- English
- ePUB (mobile friendly)
- Available on iOS & Android
Emergency Medicine
About this book
Emergency Medicine Lecture Notes provides all the necessary information, within one short volume, for a sound introduction to this core specialty area.
Presented in a user-friendly format, combining readability with flowcharts and high-quality illustrations, this fourth edition has been thoroughly revised to reflect recent advances in the field of emergency medicine. For this new edition, Emergency Medicine Lecture Notes features:
• Illustrations and flow charts in a two colour presentation throughout
• More detail on imaging, diagnosis and management of a wide range of acute conditions
• A brand new companion website at www.lecturenoteseries.com/emergencymed featuring a selection of MCQs to test readers on common pitfalls in emergency medicine
Not only is this book a great starting point to support initial teaching on the topic, but it is easy to dip in and out of for reference or revision at the end of a module, rotation or final exams. Whether you need to develop or refresh your knowledge of emergency medicine, Emergency Medicine Lecture Notes presents 'need to know' information for all those involved in treating those in an emergency setting.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
WHAT TO DO IN AN EMERGENCY
A – Airway
- patent, partially obstructed or completely obstructed (this results from physical obstruction or loss of muscle tone)
- adequately protected or at risk (this depends on the protective reflexes of the airway).
Check for Responsiveness
- a maintained and protected airway
- temporarily adequate breathing and circulation
- cerebral functioning.
Look, Listen and Feel for Breathing
Look for the Signs of Partial Upper Airway Obstruction
- Snoring: the familiar sound of obstruction caused by the soft tissues of the mouth and pharynx. Often it accompanies the reduced muscle tone of a lowered level of consciousness.
- Rattling or gurgling: the sound of fluids in the upper airway.
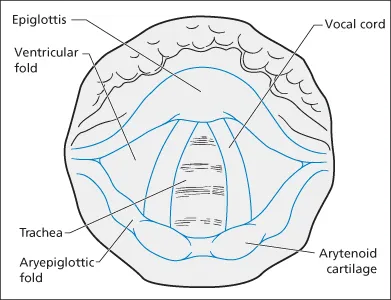
- Stridor: a harsh, ‘crowing’ noise, which is heard best in inspiration. It is thus different from wheezing, which is usually loudest in expiration. Stridor suggests obstruction at the level of the larynx and upper trachea. General illness and temperature usually indicate an infection causing swelling. Obstruction by a foreign body is the other main cause.
- Drooling: the inability to swallow saliva. It suggests blockage at the back of the throat.
- Hoarseness: gross voice change. This suggests obstruction at the level of the larynx.
Clearance and Maintenance of the Airway
- tightening these tissues (chin-lift manoeuvre)
- pushing the jaw and the hyoid bone and their attached soft tissues forward (jaw-thrust manoeuvre)
- putting an artificial airway down the anatomical airway (oro- or nasopharyngeal airways, endotracheal tubes, laryngeal masks, etc. → Figure 1.1).
- removing the cause of the obstruction (suction, manual removal or choking manoeuvres)
- passing an artificial airway (as detailed above) past the obstruction
- reducing the swelling with vasoconstrictor drugs (adrenaline)
- bypassing the obstruction with a surgical airway.
Protection of the Airway
- The recovery position uses gravity, both to drain fluid matter away from the airway and to allow the soft tissues to be positioned in such a way that they do not cause obstruction. Once the airway is clear, this position can be used to both maintain and protect the airway.
- A high-flow suction catheter must always be near the patient’s head.
- The patient’s trolley must be capable of tilting ‘head down’ so as to drain vomitus out of the airway.
- If endotracheal intubation is attempted, the airway must be protected by the manoeuvre known as cricoid pressure throughout the period of instrumentation. Pressure is applied to the front of the patient’s cricoid cartilage by an assistant using the thumb and two fingers. This compresses the oesophagus against the cervical spine and thus prevents the passive regurgitation of gastric contents. The airway is vulnerable from the start of induced paralysis until the cuff is i...
Table of contents
- Cover
- Dedication
- Title page
- Copyright page
- Preface to the fourth edition
- Preface to the second edition
- Preface to the first edition
- 1 What every emergency physician must know
- 2 Major trauma and multiple injuries
- 3 Head injuries
- 4 The neck and the back
- 5 Facial injuries
- 6 Injuries to the trunk
- 7 The lower limb
- 8 The upper limb
- 9 The hand
- 10 Burns, contamination and irradiation
- 11 Cardiac arrest and cardiac dysrhythmias
- 12 Chest pain
- 13 Respiratory distress
- 14 Collapse and sudden illness
- 15 Poisoning
- 16 Abdominal pain
- 17 Obstetric, gynaecological, genitourinary and perineal problems
- 18 Children’s problems in the emergency department
- 19 The disturbed patient
- 20 Medicolegal aspects of emergency medicine
- 21 Small wounds and localised infections
- 22 Ophthalmic, ENT and facial conditions
- Index
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app