This is a test
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
ABC of Palliative Care
Book details
Book preview
Table of contents
Citations
About This Book
This brand new edition pulls together the most up-to-date information on this complex, multidisciplinary area in a practical, user-friendly manner. It deals with the important social and psychological aspects for palliative care of people with incurable diseases including quality of life, communication and bereavement issues.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access ABC of Palliative Care by Marie Fallon, Geoffrey Hanks, Marie Fallon, Geoffrey Hanks in PDF and/or ePUB format, as well as other popular books in Medicine & Nursing. We have over one million books available in our catalogue for you to explore.
1
The principles of palliative care
Components of palliative care
Palliative care is recognised by individualised, holistic models of care, delivered carefully, sensitively, ethically, and therapeutically by using skilled communication with attention to detail, meticulous assessment, and advancing knowledge.
Wherever palliative care is used, its core ingredient is the quality of presence that the caregiver brings to the patient, a way of caring that enables discernment of the ongoing needs of the patient and family as they evolve and emphasises being alongside them. The focus is on all that is still possible in this time of multiple losses, the patient’s and family’s quest for meaning, and sustaining their experience of connectedness as they adapt to the challenges of the moment.
The term “palliative care” implies a personalised form of health care. It extends the healthcare professional’s mandate beyond the biomedical model to the wider horizon necessary if one is to attend to suffering as well as the biology of disease, caring as well as curing, quality of life as well as quantity of life. The patient and family or significant others are taken together as the unit of care in assessment of needs related to illness. The aim of palliative care is to support optimal quality of life and to foster healing—that is, a shift in response towards an experience of integrity and wholeness on the continuum of the quality of life.
Beyond the physical
Meticulous attention to the alleviation of symptoms is the foundation of care of the whole person. Important psychosocial and spiritual concerns may be eclipsed by the presence of uncontrolled pain, nausea, constipation, and the other symptoms of advanced disease. Optimal treatment demands careful assessment of the multiple contributory factors to each symptom. If increasing doses of opioid are prescribed in response to pain that is escalating due to unrecognised existential anguish, the result will be persistent pain, opioid toxicity, and ongoing distress for the patient, family, and caregivers. If we are body, mind, and spirit, those domains are inseparable and interdependent. Thoughtful assessment of each complaint should be considered in the context of the patient’s total suffering; therefore thoughtful assessment is mandatory.
Not just symptom control
Control of symptoms in palliative care commonly involves the concurrent use of six to eight or more medications. The goal is consistently to prevent rather than treat symptoms. Effective management depends on frequent adjustment to consistently sustain the minimal effective doses of medication and an emphasis on skilled nursing care as well as the use of the complementary skills of an interdisciplinary team experienced in end of life care.
Laboratory investigations—and even such non-invasive routines as monitoring blood pressure, pulse, and temperature—are undertaken only if doing so may lead to interventions that will enhance the quality of life.
Palliative care is founded on a philosophy that promotes sensitivity to cultural, religious, sexual, and other defining perspectives from the patient’s point of view; the intent to meet patients where they are rather than where the caregivers feel they should be; sensitivity to the determinants of coping, particularly concerning major existential challenges for the patient, family, and caregivers (death; isolation; freedom—the absence of external structure; meaning); attention to the meaning of the illness for the patient, family, and caregivers; and attention to the need for relating to people in an empathic way.
Palliative care is the approach that improves the quality of life of patients and their families facing the problems associated with life threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual (World Health Organization, 2005)
The quality of life continuum

Palliative care: selected philosophical perspectives and assumptions
- Nothing matters more than the bowels (Cecily Saunders)
- Humanise, personalise, de-institutionalise
- Clinical care grounded in qualitative and quantitative inquiry
- Experience of illness viewed as a narrative: relational, meaningful, filled with potential
- Assist progressive understanding of reality at a rate acceptable to the patient
- “Reality” as illusion; subjectivity of experience; acknowledgment of mystery
- Quiet efficiency, not hustle and bustle
- Focus on quality of living in the present moment, not death
- Accompaniment: empathic presence to the other in the moment
- Team: led by the patient; egalitarian rather than hierarchical
- Environment: centred on the patient, welcoming, peaceful
- Uniqueness, limitations, defences of the patient/family
- Healing of psyche: an innate potential
- Potential for adaptation, integration, reconciliation, transcendence
- Importance of compassion, celebration, community, paradox, humour
- With unresolved symptoms, “Review! Review! Review!” (Robert Twycross)
Application
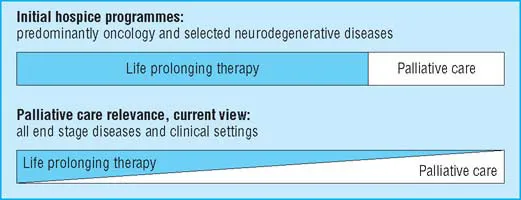
The early successes of hospice care in alleviating the suffering of patients with cancer and those with motor neurone disease and some other neurodegenerative diseases at the end of life has led now to broad agreement concerning the relevance of palliative care across the spectrum of disease and healthcare settings.
Care delivery
Considerations in the provision of palliative care include a seamless continuity of care appropriate to the needs of the patient and the family, with options that include home care; chronic inpatient care; acute, specialised inpatient (tertiary) care; consultation services available for those still receiving treatment to modify the disease; day care with resources for multidisciplinary assessment; bereavement support for those at risk of a complicated grief reaction.
Specialist role
General palliative care is practiced widely in specialties other than palliative care. Multiprofessional teams who work full time in palliative care, and are trained beyond the basic level, deliver specialist palliative care. They aim to care for those patients and carers who have complex physical, psychosocial, or spiritual needs that are difficult to manage. Their role is primarily about advice, support, and education when they work alongside other specialties. Hospices and hospice wards have more direct management of patients and carers in an inpatient setting. Role modelling, service development in line with local, national, and WHO guidelines, education, and research are further components of the role.
Multidisciplinary teams
Caring for patients and carers at a difficult time is synonymous with palliative care. Each patient and carer will require a unique and individualised approach to incorporate all their biopsychosocial and spiritual needs. There cannot be a universal optimum model for the delivery of care; adaptability and flexibility is paramount, and this is an increasing challenge in today’s healthcare systems.
A single profession, like a single model of care, can only fail to meet the holistic fluctuating needs of patients and carers. The knowledge and skill of many professions—medical, nursing, pharmacy, social work, physiotherapy, occupational therapy, and chaplaincy—held together by endless communication and teamwork is vital.
Future challenges
New and evolving challenges in palliative care are emerging as patients live longer with improved palliative tumoricidal treatments. Symptoms that are difficult to control and are chronically debilitating test the resilience and resources of weary patients, carers, and providers of health care. Education and robust multiprofessional support are necessary to equip those working in palliative care with the sustainable resilience demanded by an unwavering quality of presence that continues to effectively focus on quality of life and care and attend to suffering of patients with longer and more difficult experiences.
Changes in allocation of resources with the development of palliative care
Palliative care
- Affirms life and regards dying as a normal practice
- Neither hastens nor postpones death
- Provides relief from pain and other distressing symptoms
- Integrates the psychological and spiritual aspects of care
- Offers a support system to help patients live as actively as possible until death
- Offers a support system to help the families of patients cope during the patient’s illnesses and in their own bereavement
Essential components of palliative care
- Control of symptoms
- Effective communication
- Rehabilitation
- Continuity of care
- Terminal care
- Support in bereavement
- Education
- Research
Dame Cecily Saunders, founder of St Christopher’s Hospice (reproduced with permission)

Without research, advances in the science of control of symptoms and quality of care will stagnate and palliative care will cease to meet the future needs of patients with advanced life threatening illnesses and their carers. Though there are numerous epidemiological surveys outlining problems, few researchers do good quality interventional studies or try to extend knowledge through collaboration with basic science. More collaborative research involving basic science and other appropriate specialties is needed urgently.
The late Dame Cecily Saunders and her vision of combining optimum care, observation, and appropriate research established the essential ingredients of modern palliative care; this should remain our basis for the future.
Further reading
• Cassell EJ. The nature of suffering and the goals of medicine. 2nd ed. New York: Oxford University Press, 2004.
• Doyle D, Hanks GW, Cherny N, Calman K, eds. The Oxford textbook of palliative medicine. 3rd ed. Oxford: Oxford University Press, 2004.
• Halpern J. From detached concern to empathy: humanizing medical practice. New York: Oxford University Press, 2001.
• Kearney M. A place of healing: working with suffering in living and dying. Oxford: Oxford University Press, 2000.
• Saunders C, Sykes N. The management of terminal disease. 3rd ed. London: Edward Arnold, 1993.
• Yalom ID. Existential psychotherapy. New York: Basic Books, 1980.
2
The principles of control of cancer pain
Pain is a complex phenomenon which is the subjective endpoint of a variety of physical and non-physical factors. For most patients, physical pain is only one of several symptoms of cancer. Relief of pain should therefore be seen as part of a comprehensive pattern of care encompassing the physical, psychological, social, and spiritual aspects of suffering. Physical aspects of pain cannot be treated in isolation from other aspects, nor can patients’ anxieties be effectively addressed when patients are suffering physically. The various components must be addressed simultaneously.
Our understanding of the basic mechanisms of pain has improved considerably over the past few years. This understanding has included a greater appreciation of the relationship between the physical injury, pain pathways, and our emotional processing of this information; these factors are interlinked in the nervous system, rather than working in parallel. We now understand from basic science more of the mechanisms of total pain than ever before. It is clear that anxiety, fear, and sleeplessness feed into the limbic system and cortex. In turn, the brain talks back to the spinal cord modifying pain input at spinal levels. This then feeds back to the brain and a loop is established.
Mood disturbance is common in patients with uncontrolled cancer pain and may need specific management, however, sometimes it will improve dramatically with effective resolution of pain. Hence the first principle of managing cancer pain is an adequate and full assessment of the cause of the pain, bearing in mind that most patients have more than one pain. With effective assessment and a systematic approach to the choice of analgesics using the WHO’s three step analgesic ladder, over 80% of cancer pain can be controlled with the use of inexpensive drugs that can be self administered by mouth at regular intervals.
The WHO analgesic ladder
The analgesic ladder remains the mainstay of our approach to analgesia, though this was never designed for use in isolation. Surgery, radiotherapy, and appropriate tumoricidal treatments will have an important role in some patients, as will non-drug treatments. A combined approach can lead to optimum analgesia with minimum side effects.
Analgesic drugs do, however, remain key in managing cancer pain. The choice of drug should be based on the severity of the pain, not the stage of disease. Drugs should be administered in standard doses at regular intervals in a stepwise fashion. If a non-opioid or, in turn, an opioid for moderate pain is not sufficient, an opioid for severe pain should be used.
When a non-opioid drug is used with an opioid for moderate pain, many patients find combination formulations more convenient to use. Care must be taken with the dose of each drug in the formulation; some combinations of codeine or dihydrocodeine with aspirin or paracetamol (including co-codamol and co-dydramol) contain subtherapeutic doses of the opioid. The decision to use an opioid for severe pain should be based on severity of pain and not on prognosis.
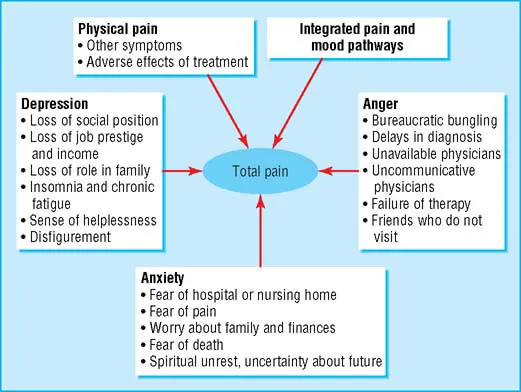
Factors affecting patient’s perceptions of pain (adapted from Twycross RG, Lack SA, Therapeutics in terminal disease, London: Pitman, 1984)
Analgesic drugs commonly recommended for cancer pain
Mild pain
- Aspirin 600 mg four times a day
- Paracetamol 1 g four times a day
Moderate pain
- Codeine 60 mg (plus non-opioid drug) four times a day
Severe pain
- Morphine 5–10 mg (starting dose) every four hours
Non-drug treatments used in management of cancer pain
- TENS (transcutaneous electrical nerve stimulation)
- Physiotherapy
- Acupuncture
- Relaxation therapy
WHO analgesic ladder (adapted from WHO’s Cancer pain relief and palliative care technical report ...
Table of contents
- Cover
- Contents
- Series Page
- Title Page
- Copyright
- Contributors
- Foreword
- 1 The principles of palliative care
- 2 The principles of control of cancer pain
- 3 Difficult pain
- 4 Breathlessness, cough, and other respiratory problems
- 5 Oral health in patients with advanced disease
- 6 Anorexia, cachexia, nutrition, and fatigue
- 7 Nausea and vomiting
- 8 Constipation, diarrhoea, and intestinal obstruction
- 9 Depression, anxiety, and confusion
- 10 Emergencies
- 11 The last 48 hours
- 12 Palliative care for children
- 13 Communication
- 14 The carers
- 15 Chronic non-malignant disease
- 16 Community palliative care
- 17 Bereavement
- 18 Complementary therapies
- Index