![]()
Part One
Issues and Methods of Public Health Practice
![]()
Chapter 1
The Need for Change in the Practice of Public Health
Learning Objectives
- Explain the primary mission of public health
- Define health
- Define primary prevention
- Describe population health
- Discuss the history of public health and its impact on current public health services
- Identify the characteristics of quality in the field of public health
Mission and Services of Public Health
Public health organizations, particularly government agencies, are pulled in many directions, and have had difficulty in both addressing the multiple determinants of health and providing population-centered services to improve community health outcomes. Determinants of health are the factors in the personal, social, economic, and environmental areas of life that affect the health status of individuals and populations.
The challenges facing modern-day societies require interventions and services that move beyond the traditional local public health offerings of personal health care, communicable disease control, and enforcement of environmental health laws. Public health organizations are now expected to understand and address the many factors affecting health produced by the environment, social relationships, communities, and institutions—while in the process forming multiple partnerships to improve health around the globe.
Mission of Public Health
The definition of mission of public health has undergone transformation over time. The earliest mission of public health involved the control of communicable diseases, such as cholera, smallpox, tuberculosis, and yellow fever, that inevitably led to epidemics. The most recent definition originated from the Institute of Medicine (IOM) in 2002 and is much broader. The IOM declared that the new mission of public health encompasses the organized efforts of society toward assuring conditions in which people can be healthy. Society has a dual interest in reducing communities' exposure to risk factors known to negatively affect health and in promoting healthy conditions that create and sustain health in the social and environmental spheres of everyday life.
Society's interest stems from the concept of health as a primary public good that promotes the many goals of a society, including the ability of humans to work, to enter into social relationships, and to participate in a political process. As a result of this broad interest, public health practitioners are expected to focus primarily on the health of community populations as opposed to expending their resources on the treatment of individuals for health problems that are usually addressed by physicians or hospitals providing medical services.
Population-Centered Health Services
A public health organization is expected to provide primary prevention services to a population. Primary prevention approaches to improving the health status of populations seek to inhibit the occurrence of disease and injuries by reducing exposure to risk factors that cause health problems. In other words, public health services intended to fulfill the mission of public health address the fundamental causes of disease and help foster or sustain conditions that contribute to health, with the goal of preventing undesirable health outcomes (Public Health Leadership Society, 2002). Public health's role also extends to health promotion and helping people gain control of their life and the determinants of health, creating healthier community populations.
What is a population-centered service? To answer this question, we must define the terms population and health. A population is a group of people with shared characteristics, such as location, race, ethnicity, occupation, or age. Community is a word that is often used interchangeably with the term population. Students in a school system, migrant and seasonal farmworkers, employees of the automobile industry, and county residents and visitors are all examples of populations or communities on which public health organizations may choose to focus and in which they might plan services designed to improve overall health outcomes, such as by reducing obesity or cancer rates.
A population-centered service organization seeks to improve health across multiple individuals over a period of time. Healthy People 2010 and 2020 are national initiatives to promote health and prevent disease by setting and monitoring national health objectives (Centers for Disease Control and Prevention [CDC], 1999a, 2009d). Proponents of these initiatives work collaboratively with partners to realize the goal of healthy people in healthy communities, a population-centered approach to improving the nation's health. Two examples of the proposed population-centered goals for Healthy People 2020 are increasing the quality and years of healthy life for individuals of all ages and eliminating health disparities among segments of the population that experience poorer health due to gender, race, ethnicity, education, income, disabilities, geographic location, or sexual orientation—the social determinants of health (U.S. Department of Health and Human Services [HHS], 2011). Population-centered health services designed to increase rates of physical activity across communities are examples of public health interventions that incorporate evidence, are population-centered, and promote health. The application of evidence-based practices increases the likelihood of achieving improved community health outcomes. Evidence-based public health practice is the use of the best available scientific evidence to make informed decisions about public health services (Brownson, Fielding, and Maylahn, 2009).
Defining and Modeling Health
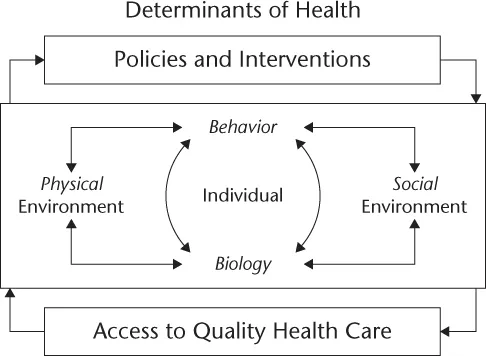
A current and popular definition of health was first presented by the World Health Organization (WHO) in its constitution in 1946, when health was defined as the state of complete physical, mental, and social well-being, and not just the absence of disease (WHO, 1947). This definition of health points to the intersecting domains of life (biological, social, political, cultural, and environmental) that work together in complex ways to produce the health of individuals who form populations. Models of health, such as the Healthy People 2010 determinants of health (see Figure 1.1), present the multiple parts of the system of health and help us understand the interrelationships among those parts. With models of health we can consider and address the various factors influencing the health of individuals and groups. Broadly understanding how communities maintain or promote health will assist us in adopting the public health interventions that are most likely to reduce or eliminate community populations' exposure to risks and improve their overall health status.
In the Healthy People model of the determinants of health, it is clear that health is contingent on more than individual biology or behavior. Current efforts to reform the health care system center on the issues of health care access, quality, and cost. However, physical and social environments are also important determinants of health, including the educational and income-earning potential of individuals. The policies implemented through legislation and the interventions to achieve policy goals that public health agency leaders and their staff select are also key in determining the health status of populations. Failure to enact the policies and interventions with the greatest likelihood of improving population health, evidence-based practices, can have dire consequences for communities if health outcomes decline as a result. A population-centered approach to health aims to improve health for all members of a population and reduce health disparities among segments of that group. Many experts and practitioners in public health are concerned about the lack of emphasis on population-centered policies and initiatives to promote health and reduce risks, such as laws that mandate the use of seat belts and control tobacco, and about the perpetuation of a system of personal health care services that are overly disease focused.
Intersectoral Public Health
The 2002 IOM definition of public health states that an organized effort is deemed essential for reducing risk and promoting healthy conditions in which people can experience improved quality of life. The absence of an organized societal effort to address identified risk factors that are connected to poor health is a barrier to progress on the front lines of improving the health of communities. Tobacco use, inadequate physical activity, poor diet, and excessive alcohol use cause many of the illnesses, disabilities, and early deaths attributed to chronic diseases. These are great challenges for a local public health system that is in disarray, and in which efforts to improve population health in a community or region show little signs of coordination across the various practitioners of public health. Relatively little coordination occurs across the various sectors working on public health to address the major health issues of our time—chronic and infectious diseases, tobacco use, poverty, environmental pollution, and man-made and natural disasters. Minimal integration of the delivery of personal health care, community health services, and environmental health services by a local public health agency reduces the effectiveness of that agency in preventing risk factors that contribute to common health problems, such as chronic illnesses. Recent assessments of the performance of some local public health systems revealed a number of serious deficiencies and indicated that little progress had been made over recent decades to provide the essential public health services (Brooks, R., Beitsch, L., Street P., Chukmaitov, A., 2009; Smith, T., Minyard, K., Parker, C. Valkenburg, R., and Shoemaker, J., 2007; FL DOH, 2005). Gaps continue to be found across local public health systems in the performance of the essential public health services, and the Centers for Disease Control and Prevention (CDC, 2008b) report that no state is completely prepared to respond to a major public health threat. A National Association of County and City Health Officer's (2010) profile study of over 80 percent of local public health agencies (LPHAs) in the USA revealed that from 2005 to 2008, immunizations were the most stable service category in LPHAs and population-based primary prevention services were the least stable service group.
The complex health problems on which public health systems are focused require interactions across the multiple sectors of society contributing to health outcomes. Public health experts and practitioners have worked together to identify the main sectors of society that have a role in promoting health—governmental public health, mass media, academia, business, communities, and health care institutions (IOM, 2002). Together these multiple players and disciplines form local public health systems, which have the potential to coordinate services and have a powerful impact on the challenging health problems in the world today.
Local public health agencies, also known as local health departments, are located in most counties or regions in the United States and are the primary government entities with the statutory responsibility for protecting and promoting populations' health. Local public health agency workers help form the backbone of a local public health system and are skilled in multiple disciplines, including epidemiology, surveillance, laboratory testing, health education, environmental health, and medicine. State public health offices or departments exist in every state in the nation. The national arm of public health is present in the Department of Health and Human Services, which houses the CDC, along with the Health Services Research Agency, the Office of the Assistant Secretary for Preparedness and Response, the U.S. Food and Drug Administration, and the National Institutes of Health.
As mentioned already, health care providers are important partners in promoting the public's health. For decades, the Internal Revenue Service has required nonprofit hospitals to report community benefit expenditures that improve community health status and reduce the burden for individuals of diseases and injuries that increase health care costs (Barnett, 2009). Community benefit was defined in a 1983 ruling by the Internal Revenue Service as the promotion of health for “a class of persons sufficiently large so that the community as a whole benefits.” The ruling called for nonprofit hospitals to be more proactive in improving health at the community level—a population-centered approach—and legislators and policy experts are now requesting that nonprofit hospitals play a more strategic role in allocating resources for imp...