- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Haimovici's Vascular Surgery
About this book
To improve the diagnosis and management of patients with vascular disease turn to the most authoritative and trusted reference for 36 years and counting . . .
The role of the vascular surgeon has evolved. Vascular surgeons now perform minimally invasive vascular procedures and provide comprehensive care in addition to open surgery.
Haimovici's Vascular Surgery, now in its 6th edition, has been extensively updated to provide you with:
- Expert perspectives on how the vascular surgery field has evolved so you continue to stay on the leading edge of this dynamic field
- Concise and practical advice about what these changes and new areas of practice mean to you – the practitioner and trainee in the fields of vascular surgery, interventional cardiology and interventional radiology
- Fundamental principles and best practices to treat traditional and new modalities that are now part of the vascular surgeons purview
What's new in this edition?
- Full-color photographs and illustrations
- Complete coverage of the latest diagnostic imaging modalities, including intravascular ultrasound and computed tomography
- Expanded information on the most effective minimally invasive treatment options, including those for diseases of the carotid artery, lower extremity and abdominal aorta
- Full coverage of non-surgical techniques that vascular surgeons may add to their repertoire.
Time-saving feature exclusive to the 6th edition
To help you identify actionable information quickly, each chapter now highlights the most relevant clinical information. Apply what you learn to your own practice immediately.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
PART I
Vascular Imaging Techniques and Physiologic Testing
CHAPTER 1
Arterial and Venous Duplex Scanning
The noninvasive vascular laboratory provides the scientific basis for vascular surgery. It safely provides accurate and quantitative evidence of the presence and physiologic significance of arterial and venous disease. In the modern vascular laboratory ultrasound-based techniques, particularly duplex ultrasound techniques, are most extensively employed.
Ultrasound Basics
Duplex ultrasound was introduced in 1974 with application to the carotid artery. “Duplex” indicates the technique combines B-mode imaging and Doppler analysis of blood-flow direction and velocity. It is extensively utilized for evaluation of carotid arteries, intra-abdominal arteries and veins, and upper- and lower-extremity arteries and veins. Since its inception, engineering and software advances have been extensive and include: 1) improved gray-scale B-mode imaging, 2) low-frequency scan heads permitting deep penetration of the ultrasound beam from the skin surface, 3) improvements in online computer-based microprocessing, and 4) addition of color-flow imaging.
Color flow is a superimposed real-time colorized image of blood flow onto a standard gray-scale B-mode picture. Echoes from stationary tissues generate B-mode images, whereas those interacting with moving substances (blood) generate a phase shift that is processed separately and color coded to give information on the direction and velocity of blood flow that reflects the magnitude and direction of the Doppler shift. Color flow dramatically reduces the time required to perform duplex examinations by allowing more rapid identification of vessels to be examined. It appears essential for duplex examination of some vessels, such as tibial arteries and veins. Color flow and the ability of modern duplex scanners to detect blood flow velocities <5 cm/s make duplex scanning practical in virtually all areas of the body.
Basics of Duplex Ultrasound
A vibrating source produces an ultrasonic wave. In duplex ultrasound the vibrating source is the transducer. Ultrasound transducers are contained within scan heads. Scan heads steer and focus the sound beam produced by the transducer. The ultrasound image is derived from the returning echoes and is dependent on precise steering and focusing of the sound beam.
Transducers convert electrical into vibrational energy to produce the ultrasound wave. Transducers can also convert vibrational energy of returning echoes into electrical signals for analysis by the duplex machine’s software. The frequency of the vibration is determined by the design of the transducer and determines the wavelength of the sound wave. Frequency and wavelength are related, λ = c/f, where λ is the wavelength, c is the speed of sound in tissue, and f is the frequency.
Speed of sound in soft tissues averages 1540 m/s. There is little variation in the soft tissues insonated in clinical use of duplex ultrasound. Wavelength is the principle determinant of how well an ultrasound beam penetrates tissue, and wavelength depends on the frequency of the transducer. The transducer frequency is determined by the design of the transducer and is thus controlled by the manufacturer. For examination of the carotid artery, transducer frequencies of 5 to 7.5 MHz provide optimal tissue penetration for clinical purposes.
As noted above, duplex refers to the combination of Doppler and B-mode (“B” stands for “brightness”) ultrasound in the same device. Both require analysis of reflected echoes of the original sound beam created by the ultrasound transducer. B-mode analyzes the strength (intensity) and origin of the reflected echo. Doppler analyzes shifts in frequency of the original sound wave produced by the transducer.
B-Mode Ultrasound
As a sound wave passes through tissue and moves away from the transducer its strength depends upon how much the beam is scattered, attenuated, and reflected. Strength of reflected echoes depend, in part, upon differences in acoustic impedance between media. When there are major differences in acoustic impedance a large proportion of the sound beam is reflected back to the transducer. Small differences in acoustic impedances result in little reflection and the beam continues to propagate through the tissue.
In B-mode ultrasound, the brightness of the individual pixels comprising the ultrasound image is proportional to the strength of the returning echo. This is the ultrasound gray scale, and the resulting image is termed a gray-scale image. Very bright pixels in the gray-scale image indicate large differences in acoustic impedance between media. Less dramatic differences are represented by proportionally less-bright pixels. Thus gallstones, with dramatic differences in acoustic properties from soft tissue, produce strong echoes and proportionally very bright pixels on the ultrasound image, whereas blood, which differs little from soft tissue in acoustic characteristics, often cannot be distinguished from soft tissue with B-mode imaging.
The strength of the reflected echo is also dependent upon the strength of the sound beam at the point where it is relected. Gray-scale images represent the absolute strength of the reflected echo arriving back at the transducer, not the percentage of the beam reflected. Therefore, if the sound beam is very weak at the point of reflection even areas of dramatic acoustic differences will not result in a bright pixel in the B-mode image.
The strength of the ultrasound beam at a specific point also depends on how much the beam has been attenuated passing through tissue. Attenuation depends upon both the tissue traversed and the frequency of the wave. Wave frequency depends upon the frequency of the transducer generating the wave (see discussion above and Equation 1). Higher-frequency sound waves are attenuated more rapidly than lower-frequency sound waves. Higher-frequency transducers therefore provide relatively weak echoes to be reflected from a deep structure. The image generated is comparatively poor compared with a lower-frequency transducer insonating a deeper structure.
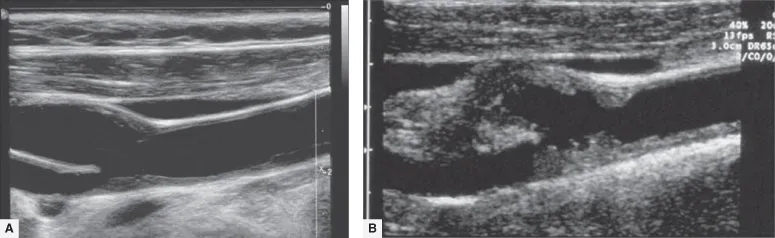
Image quality also depends upon linear resolution. Linear resolution is dependent upon the ability to focus the beam. High-frequency sound waves are better focused than sound waves from low-frequency transducers and provide sharper and better quality B-mode images. Image quality is therefore a balance of the strength of the reflected echo and the ability to focus the sound beam. The carotid artery is superficial and higher-frequency transducers can be used to provide clear B-mode images. (Fig. 1.1A and B) Image quality is less when examining deep vessels such as renal or iliac arteries.
Figure 1.1 Gray-scale images of (A) mildly and (B) severely diseased bifurcations of the cervical carotid artery.
Doppler Ultrasound
Continuous wave Dopplers have transducers that continually emit vibrations into tissue. Therefore, echoes are also continually reflected back to the transducer. Transducers cannot generate and receive echoes simultaneously. A continuous wave Doppler therefore must have separate transmitters and receivers to generate and receive echoes.
Duplex devices utilize pulse Doppler. Pulse Dopplers use a single transducer to generate and receive echoes. With a pulse Doppler it is possible to know when an echo is generated and when it is received. Because the speed of sound is relatively constant in tissue it is therefore possible to tell from what depth a reflected echo originated. The sample volume of the duplex machine is the site from which the returning echo originated. It is determined by specifying the depth from which the pulse Doppler receives reflected echoes.
The transducer of a pulse Doppler is gated, based on the total time from sound-wave generation to arrival of reflected echoes back at the transducer, to receive echoes only from a specified depth, the sample volume. The “position” of the sample volume is determined from the B-mode image. In vascular applications of duplex ultrasound this corresponds to points within the lumen of the vessel examined. B-mode images and Doppler waveforms cannot be generated simultaneously. The B-mode image therefore must be frequently updated during the course of a duplex-ultrasound examination to insure proper placement of the sample volume in the vessel.
When a sound wave encounters moving reflectors, the frequency of the reflected wave changes from that of the original wave generated by the transducer. In vascular ultrasound the moving reflectors are red blood cells. The frequency shift depends upon the velocity of the reflector and its angle with the incident sound beam. The frequency of the original sound wave is known. The frequency of the received echo can be determined by the software of the duplex machine. The velocity of the red blood cells can therefore be calculated provided the angle of the sound beam with the moving reflectors is also known. This relationship is the Doppler equation, fr − fo = [(2fov)/c] cosθ, where fr is the received frequency, fo is the originating frequency, v is the velocity of the reflector, c is the speed of sound in tissue, and θ is the angle of the incident sound beam with the moving reflectors. θ is termed the “Doppler angle.”
Obviously, solving the Doppler equation for the velocity of the moving reflectors requires knowing the Doppler angle. To standardize the results of duplex scanning it is recommended examinations be conducted with a Doppler angle of 60°. At this angle errors in velocity calculations secondary to misreading of the Doppler angle are small as a percentage of the true velocity. When the Doppler angle approaches 70° errors become of greater magnitude because the cosine of θ increases more than linearly. Small errors in determining the Doppler angle when the angle of insonation is <60° have little overall impact on the calculation of the velocity of the moving r...
Table of contents
- Cover
- Dedication
- Title page
- Copyright page
- Preface
- Preface to the Fifth Edition
- Contributors
- List of Abbreviations
- PART I: Vascular Imaging Techniques and Physiologic Testing
- PART II: Basic Science in Vascular Diseases
- PART III: Basic Open Vascular Techniques
- PART IV: Open Surgical Exposure of Arteries
- PART V: Cerebrovascular Insufficiency
- PART VI: Aortic and Iliac Aneurysms
- PART VII: Visceral Vessels
- PART VIII: Lower Extremity Occlusive and Non-Occlusive Arterial Disease
- PART IX: Vascular Trauma
- PART X: Upper Extremity Vascular Disease
- PART XI: Arterial-Venous Malformation, Access for Hemodialysis and Portal Hypertension
- PART XII: Venous and Lymphatic Disorders
- PART XIII: Amputations and Rehabilitation
- Index
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Haimovici's Vascular Surgery by Enrico Ascher in PDF and/or ePUB format, as well as other popular books in Médecine & Chirurgie et médecine chirurgicale. We have over one million books available in our catalogue for you to explore.