![]()
Section 1
Introduction
| Chapter 1 | Theoretical Frameworks That Support Home Care
By Leslie Neal-Boylan, PhD, RN, CRRN, APRN-BC, FNP |
| Chapter 2 | Managing the Complexities of Home Health Care
By Mary Curry Narayan, MSN, RN, HHCNS-BC, COS-C |
| Chapter 3 | Transitioning
By Jeanie Stoker, MPA, RN, BC |
| Chapter 4 | The Home Visit
By Pamela Teenier, RN, BSN, MBA, CHCE, HCS-D, COS-C, and Lelah R. Marzi, RN, MBA, BSN, COS-C, HCS-D |
![]()
1
Theoretical Frameworks That Support Home Care
By Leslie Neal-Boylan, PhD, RN, CRRN, APRN-BC, FNP
Several theoretical frameworks provide the foundation for home health practice. This chapter will describe those frameworks and lay the foundation for the rest of this book. It is important that home health clinicians use theory to guide their practice so that home care can continue to distinguish itself as a setting of care that is quite different from inpatient settings. Clinicians considering a move into home care should understand that clinical expertise is not automatically transferred to the home care setting. Rather, the clinician must be able to work in an unstructured setting and be confident enough to practice autonomously.
REHABILITATION THEORY
Rehabilitation theory revolves around the concept of self-care management. That is, the patient is encouraged toward maximal self-care. Rehabilitation professionals strive to assist the patient to regain functional independence, if possible. If independence is not possible, then the patient is assisted to do as much as she/he can for her/himself without pain, loss of quality of life, or the progression of disability. Patients are assisted to adapt to the alterations that may be imposed by their disability or illness.
Orem’s (1995) [10] theory of self-care management is one of the theories that are used to support the rehabilitation and restoration of the patient. Orem suggests that the nurse offers wholly compensatory, partly compensatory, or supportive-educative care to the patient. The patient who must have total care because she/he is unable to participate in self-care receives wholly compensatory care, while the patient who can do some things for her/himself receives partly compensatory care. The clinician compensates for the things that the patient cannot do. Supportive-educative care is the ideal. This involves supporting and educating the patient who is able to provide self-care but needs to be taught how and to be supported in efforts to do so.
Henderson’s (1978) [7] theory also revolves around the concept of self-care. The home health clinician stands in or substitutes for those activities or functions that the patient is unable to complete alone. As the patient gets better, the clinician helps the patient convalesce and works in partnership with the patient toward progressing through the plan of care. The clinician also works on the environment to make it malleable to the patient’s needs and abilities. In the case of projected death due to the illness, the clinician assists the patient to make it peaceful and dignified.
Roy’s adaptation model [13] focuses on the adaptation of the patient to the alteration in lifestyle caused by the illness or disability. The clinician’s role is to encourage adaptation and to help the patient channel his/her resources toward adaptation.
THEORIES OF CHRONIC ILLNESS MANAGEMENT
Home care patients are often chronically ill. Consequently, home care clinicians must understand concepts of chronic illness since caring for those who are chronically ill is inherently different from caring for acutely ill patients. The Commission on Chronic Illness (1957) [2] originally outlined certain characteristics that describe someone who has a chronic illness. The illness or impairment caused by the illness:
- Is permanent
- Leaves a residual disability
- Is caused by a nonreversible pathologic condition
- Requires special training of the patient for rehabilitation
- Requires a long period of supervision, observation, or care [2, 6]
Patients with chronic illnesses often gain experience with aspects of their illness such as wound care, procedures, or medications. It is important that the home health clinician respect that knowledge and the routine with which the patient has become comfortable. That is not to say that the clinician (and the ordering provider) will not have better methods. However, if a method needs to be altered, the patient should be taught the reasoning behind the need for change and the patient should be made a partner in the plan of care.
Patients with chronic illnesses live with the consequences of their illnesses all of the time, such as pain, possible disfigurement, reduced function, dependence on others, and the inability to participate in everything they’d like to do. These patients often experience a lack of patience with their symptoms on the part of health care providers, friends, and family. They are often not taken seriously and may tell people they feel well when they don’t so that they don’t disappoint others. They may worry that others will tire of hearing about how they feel or what they cannot do.
Home care clinicians are likely to achieve a rapport and cooperation from chronically ill patients if they allow time to listen to patient concerns and show respect and empathy for what these patients know about how they feel and how they want to be cared for. Patients in home care (as should all patients regardless of setting) should be made to feel that they are equal partners in care particularly because care takes place in the patients’ homes and the patients must be willing to allow the care to be provided. Family members and other caregivers must be recruited to “buy into” the plans for home care so that they can encourage and assist patients to participate.
Some patients with chronic illness may blame others for their misfortune, and other patients may feel that they have done something wrong, such as smoking or gaining weight, to cause their illness. The truth is probably a combination of both, but it is helpful for the clinician to assess the patient’s perspective regarding the illness so the clinician will be able to know how to approach the patient as they work together to proceed through the plan of care.
In order to effect changes in health behaviors to move toward the restoration of function, it is helpful to understand how people perceive health behaviors. This understanding can enable the home care clinician to identify and begin with the patient’s perception so that interventions can be realistic and doable. It is unrealistic to expect a patient to change behavior when they are not ready and willing. However, the clinician can help the patient reach a point of readiness to accept change.
One model of health behavior change is the Health Belief Model (HBM) [3, 12]. The patient must accept that he/she has or can get the disease or condition (perceived susceptibility), then must recognize that the condition is serious and that it has serious consequences (perceived severity). Once the patient has accepted these concepts, he/she must accept that the recommended intervention or treatment can work to reduce the risk of acquiring the disease or reduce its impact. However, the patient must then recognize the perceived barriers (tangible and intangible) that can prevent changing the behavior and be ready to learn about how those barriers can be reduced or eliminated. Cues to action are useful to clinicians to remind patients of the need to change, and self-efficacy is ultimately the confidence one has to take action.
The Shifting Perspectives Model [4] explains how patients switch the perspectives of their illness at any given time. When the patient views wellness as in the foreground, the illness is viewed as an opportunity for growth and for meeting people the patient might otherwise not have met. The person who is thinking this way seems able to separate his/her sense of self from the illness and does not allow the illness to define them. During this time, the person may also neglect to seek health care when they need services because they may avoid allowing themselves to focus on their symptoms.
When illness is in the foreground, the patient’s illness may be tied up with their identity. They may appreciate the secondary gain from having an illness, such as getting attention from others, being excused from activities or responsibilities they do not want to be part of, and avoiding other painful aspects of their lives by dwelling on their illness. This perspective allows clinicians to feel needed by their patients but also fosters patient dependence when the patient should be achieving optimal and maximal self-care management.
HOME HEALTH NURSING THEORY
There are three major theories or conceptual frameworks in home care. The first two are based on the theorists’ experience, anecdotal experience, and reviews of the literature. The last theory is based on a research study of home health nurses.
The Rice Model of Dynamic Self-Determination (1996) [11]
This framework is patient focused and incorporates the patient’s perceptions, motivations, health beliefs, sociocultural influences, support systems, and disease process. As the title suggests, the goal is for the patient to be able to manage their own health care needs and in so doing, achieve personal harmony. The nurse’s role is to facilitate patient independence by educating, advocating, and case managing. The patient and caregiver form a unit and should be cared for in a holistic manner. The nurse, patient, and caregiver move through stages of dependence, interdependence, and independence. They work together in partnership to achieve independence in the home.
The Albrecht Model for Home Health Care (1990) [1]
Albrecht used a review of the literature and her own experience to identify 18 concepts that are interrelated and reflect the dynamic relationships and complex processes of home care. Like the other models used in home care, Albrecht describes the primary goal of home care as patient self-care. (Table 1.1.1)
Table 1.1.1. Albrecht’s 18 Concepts.
| Accessibility | Accountability |
| Availability | Comprehensiveness |
| Continuity | Coordination |
| Cost-effectiveness | Client/consumer |
| Demand | Efficiency |
| Intervention | Nurse |
| Client classification | Productivity |
| Provider | Quality of care |
| Satisfaction | Use of home care |
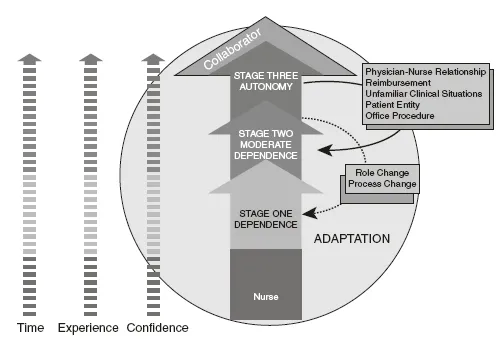
The Neal Theory of Home Healthcare Nursing Practice [8, 9]
The Neal theory is based on a study of practicing home health nurses. Nurses were asked to define their practice. From the research evolved a model consisting of 3 stages: dependence, moderate dependence, and autonomy. The ability to adapt to an unstructured setting enables the clinician to move through the stages toward autonomy. Once the clinician has achieved stage 3, autonomy, it is possible to fall back briefly to stages 2 or 1, because of role changes, process changes, the physician-nurse relationship, reimbursement factors, office procedures, unfamiliar clinical situations, or the influence of anyone or anything that has an influence or potential impact on the patient’s care (patient entity).
The theory is helpful to home health care clinicians because certain characteristics define a clinician who can function effectively in home care, and the theory helps clinicians to see that not everyone can function effectively in the home setting. The ability to adapt is key to being able to move through the stages. Clinicians in different stages will likely handle patient cases differently, and home health agencies can help clinicians to move more quickly through the stages to reach their optimal effectiveness. Each case discussed in this book will further highlight how a nurse in each stage, according to the theory, would act and perform (Figure 1.1.1).
Family Theory
Home health is holistic and very frequently involves the family as the unit of care. Caregivers may or may not be relatives of the patient. Regardless, the people who informally care for the patient, whether related by blood or not, are often the patient’s family for the purposes of home care.
It is important that clinicians in home care understand family theory so that the power and influence of the “family” is not underestimated. A thorough understanding by the clinician can help him/her work with the family in order to attain patient-centered goals.
One family theory is Duvall’s Family Development Theory [5]. Duvall identified 8 stages through which the family proceeds, beginning with the couple separating from their families of origin and ending with the aging family. While, Duvall’s theory needs some updating to reflect families who are not always made up of the traditional heterosexual married couple, the stages through which a couple and, later, a family progress remain largely unchanged. Certain fundamental principles underlie Duvall’s family theory:
- Families progress through predictable stages.
- There are different expectations of the family in each stage.
- The relationships and interactions among family members change as the expectations change.
- Roles change as family members try to fulfill their roles in each stage.
- The family has its tasks to accomplish in each stage, as does each individual.
- The family as a whole must help the family and the individuals accomplish their tasks in order to function effectively as family unit.
- Conflict can result between the tasks of the family and the tasks of the individual.
THE PHILOSOPHY OF HOME CARE
The theoretical foundation of home care rests solidly on a core of patient self-care, functional restoration or substitution, and chronic illness management. The setting of care is in the patient’s home, whether that is the street, a homeless shelter, or a mansion. The environment of the patient’s home influences patient care and the role of the nurse. The environment has both tangible and intangible qualities. The tangible environment includes the building or street, the rooms, the furniture, the hallways, the presence or lack thereof of food or refrigeration, heat, or air-conditioning.
The intangible aspects of the environment are just as important. They include, but are not limited to, the dynamics between the patient and the family and/or caregivers, the knowledge and/or educational level of the patient, the perceptions of the patient and caregivers regarding receiving care in the home and their ability to comply with recommended treatment. Often the environment outside of the home filters inside, such as in the case of an unsafe neighborhood or the lack of neighbor support, community resources, or transportation. However, the environment outside of the home can have positive effects, such as a spiritual community that helps the patient and offers support.
The home setting is inherently different from the inpatient setting. The clinician must be comfortable working in an unstructured setting and in making many autonomous decisions, often without assistance or guidance. The clinician must have excellent communication skills, not only to communicate with the patient and the caregivers but to report efficiently and accurately to the primary care provider and other health care professionals who are involved with the case. Interdisciplinary conferencing and collaboration are even more vital when working in home care than in other settings, because other professionals are not as readily available. Communication must be regular and goal-oriented so that all team members work toward the same goals and reinforce each other’s plans of treatment.
Since care occurs in the patient’s home, the clinician must be certain to partner with the patient and caregivers and make the effort to understand the patient’s routine, what is realistic within the patient’s environment, and what is not possible to accomplish. The clinician becomes very creative and flexible as he/she works with the patient and caregiver to find ways to achieve goals and objectives.
The following 3 chapters will further enlighten the reader regarding the processes of home care and the details that make it so different and so rewarding for both patients and clinicians. The cases that follow these chapters will further illustrate how the home health clinician works to care for patients who have specific needs, conditions, and treatment goals in their home.
[1] M.N. Albrecht, “The Albrecht nursing model for home health care: Implications for research, practice, and education,” Public Health Nursing, 7 (2):118–126, 1990.
[2] Commission on Chronic Illness, Chronic Illness in the United States, Vol. 1, L. Braslow (ed.), Harvard University Press, 1957.
[3] M. Conner and P. Norman, Predicting Health Behavior: Search and Practice with Social Recognition Models, Open University Press, 1996.
[4] R. Davis and J.K. Magilvy, “Quiet pride: The experience of chronic illness by rural older Americans,” Image Journal of Nursing Scholarship, 32(4):385–390, 2000.
[5] E.M. Duvall and B.C. Miller, Marriage and Family Development (6th ed.), Harper & Row, 1990.
[6] S.E. Guillett, “Understanding chronic illness and disability,” Care of the Adult with a Chronic Illness or Disability, L.J. Neal and S.E. Guillett (eds.), pp. 1–10, Mosby, 2004.
[7] V. Henderson, “The concept of nursing,” Journal of Advances in Nursing, 3(2):113–130, 1978.
[8] L.J. Neal (ed.), Rehabilitation Nursing in the Home Health Setting, Association of Rehabilitation Nurses, 1998.
[9] L. Neal-Boylan, On Becoming a Home Health Nurse: Practice Meets Theory in Home Care Nursing, National Association for Home Care, 2009.
[10] D.E. Orem, Nursing Concepts of Practice (5th ed.), Mosby, 1995.
[11] R. Rice, Home Health Nursing Practice: Concepts and Application, Mosby, 1996.
[12] I. Rosenstock, “Historical origins of the Health Belief Model,” Health Education Monographs, 2(4):328–335, 1974.
[13] C. Roy and H.A. Andrews, The Roy Adaptation Model (2nd ed.), Prentice Hall, 1999.
![]()
2
Managing the Complexities of Home Health Care
By Mary Curry Narayan, MSN, RN, HHCNS-BC, COS-C
Home health care nursing is a highly complicated field of nursing practice. Its complexity frequently astounds nurses when they first step into pat...