![]()
Chapter 1
Setting the scene
Caroline Watkins and Michael Leathley
Key points
- Transforming stroke services is of paramount importance in the quest to save lives and reduce dependency.
- Translating research evidence into clinical practice is challenging but many examples show that this is both achievable and worthwhile.
- Continued development of stroke nursing through expansion of the stroke nursing knowledge base and demonstration of competence and skill is pivotal to the future of the specialism.
- Continued development of stroke nursing is essential for development of stroke services, locally, nationally and internationally.
Introduction
In the UK and internationally, stroke and its impact on people’s lives is finally gaining the recognition it deserves both as an acute event and as chronic disease. The profile of stroke has been raised partly by the burden it places on an individual, their family, the health service and society but more recently because effective treatments have become available. However, to make these treatments available for everyone who might benefit, it is imperative that the public know about and have a heightened awareness of stroke symptoms. Public awareness campaigns are graphically driving home the message that if a stroke is suspected, contact the emergency medical services. Emergency services must respond rapidly and get patients to centres providing specialist acute-stage treatments, ongoing rehabilitation and long-term support. Throughout this care pathway, best-available treatment can only be provided if staff have stroke-specific knowledge and skills commensurate with their roles, and if all agencies involved work collaboratively, providing a seamless journey for the person affected by stroke. Nurses are the largest section of the workforce, and involved throughout the entire pathway. Consequently, nurses have the greatest opportunity to play a key role in providing leadership and delivery of evidence-based stroke services.
This chapter sets stroke nursing in the context of wider systems. Starting by identifying the extent of the problem of stroke, it illustrates why stroke has become a burning issue for health care and research. It discusses policy imperatives and the present and future stroke-specific infrastructure; it identifies the need to support stroke service developments, to put in place mechanisms to produce evidence for practice, as well as clarifying how evidence can be implemented into practice. Fundamental to delivery of this huge agenda is the development of a stroke-specialist workforce, such that those staff delivering care along the stroke pathway not only have the right knowledge, skills and experience in stroke, but achieve recognition for it. Suitable recognition for the specialism should ensure that the most able staff pursue careers in stroke care. This then should establish a virtuous circle, whereby able staff stay in the specialty and contribute further, delivering sustainable quality improvements into the future.
Stroke epidemiology
Stroke is a major cause of mortality and morbidity in adults. It is the third leading cause of death, and a major cause of adult neurological disability. In the UK, the incidence per annum of stroke is approximately 130000 people, with a further 20000 people per annum experiencing transient ischaemic attack (TIA) (National Audit Office 2005). In the UK, the incidence of first-ever stroke is approximately 200 per 100000 people per year (Sudlow & Warlow 1997), similar to other Western countries, including Australia. The case fatality of first-ever stroke has been reported as approximately 12% at 7 days, 20% at 30 days, 30% at 1 year, 60% at 5 years and 80% at 10 years (Dennis et al. 1993; Hankey et al. 2000; Hardie et al. 2003). There is a 10% risk of recurrent stroke within 7 days, 18% within the first 3 months (Coull et al. 2004; Hankey 2005; Hill et al. 2004).
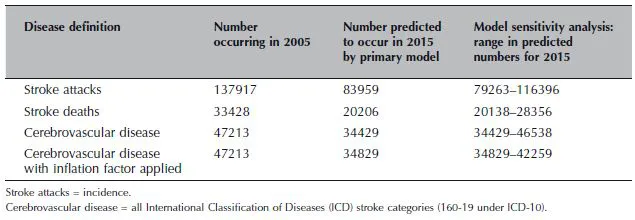
Earlier estimates suggested that in the UK between 1983 and 2023 there would be a 30% increase in numbers of people experiencing a first-ever stroke, increasing the demand on stroke services. More recently, it has been suggested that the incidence of stroke is falling, but with increasing numbers of older people in the population, the overall burden of stroke is nonetheless likely to increase due to a rise in prevalence (Rothwell et al. 2005). Lifestyle issues, for example obesity and binge drinking, may also result in an increased risk of stroke (Reynolds et al. 2003; Zaninotto et al. 2006) and have become the focus of important public health messages. Currently, trends are unclear and further research is needed to understand what the future holds. Recent work, which is shown in Table 1.1, indicates trends of stroke incidence may not increase, and may even decrease (Dey et al. 2007). However, it is clear that more people are surviving stroke and living with the sequelae, which can have profound effects in all domains of life (Jagger et al. 2007). Whilst we want acute stroke interventions to improve survival rates, we also want them to ensure independent survival.
Table 1.1 Summary table of predictions. Reproduced with permission from Dey, P, Sutton, C, Marsden, J, Leathley, M, Burton, C, & Atkins, C, 2007, Medium Term Stroke Projections for England 2006 to 2015, Department of Health.
Stroke policy
Developing stroke as a health care priority
Over the past decade stroke has received increasing attention from professional health care providers and the UK government. A similar situation has been seen in Australia (see Preface, Australian perspective). When the first National Sentinel Audit (NSA) was performed in 1998, it highlighted the poverty of stroke services. One of the biggest problems was the lack of stroke units and how few people were admitted to a stroke unit at some point during their hospital stay. This was particularly discouraging because the benefits of organised inpatient care had been known for over a decade (Indredavik et al. 1991; Langhorne et al. 1993). Not long after this first audit the first edition of the National Clinical Guidelines for Stroke (Intercollegiate Stroke Working Party 2000) was developed. From the start, guideline developers agreed that patients’ views would be an important factor in determining how services should be run. Focus groups were used to elicit the experiences of those affected by stroke, their preferences and recommendations for service provision (Kelson et al. 1998). The guidelines give health care providers best practice recommendations, underpinned by evidence from research or expert consensus, and incorporate the views of those affected by stroke. Both the NSA and the clinical guidelines have been important levers in the improvement of stroke care, demonstrating the influence that stroke metrics (data collection points) and clinician-led practice standards can achieve. The success of this model has led to its replication in Australia and other countries.
Key components of stroke care are assessment, management and treatment, and evidence to underpin these have been used to produce and update UK National Clinical Guidelines for Stroke (Intercollegiate Stroke Working Party 2000, 2004a, 2008a). Concurrently, successive rounds of the National Sentinel Audit (Intercollegiate Stroke Working Party 2002, 2004b, 2007, 2008b) have revealed the relationship – and shortfalls – between evidence and practice. Overall, the judgement has been that response to suspected stroke has not been fast enough, either in terms of actions taken for an individual experiencing a stroke or in implementing into practice what scientific literature indicates should be done (National Audit Office 2005). That is, scientific advances are not consistently or rapidly translated into clinical practice. It is precisely this which has led to current benchmarking of stroke services.
In 2001, the UK National Service Framework (NSF) for Older People was published (Department of Health 2001). The NSF set standards to provide person-centred care, remove age discrimination, and promote older people’s health and independence. Standard Five in this document focused on stroke and set milestones (dates) for the provision of aspects of care, for example, that those affected by stroke would have access to a stroke unit. The NSA demonstrates these milestones still have not been fully met. Furthermore, it has taken time to ensure that all important milestones are recognised. For example, the second edition of the National Clinical Guidelines for Stroke, published in 2004, updated the evidence from the first edition, but still missed an important element of the stroke pathway – that between symptom onset and arrival at hospital. An addendum around early recognition and management of suspected stroke and TIA addressed this shortcoming (Jones et al. 2007).
A National Audit Office report in 2005 outlined advances in stroke care and made recommendations about future improvement (National Audit Office 2005). The following year, Professor Roger Boyle, National Director for Heart Disease and Stroke, published the Mending Hearts and Brains document. His aim was to encourage continued development and change in the way we think and act about stroke and heart disease. The document acknowledged the hard work and enthusiasm of NHS staff and set a challenge to improve services: ‘we have to set the bar a lot higher in defining the level of service the public should be able to expect’(Department of Health 2006). This was followed by a consultation process with health care providers and service users, resulting in the National Stroke Strategy in 2007 (Department of Health 2007) – see below. The next round of updated guidelines saw initial management of acute stroke and TIA published by the National Institute for Health and Clinical Excellence (NICE) linked with the third edition of the National Clinical Guidelines for Stroke (Intercollegiate Stroke Working Party 2008a).
Between 2004 and 2005 the UK Stroke Association developed the ‘FAST campaign’, designed to raise public awareness of stroke through use of the ‘Face, Arm, Speech, Test’(Harbison et al. 2003). Their campaign was revised in 2009, with the ‘T’ in FAST now standing for time rather than test, which emphasises the importance of rapid response. The campaign ran alongside a Department of Health public awareness campaign, also using FAST, through television and radio advertising. The potential value of such campaigns is great. Stroke has been calculated to cost the NHS £2.8 billion in direct costs; additionally £1.8 billion accrued due to lost productivity and disability, plus £2.4 billion in informal care costs (National Audit Office 2005). The National Audit Office report stated that response to stroke was not as fast and effective as it could be and that, with more efficient practice, there was scope for potential savings of £20 million annually, with 550 deaths avoided and over 1700 people recovering from their stroke each year who would not otherwise have done so (National Audit Office 2005).
UK stroke policy development
Throughout the world, countries are developing documents and guidelines to mandate the provision of quality stroke care. In England, for example, the National Stroke Strategy (NSS) was launched in 2007 (Department of Health 2007). The NSS is underpinned by substantial research evidence and expert consensus, and endeavours to clarify the components of guideline-concordant care, whilst acknowledging the current lack of comprehensive, integrated stroke care systems to deliver this. To assist in implementing NSS recommendations, an additional £105 million was identified for stroke care in the 2007 Public Spending Review. A commissioning framework was developed (Department of Health 2006) with guidance to Commissioners on key issues and resources to inform decision-making.
Nevertheless ensuring that ‘the system provides patients with the precise interventions they need, delivered properly, precisely when they need them’(Woolf & Johnson 2005, p. 545) is challenging. Whilst the NSS can tell us what we need to do, we must determine how this can be delivered in local health care systems. Where there is evidence for effectiveness of interventions, we need to understand the design of the studies, underlying suppositions, and the context (organisational, geographical, demographic, etc.) in which the intervention was tested. Often, studies report the effectiveness of interventions with only an outline of the intervention; methods of testing are detailed, but processes (barriers, facilitators, etc.) of introducing the intervention are rarely considered. Without detailed knowledge of how to implement research evidence into practice, implementation is hampered, and potential benefits to patients not fully realised. Consequently, despite having effective treatments for stroke and TIA, unless we understand the health care delivery models that can ensure timely access to treatment and ...