This is a test
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Health Behavior Change in the Dental Practice
Book details
Book preview
Table of contents
Citations
About This Book
Health Behavior Change in the Dental Practice presents an overview of health behavior change, focusing on the spirit of motivational interviewing. Targeting the clinical application of the principles, the book applies lessons learned from the field of general and behavioral medicine to the dental practice. By presenting a series of clinical examples and accompanying dialogue, the book guides the reader in using motivational interviewing techniques as tools for oral hygiene education, tobacco use cessation, and dietary counseling. Health Behavior Change in the Dental Practice supports the trend towards risk management in oral health care, offering practical guidance to promote health behavior change in patients.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Health Behavior Change in the Dental Practice by Christoph Ramseier, Jean E. Suvan in PDF and/or ePUB format, as well as other popular books in Medicine & Dentistry. We have over one million books available in our catalogue for you to explore.
Information
CHAPTER 1
INTRODUCTION TO HEALTH BEHAVIOR CHANGE FOR THE DENTAL PRACTICE
Christoph A. Ramseier, Jean Suvan, Angela Fundak, and Philip S. Richards
HEALTH CARE IN THE TWENTY-FIRST CENTURY
Health professionals working in this century are presented with a unique combination of patient care scenarios. The unprecedented advances in the development of scientific knowledge, means of knowledge dissemination, clinical skills application, public health initiatives, and workforce diversity are well recognized in today’ s health care environment. However, many additional factors influence the opportunity for patients and clinicians alike to achieve the goal of attaining health and continued wellness. Some of these may be derived from catastrophic events associated with the conflicts of war, natural disasters, and critical socio- economic factors. Others are more reflective of circumstances for individuals and the lifestyle choices they make throughout their lifetime. In many situations, health status is not a result of the influence of a single element working in isolation. It is more likely that we see a number of components present in the overall environment in which the patient chooses to exist. The acknowledgement of the potential impact of a variety of influences on health status allows the health professional to work with the patient to understand the individual approach for optimal wellness. As oral health professionals, this recognition is integral to the future development of patient care plans that are not limited to treating the signs and symptoms of common dental diseases.
There is increasing evidence suggesting oral health status can affect general health and quality of life in people of all ages. Most oral diseases are common chronic diseases and are momentous public health issues with a high prevalence across all populations worldwide. Some of the etiologies of oral diseases are well known. They include (1) the causal factors induced by oral biofilms, and (2) the lifestyle risk factors common to a number of chronic diseases: insufficient oral hygiene, tobacco use, diet, behaviors causing injuries, and stress. All of these elements are modifiable and associated with the influence of health behaviors as determinants of disease prevalence.
As we are living in a century of heightened awareness of chronic diseases, health care challenges are becoming more diverse, with an increasing percentage of the population in the developed world being diagnosed with health decline associated with “lifestyle” behaviors. Therefore, the health professional is continuously presented with a dual focus — control of current disease while facilitating the understanding of continuous self- management as part of an effective and equitable long-term solution. Oral health professionals are not exempt from this approach to patient care as we continue our efforts to manage common oral diseases as a chronic condition rather than simply treating the sequelae of acute episodes. This introductory chapter sets the stage for this book through a discussion of past, current, and future understanding of the dental clinician as a health professional supporting the promotion of total health rather than a provider of operative dentistry alone.
There is substantial evidence that oral health can be maintained by ade- quate behaviors such as regular oral hygiene, avoidance of tobacco, and consumption of a healthy diet. Future public health policies should be reoriented to incorporate oral health practices recommending behavioral support and the common risk factor approach for health promotion. Oral health care professionals should gain an understanding of the health effects of inappropriate behaviors in order to successfully target prevention and disease control. As a consequence, services for primary and secondary prevention on an individual level oriented toward the change of inappropriate behavior will become a professional responsibility for all oral health care providers.
From a practical point of view, it may be preferable to apply methods for health behavior change counselling in oral care that are shown to be effective in both primary and secondary prevention of oral diseases. These methods should be
- based on the best available evidence,
- applicable to oral hygiene behavior, tobacco use prevention and cessation, and dietary counselling, and
- suitable for implementation by the dental practice team in a cost- effective way.
THE OPPORTUNITY IN THE DENTAL SETTING
The dental setting provides a unique environment for the provision of care for a range of health issues. For some time, in many developed nations, people have tended to visit the dental practice more frequently than they visit the medical practitioner. They have been more likely to seek medical advice when they are experiencing discomfort or have recognized symptoms that require assistance. The concept of the regular, 6 - month “dental check - up” has enjoyed strong recognition and relevance with many members of the public. In more recent times, health practitioners and public health care initiatives have embraced the concept of regular visits as part of a monitoring/preventive approach rather than a response to an acute episode. This frequency of visitation has allowed collaborative patient care plans to develop with interprofessional exchange. For example, many optometrists regularly screen for signs of diabetic retinopathy as a possible indicator of undiagnosed diabetes or as a consequence of managed diabetes. Within the context of the dental setting, a patient may be a part of the practice for many years and, in some cases, a lifetime. Additionally, the practice may also provide care for the patient’s family members and their friends, who all form part of the individual’ s environment and lifestyle. This unique situation allows the oral health professional to acknowledge and gain a broad understanding of the myriad of influential health care factors associated with patient care. The dental setting, therefore, provides a privileged situation in which the dental professional can realize the opportunity to form a long-standing and supportive relationship in health care management with his or her patient. However, this opportunity is often underutilized or ignored completely when the clinician assumes a more conventional role.
Historically, dental clinicians have been characterized as “active,” “powerful,” and “expert,” while patients have been described as “passive” and “cooperative.” The dental treatment room itself, where the patients are in a submissive position and the clinicians are in a controlling position, supports these traditional roles. With a focus on technical expertise, dental clinicians may believe that their communications with patients will be based on common sense or are secondary to the provision of successful treatment. As shown in Figure 1.1, this traditional view of dental care is generally understood as operative oral medicine, or even dental surgery alone. Even though a patient suffering from oral pain will be correctly diagnosed with a hopeless tooth by the clinician, and subsequently treated with a tooth extraction, the patient may not be approached any further with the measures necessary for the prevention of further tooth loss.
Even if the need for preventive measures is recognized, some dental clinicians struggle with interviewing skills, may miscalculate how much (and how) information should be shared, have difficulty detecting and resolving issues with patient cooperation, or have varying levels of skill in interpreting nonverbal behaviors. Quite possibly due to a familiarity with diagnosing a problem, followed by providing a solution, preventive approaches are delivered in a prescriptive format. This may result in a situation that is illustrated in Figure 1.2: tobacco use is identified in the health history form of a patient who will be approached with the advice to quit. However, since there are no further measures taken, doubt remains whether beneficial health behavior change, such as smoking cessation, will occur.
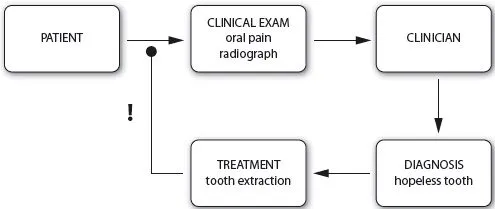
Figure 1.1. Operative oral medicine.
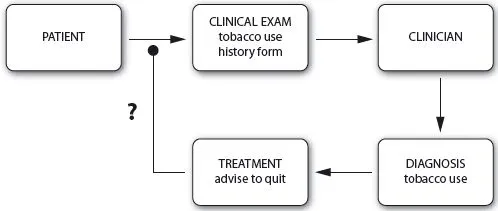
Figure 1.2. Preventive oral medicine.
Consequently, current advice giving or health education approaches appear to be unpredictable in accomplishing long-term change, potentially leading to frustration of both the patient and the clinician. Yet, the patient may be blamed for poor compliance and further oral health education may be judged as pointless.
Adoption and i ntegration of health behavior change
History has demonstrated that the past efforts of health professionals to promote changes in behavior that support positive health outcomes have potential for improvement. Compliance with medical recommendations is generally poor across all chronic disease regimens, which increases health care expenditures and prevents patients from achieving the full benefit of health behavior interventions. A number of studies have been conducted investigating ways to improve compliance, but research results have not shown to affect significant changes in compliance behavior (Berg et al. 2006).
This dilemma of patient and clinician agreement regarding long-term changes in health behavior has been systematically examined for over 50 years. In 2001, the World Health Organization (WHO) convened a conference to focus on the issues associated with outcomes commonly termed as treatment adherence and compliance. Poor adherence to treatment of chronic diseases was reported at a rate of 50% in developed countries with even lower rates of adherence in developing countries (WHO 2003). This review not only demonstrates the challenges associated with health behavior change but also provides a catalyst for health practitioners to review their role as a significant factor in the success of compliance strategies.
Health care providers may harbor an unwarranted sense of their own importance in inspiring behavior change, ignoring other variables that impact a patient’ s behavior. This may serve to diminish the patients’ key role rather than empowering the patients themselves. Although health care professionals typically believe that they are providing quality care, it is generally from their own perspective that they are defining quality (Larsen et al. 2006). The patient perspective of quality could be very different, as there may be a fundamental disagreement of needs and expectations in the clinician-patient relationship. Even if there is agreement, the acceptance of care or behavior change (adoption) and the practical application (integration) of care or behavior change often requires further exploration to ensure ongoing success.
Many oral health professionals underestimate the importance of communication as compared to technical skill. This tends to foster a focus on compliance rather than collaboration. Additionally, the framework of dental care delivery reinforces a traditional model of clinician-patient roles that diminishes the value of the communication necessary for successful partnership (Gochman 1997). Despite the possible negativity associated with past approaches, oral health professionals should be e...
Table of contents
- Cover
- Table of Contents
- FOREWORD
- PREFACE
- CHAPTER 1: INTRODUCTION TO HEALTH BEHAVIOR CHANGE FOR THE DENTAL PRACTICE
- CHAPTER 2: THE CHALLENGE OF BEHAVIOR CHANGE
- CHAPTER 3: COMMUNICATION AND HEALTH BEHAVIOR CHANGE COUNSELLING
- CHAPTER 4: MOTIVATIONAL INTERVIEWING (MI) AND ITS BASIC TOOLS
- CHAPTER 5: BRIEF INTERVENTIONS IN PROMOTING HEALTH BEHAVIOR CHANGE
- CHAPTER 6: IMPLEMENTATION OF HEALTH BEHAVIOR CHANGE PRINCIPLES IN DENTAL PRACTICE
- CHAPTER 7: HEALTH BEHAVIOR CHANGE EDUCATION
- INDEX
- End User License Agreement