- English
- ePUB (mobile friendly)
- Available on iOS & Android
Implant Site Development
About this book
With the desire for dental implant therapy ever escalating, clinicians are faced with the challenge of augmenting deficient natural physiology to provide effective sites for implantation. Implant Site Development helps the clinician decide if, when, and how to create a ridge site amenable to implantation. This practical book offers solutions to many implant site preservation scenarios, discussing different treatment options, timing, a variety of materials and techniques, and their application to the clinical practice. With a unique integrated clinical approach, Implant Site Development covers a range of site development techniques.
Highly illustrated, Implant Site Development presents diagrams and clinical photographs to aid with clinical judgment and will prove useful for any dental professional involved in implant therapy, from general practitioners to prosthodontists, but especially surgeons. This literature-based, yet user-friendly, reference will be indispensable to the novice or veteran clinician.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
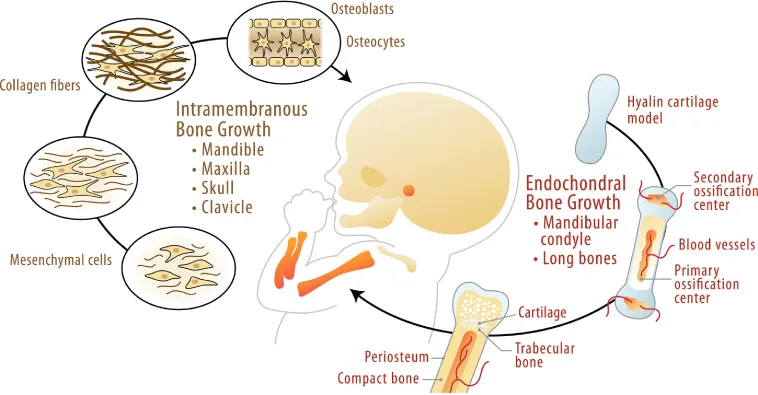
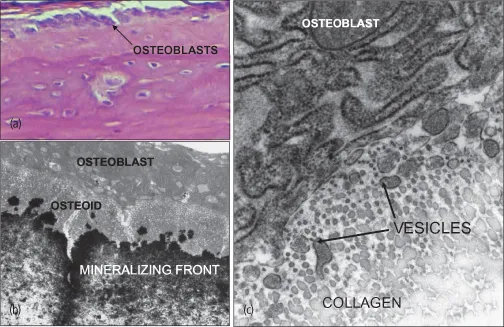
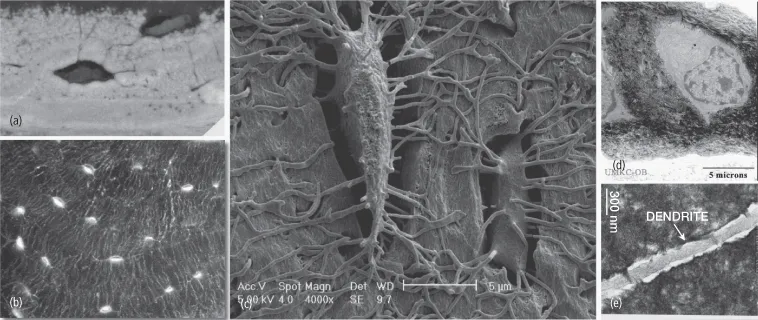
Table of contents
- Cover
- Title page
- Copyright page
- Dedication
- Contributors
- Foreword
- Acknowledgments
- Chapter 1 Principles of bone biology and regeneration
- Chapter 2 Bone anatomy
- Chapter 3 Treatment philosophy
- Chapter 4 Decision-making algorithm for regeneration of the periodontally compromised tooth: Maintaining these teeth when dental implants provide a compelling alternative treatment option
- Chapter 5 The making of beautiful smiles in perio-implantology
- Chapter 6 CT/CBCT diagnosis and treatment planning concepts for bone grafting applications
- Chapter 7 Implant site development: Socket preservation
- Chapter 8 Implant interactions in orthodontics
- Chapter 9 Guided bone regeneration: Concepts and materials
- Chapter 10 Implant site preparation: Horizontal ridge augmentation using particulate allograft and the principles of guided bone regeneration
- Chapter 11 Guided bone regeneration: Peri-implantation
- Chapter 12 Guided bone regeneration: Vertical growth
- Chapter 13 Intraoral bone grafts for dental implants
- Chapter 14 Bone grafting in large bone defects and extreme atrophy situations
- Chapter 15 Sinus elevation: Osteotome-mediated approach
- Chapter 16 Sinus elevation: Lateral wall approach
- Chapter 17 Distraction osteogenesis
- Chapter 18 Immediate implant placement: A comprehensive understanding for achieving optimal clinical success
- Chapter 19 Soft tissue augmentation: Pre-, peri-, and postimplantation
- Chapter 20 Soft tissue enhancement after implant placement
- Chapter 21 Soft tissue augmentation: Allograft
- Chapter 22 Soft tissue development with provisional and definitive implant restorations
- Chapter 23 Bioengineering concepts
- Index
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app