![]()
Section II: Assessment, Interpretation and Management of Specific Problems in the Neurological Patient
7
Assessment and Management of Raised Intracranial Pressure
Ann-Marie Mestecky
INTRODUCTION
A number of intracranial conditions can cause an increase in intracranial pressure (ICP). The increase can occur either suddenly, e.g. following an intracranial haemorrhage, or gradually, e.g. with a slow growing brain tumour. Any pathological process that causes an increase in volume of one or more of the intracranial components (cerebrospinal fluid (CSF), cerebral blood, brain tissue) or a mass lesion, will result in an increase in ICP when the intracranial compensatory mechanisms have been exhausted. ICP is generally regarded as raised when ICP is greater than 20 mmHg, and interventions to reduce ICP are generally instituted when ICP reaches this level.
Nursing patients with raised ICP requires an understanding of the concepts presented in the previous chapter, as well as a knowledge of the signs and symptoms of raised ICP, the current evidence to support nursing interventions and the treatment options that are available. With this knowledge the nurse is better equipped to interpret assessment data, to plan evidence based care and to make effective decisions which ultimately could affect the outcome of the patient.
There are a number of different measures to treat raised ICP, all of which aim to reduce the volume of one or more of the three intracranial components. Most of the recommendations for the management of raised ICP have evolved from research involving patients with traumatic brain injuries (TBI). The specific management of raised ICP for this patient group is similar to that for other pathologies that give rise to raised ICP, however there are some exceptions. Where specific recommendations for other pathologies exist, e.g. spontaneous intracerebral haemorrhage, it will be clearly stated within the text. Otherwise it can be assumed that each of the measures/treatments presented in this chapter are instituted to treat raised ICP regardless of pathology.
CAUSES OF RAISED ICP
There are a number of pathological processes that can result in raised ICP which include:
- Brain oedema
- Hydrocephalus
- Vascular engorgement
- Mass lesions
- Idiopathic intracranial hypertension (IIH) also known as benign intracranial hypertension (see Chapter 25)
Brain oedema
Brain oedema is an increase in fluid in either the intracellular and/or interstitial spaces in the brain; the resulting increase in brain volume can cause an increase in ICP. Oedema can be localised or generalised. There are four types of cerebral oedema: vasogenic, cytotoxic (cellular), interstitial and hypo-osmolar (osmotic).
Vasogenic oedema
This type of oedema occurs due to disruption to the integrity of the blood–brain barrier (BBB). The loosening of the tight junctions between endothelial cells of the cerebral capillaries results in the BBB becoming more permeable. A protein rich fluid enters freely from the blood into the interstitial fluid of the brain, causing vasogenic oedema. It has been hypothesised that the breakdown in the BBB is caused by mediator substances released or generated within necrotic brain tissue (Unterberg and Sarrafzadeh, 2000).
Newly formed capillaries that supply blood to brain tumours lack the tight junctions that are integral to a functioning BBB and this can also lead to vasogenic oedema. Vasogenic oedema typically surrounds cerebral tumours, particularly malignant gliomas and metastatic tumours. It is also found surrounding cerebral abscesses. Vasogenic and cytotoxic oedema often co-exist following stroke and traumatic brain injury. Vasogenic oedema primarily affects the white matter because the cells are less tightly packed than in the grey matter; the white matter therefore offers less resistance to the accumulation of fluid.
Cytotoxic (cellular) oedema
The movement of water between intracranial fluid spaces in the brain is largely determined by the movement of sodium. Water will move by osmosis in the direction where sodium is most concentrated. The sodium–potassium (Na+- K+) pumps within the cell membranes (refer to Chapter 1) are dependent on a continual supply of oxygen to maintain their function of moving sodium (Na+) out of the cells and moving potassium (K+) in against their concentration gradients. When there are insufficient energy substrates available to power the Na+- K+ pumps, e.g. due to ischaemia, Na+ rapidly accumulates inside the cells and water follows by osmosis. This increase in cellular volume is called cytotoxic or cellular oedema.
Another cause for influx of Na+ into the cells is the increase in the neurotransmitter, glutamate, in the interstitial fluid. This occurs following traumatic brain injury and ischaemia (Kimelberg, 1995). Glutamate triggers the opening of Na+ channels, with subsequent influx of Na+ and water. In addition, more energy is utilised by the cells to reduce the concentration of glutamate in the interstitial space; this mopping up operation of glutamate reduces the available energy to power the Na+- K+ pumps. Irrespective of the cause for the influx of Na+, the subsequent accumulation of water inside the cells causes them to swell. Cytotoxic oedema is common following cerebral hypoxia, ischaemia and TBI. The grey and white matter are equally affected.
Interstitial oedema
Interstitial oedema is associated with hydrocephalus. When the pressure in the ventricles is increased, the CSF is forced out through the lining of the ventricles into the surrounding white matter.
Hypo-osmolar (osmotic) oedema
Water diffuses easily across the BBB and is largely determined by osmolar forces. Hypo-osmolar oedema occurs when the serum osmolality falls acutely below normal levels. The hypo-osmolality of the blood leads to the movement of water by osmosis across the BBB into the interstitial fluid of the brain. The most common causes are the syndrome of inappropriate secretion of anti diuretic hormone (SIADH), and the administration of excessive volumes of 5% glucose resulting in dilutional hyponatraemia and a fall in plasma osmolality. If changes in serum osmolality occur slowly the hypo-osmolar state is less likely to cause oedema due to the fact that the brain can compensate for the gradual change (see Chapter 16).
Hydrocephalus
Any abnormality affecting the production, circulation or absorption of CSF may result in hydrocephalus. The excessive volume of CSF causes an increase in ICP.
Vascular engorgement
Vascular engorgement is a less common cause for an increase in ICP. Any pathological process that obstructs venous drainage of the intracranial vault will result in an increase in cerebral blood volume (CBV) with a subsequent increase in ICP. Tumours that compress or invade the large venous sinuses, e.g. meningiomas, will obstruct venous outflow, as will a large thrombosis of a venous sinus, e.g. sagittal sinus thrombosis.
Vascular engorgement can also occur with severe hypoxia and hypercapnia because they both cause dilation of the cerebral vasculature resulting in a significant increase in cerebral blood volume.
Mass lesions
Mass lesions can be slow growing, e.g. meningiomas, or rapidly expanding, e.g. intracranial haematomas. Mass lesions include tumours, haematomas and abscesses.
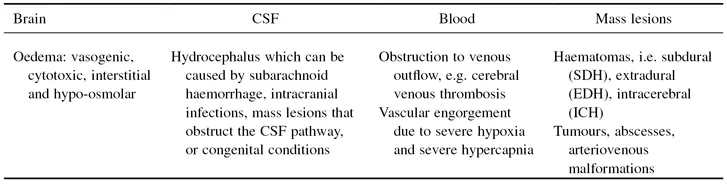
Summary of the causes of ICP
Table 7.1 provides a summary of specific causes of raised ICP categorised by the component of the intracranial cavity that is primarily affected.
Table 7.1 Causes of increased intracranial pressure (ICP).
SIGNS AND SYMPTOMS
The signs and symptoms of raised ICP will differ according to the speed with which the ICP increases and in the case of mass lesions, their location. When acute increases in intracranial volume occur as for example with acute intracranial haematomas, the compensatory mechanisms that usually maintain homeostasis of ICP become overwhelmed and signs and symptoms that indicate the patient’s condition is critical will be apparent. In patients with intracranial lesions that are slow growing, particularly those in non functional areas, the signs and symptoms will progress slowly and be more subtle.
Because of the compensatory mechanisms and the visco-elastic properties of the brain (see Chapter 6) a slow growing mass lesion will often grow to a considerable size before the symptoms become apparent. However, if the lesion is enlarging in an eloquent (functional) area of the brain then the patient will be symptomatic earlier due to direct compression and disruption of the local functional tissue and its blood supply, irrespective of whether there is an increase in ICP or not.
It is essential for the neuroscience nurse to recognise and interpret signs and symptoms of a rising ICP to enable early and appropriate measures to be taken.
Early signs and symptoms
Early signs and symptoms are commonly associated with gradual increases in intracranial volume, for example with tumours, abscesses, and hydrocephalus. Early signs include:
- Headache, which is usually worse in the morning and increases in severity with coughing, straining and bending
- Vomiting, usually in the morning often without nausea and can progress to projectile vomiting
- Papilloedema, which is swelling of the optic disc. The raised ICP is transmitted from the subarachnoid space through to the optic nerve sheath which impedes venous drainage from the retina resulting in the capillaries becoming tortuous and dilated. This congestion and dilatation of the retinal blood vessels results in a swollen optic disc often with superficial retinal haemorrhages. Papilloedema will eventually lead to blurring of vision and in rare cases loss of vision can occur. Papilloedema will not usually be present if the ICP is of recent onset, i.e. within 24 hours
- Seizures
- Focal neurological signs can occur, but are not necessarily due to raised ICP. They can be due to the mass lesion directly compressing functional tissue and its blood supply, e.g. a lesion compressing Broca’s area will result in dysphasia which can occur without an increase in ICP
Later signs and symptoms
Pathologies that result in sudden increases in ICP and slow growing lesions that are left untreated can develop the following:
- Decrease in level of consciousness, which can occur due to the distortion and compression of anatomic structures related to consciousness and/or as a result of a compromised cerebral perfusion pressure (CPP). As ICP increases it becomes more difficult for blood to flow into the brain, the CPP subsequently falls and the brain has insufficient substrates to maintain normal neuronal function.
- Seizures.
- Changes in the pupil size and the reaction of the pupils to light as a direct result of compression of the oculomotor nerve/s (cranial nerve III) (discussed below).
- Other specific signs and symptoms associated with herniation of the brain which are presented below.
Herniation syndromes
When the intracranial vault has reached maximum capacity and can no longer accommodate any further increase i...