![]()
PART 1
BASICS
![]()
Basic science
Anatomy
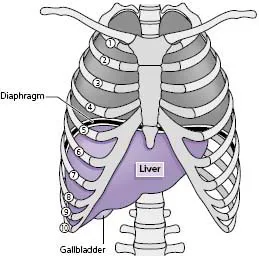
The liver is the largest solid organ in the body weighing approximately 1600 g in men and 1400 g in women. It lies in the right upper quadrant of the abdomen under the rib cage with its upper border between the fifth and sixth ribs and its lower border along the right costal margin where it can sometimes be palpated on inspiration in healthy subjects (Fig. A).
Embryological development of the liver
To understand the anatomy and vascular relationships of the adult liver it is first necessary to review its development.
Hepatic parenchyma
The primitive liver develops in the 3-week-old embryo as an outgrowth from the distal ventral wall of the foregut. This liver bud, or hepatic diverticulum, proliferates into solid cords of endodermal cells which invade the mesenchyme of the nearby septum transversum. A series of branching and anastomosing plates spread between the umbilical and vitelline veins forming a close relationship, which eventually develops into the hepatocytes and sinusoids of the mature liver parenchyma.
Biliary system
The hepatic diverticulum divides, the large cranial part forming the hepatic parenchyma and the smaller caudal part forming an epithelial cord extending from the hepatic parenchyma to the foregut, the eventual duodenum. This solid cord becomes vacuolated forming a lumen first in the common bile duct and then in the hepatic duct, cystic duct and gallbladder. The intrahepatic ducts begin to form from the hepatocytes in direct contact with the mesenchyme at week 9–10. Epithelial and mesenchymal resorption and remodelling occurs, resulting in a network of biliary tubules. Disturbance of this remodelling process is responsible for a number of disorders including congenital hepatic fibrosis, Caroli’s disease and polycystic liver disease.
Venous system
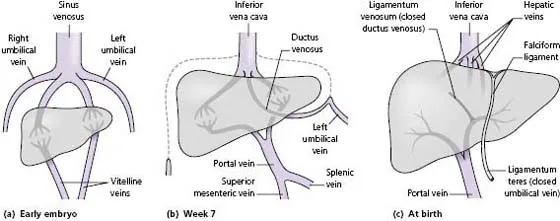
The hepatic venous system develops from four veins: two umbilical veins carrying oxygenated blood from the placenta, and two vitelline veins draining into the sinus venosus (Fig. B (a)). By week 7 the definitive fetal circulation is formed (Fig. B (b)):
- The right umbilical vein and the cranial portion of the left umbilical vein regress and disappear.
- The remainder of the left umbilical vein persists providing the principal source of placental blood.
- A new vessel, the ductus venosus, develops forming a bypass channel connecting the umbilical vein to the inferior vena cava.
- The upper anastomoses of the vitelline veins develop into a single portal vein with left and right branches.
- The distal vitelline veins form the superior mesenteric and splenic veins.
- At birth, blood fow ceases in the umbilical vein, the ductus venosus closes and the portal vein takes over the venous blood supply to the liver. The obliterated segment of the umbilical vein between the umbilicus and the left portal vein branch regresses to form the ligamentum teres, and the ductus venosus becomes a fibrous cord, the ligamentum venosum, running in the right lobe (Fig. B (c)).
Gross anatomy
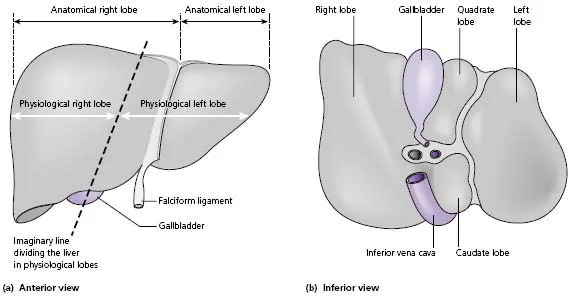
The liver is divided into two uneven lobes, the right and left, by the falciform ligament, which is a remnant of the embryonic umbilical vein. These ‘anatomical lobes’ have no functional significance. The right lobe is larger than the left and contains the quadrate and caudate lobes (Fig. C (a) and (b)). Between the quadrate and caudate lobes is the porta hepatitis or liver hilum. Here the portal vein and hepatic artery enter and the bile ducts leave the liver. In some individuals there is a downward protrusion of the anterior edge of the right lobe of the liver known as Riedel’s lobe*. It may extend into the right iliac fossa and be palpable. It is considered as a normal variant.
Apart from an area on its posterior surface, the bare area, the liver is covered by a fibrous capsule, Glisson’s capsule.† The bare area lies in direct contact with the diaphragm and is surrounded by reflections of peritoneum. The falciform ligament attaches the liver to the diaphragm and anterior abdominal wall. Its anterior portion, the round ligament (ligamentum teres), connects the left branch of the portal vein to the umbilicus. It contains small vestigial veins that can reopen and become varicose if intrahepatic portal venous hypertension develops.
Liver vasculature and functional anatomy
The liver receives about a quarter of the resting cardiac output via a dual blood supply:
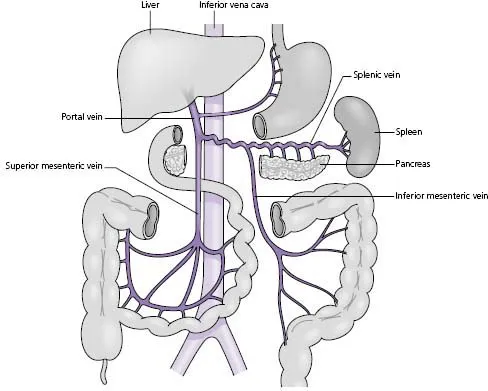
- The portal vein provides approximately 75% of hepatic blood flow. It is formed by the union of the superior mesenteric and splenic veins and drains venous blood from most of the digestive tract, spleen, pancreas and gallbladder (Fig. D).
- The hepatic artery, the second major branch of the coeliac axis, provides the remaining 25% of hepatic blood flow, but 50% of the oxygen supply. The hepatic arteries give rise to branches that supply the biliary epithelium, thus obstruction to arterial flow can result in the development of an ischaemic cholangitis.
The distribution of the hepatic blood supply and biliary drainage divides the liver functionally into two roughly equal ‘physiological lobes’. The line of demarcation between right and left vascular inflow passes along a plane joining the tip of the gallbladder to the groove of the inferior vena cava (see Fig. C (a)). The understanding of this vascular anatomy and the recognition of true right and left lobes is of major importance in radiologically staging hepatic tumours and in surgical resection of the liver.
The liver is drained by three major veins, the right, middle and left hepatic veins. As they emerge from the posterior surface of the liver the left and middle veins usually join, forming a common trunk that drains alongside the right hepatic vein into the inferior vena cava just before it passes through the diaphragm. In addition to the main hepatic veins, small inferior veins drain the posterior segment of the right lobe and the caudate lobe directly into the vena cava. This arrangement protects the caudate lobe from injury and allows it to hypertrophy if the main hepatic veins are occluded (Budd–Chiari syndrome).
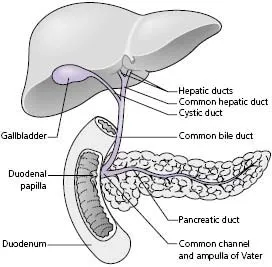
Biliary drainage
Within the hepatic parenchyma bile canaliculi form an anastomosing network between the hepatocytes. They join near the portal tracts and form progressively larger ducts, eventually creating right and left hepatic ducts which leave the right and left liver lobes, respectively. The hepatic ducts meet at the porta hepatis and unite, forming the common hepatic duct. The gallbladder lies under the right lobe of the liver where it stores and concentrates bile. It is drained by the cystic duct, which joins the common hepatic duct to form the common bile duct. The common bile duct runs behind the first part of the duodenum in the groove on the back of the head of the pancreas and enters the second part of the duodenum, usually joining the main pancreatic duct to form a common channel, the ampulla of Vater (Fig. E). The lower end of the common bile duct contains the muscular sphincter of Oddi which prevents bile entering the duodenum in the fasting state. In about 30% of individuals, the bile duct and pancreatic duct open separately into the duodenum.
Intrahepatic organisation
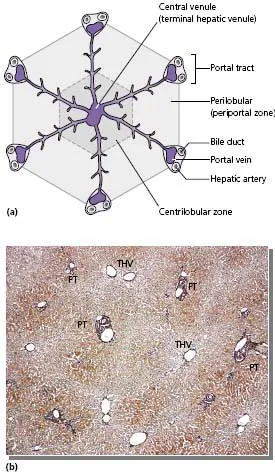
The hepatic artery and portal vein enter the porta hepatitis within a sheath of connective tissue, the gastroduodenal ligament, which also contains bile duct branches as they leave the liver. The vessels run parallel and branch in all directions eventually emptying into the hepatic sinusoids. Blood passes from the portal tract via the hepatic sinusoids to the terminal vein (central vein). The hepatic veins run in the opposite direction to the portal tract with terminal hepatic venules collecting blood from the sinusoids and forming larger channels leading to the main hepatic veins.
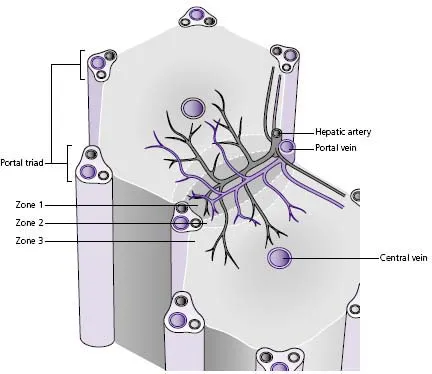
Two models have been proposed for the functional unit of the liver (Figs F and G):
1 The classic lobule (Fig. F) is a hexagonal structure organised around a central venule, a tributary of the hepatic vein, with the portal tracts forming the corners of the hexagon. This model is convenient for describing centrilobular or perilobular structural alterations occurring around the hepatic venule or portal tracts, respectively, but it is not an isolated functional unit.
2 The liver acinus (Fig. G) more accurately describes the functional unit of the liver and describes the hepatic parenchyma in zones:
- Hepatocytes in zone 1 are closest to the portal triad; they receive the richest supply of oxygen and nutrients but are more likely to be damaged by drugs and toxins as they are exposed to higher concentrations of these.
- Zone 3 hepatocytes are near the central vein and have a relatively poor oxygen supply and are therefore particularly susceptible to hypoxic damage.
Tissues of the liver
Hepatocytes
Eighty to 85% of the liver volume is made up of hepatocytes-polyhedral-shaped, polarised epithelial cells. The cells are arranged in plates with the basolateral surface projecting into the perisinusoidal space of Disse where they are in direct contact with cell-free blood.
Cholangiocytes
The bile ducts are composed of epithelial cells, called cholangiocytes. The cells lining the small interlobular ducts are cuboidal, whereas those of the larger bile ducts are columnar, mucus-secreting cells.
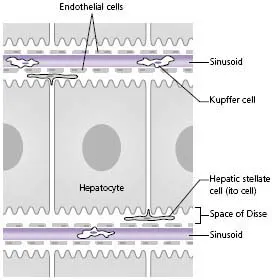
Cells of the sinusoid
The vascular sinusoids are lined by endothelial cells that contain numerous fenestrae allowing free passage of solutes into the space of Disse that lies between the sinusoidal endothelial cells and the hepatocytes (Fig. H). This space of Disse contains perisinusoidal cells, the hepatic stellate cells also known as Ito cells. These are multifunctional cells involved in fat and vitamin storage and with the potential to transform into fibroblasts, which are a major source of extracellular matrix in the normal and diseased liver. Kupffer cells float freely in the lumen of the sinusoids. They are members of the mononuclear phagocytic system and are responsible for the clearance of particles, injured red cells and toxins. Liver-associated lymphocytes can be recruited from the peripheral blood to the liver sinusoids where they mature and acquire natural and lymphokine-activated cell activity.
Lymphatics
Hepatic lymph is formed by drainage of the perisinusoidal space of Disse into lymphatic plexuses of the portal tract. The lymphatic plexuses progressively enlarge as they follow the portal vessels to the portal hepatitis, and the majority drain into hepatic lymph nodes at the liver hilum. Other drainage routes occur via the falciform ligament and epigastric vessels to the parasternal nodes, from the liver surface to the left gastric nodes and from the bare area to the posterior mediastinal nodes.
Nerve supply
Nerve plexuses around the hepatic artery and portal vein provide parasympathetic fibres from the vagus nerve and sympathetic fibres from the coeliac ganglia.
Physiology
Bile formation and excretion
Bile secretion is an important exocrine function of the liver. Bile is a mixture of water, electrolytes, bile pigments (largely bilirubin), bile acids, cholesterol, phospholipids, albumin and immunoglobulins. This composition allows it to have a broad range of physiological functions including lipid digestion and absorption, immunological defence, excretion of endogenous compounds and removal of xenobiotics.
Formation of bilirubin
The body produces approximately 250–400 mg of bilirubin daily, primarily from the breakdown of haemoglobi...