet-dependent thromboxane formation in most patients. Somewhat higher doses may be required if enteric-coated preparations are used, possibly due to a lower systemic bioavailability of aspirin [13].
The large retrospective meta-analyses of randomized trials by the Antiplatelet Trialists suggest that daily aspirin doses between 75 and 325 mg will have a similar clinical potency with respect to secondary prevention of cardiovascular events. While this might be true, there are large disease-related differences between different groups of patients, and it is not finally established whether the full-spectrum antithrombotic activity of aspirin is seen at the same dose in all patients. It is also not known whether thromboxane-independent actions of aspirin contribute to the clinical outcome, such as inhibition of inflammatory cytokines [14], actions on endothelial function [15, 16], and endothelial NO synthesis [17]. Interestingly, high-...
Table of contents
- Cover
- Title page
- Copyright page
- List of Contributors
- Foreword
- Preface
- Section I: Platelet biology and Pathophysiology
- Section II: Platelet Function Tests
- Section III: Antiplatelet pharmacology
- Section IV: Percutaneous Coronary Intervention and Antiplatelet Therapy
- Section V: Antiplatelet Responsiveness
- Index
- End User License Agreement