![]()
1
IF REPRODUCTIVE HORMONES ARE SO IMPORTANT, WHY IS THERE SO MUCH VARIATION?
When it comes to the area of fertility, many people, including some health professionals, believe that women of reproductive age can be divided into two groups: those who are fertile, and those who are not. The group with fertility problems is very diverse, as medical science today can identify numerous anatomical, genetic, physiological, and metabolic disorders leading to fertility impairments. The group of healthy, fertile women is considered much less interesting, especially if they have regular menstrual cycles, because they can conceive children without assistance, which places them beyond the interest of medical professionals specializing in reproductive health. What the medical field is not taking into account, however, is that healthy, fertile women who have no reproductive disorders still differ in many ways in their reproductive physiology. This variation is interesting and important for several reasons.
First, the variation contributes to differences in fertility (i.e., the number of children women have). It is not true that all healthy women can have a similarly large number of children so long as they do nothing to control their fertility. Women from populations with natural fertility—that is, fertility achieved without contraception or other methods of family planning—show significant variation in the number of children they have during their reproductive lives (Campbell and Wood 1988; Bentley, Goldberg, and Jasienska 1993; Bentley, Jasienska, and Goldberg 1993). The underlying causes of such variations are, to a large extent, biological: they result from differences in ovarian function. These differences, in turn, result mainly from the impact of the environment in which women live, especially from the factors that determine how much metabolic energy women have and can allocate to reproduction.
Variation in reproductive function among healthy women in response to the environment—which in humans we can call “lifestyle”—is believed to reflect the ability of reproductive physiology to react in a way that is biologically appropriate, or, in the language of evolutionary biologists, adaptive. Peter Ellison (1990, 2003b) has stressed that temporarily suppressed reproductive function, and thus a temporarily reduced ability to conceive, is an adaptive response to preserve the long-term ability of a mother to bear children in the future. This aspect of variation in ovarian function is particularly interesting for those who study evolutionary biology and life-history theory, for short-term suppression may affect reproductive success, which is how biological fitness is measured.
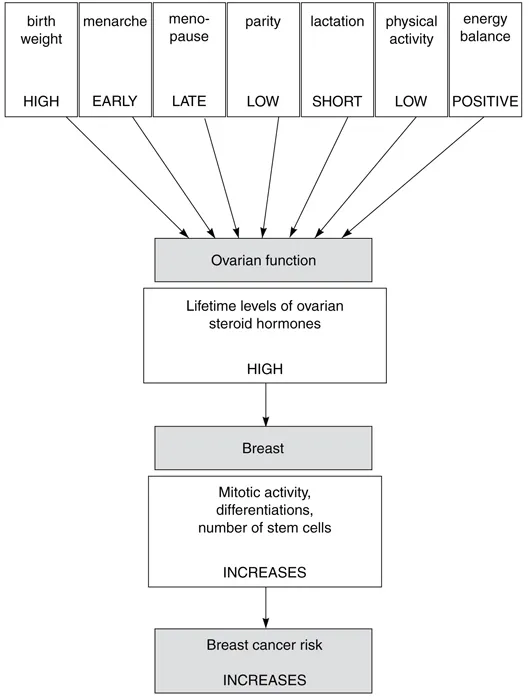
Appreciating the existence of variation in reproductive function is useful for many other theoretical areas as well: for example, it may help explain certain demographic trends. It is especially important for all aspects of health and disease prevention in women. The impact of variation in reproductive function is obvious in terms of fertility, but circulating levels of reproductive steroid hormones are also important determinants of other aspects of health and disease, which gives knowledge about variation in ovarian function practical implications for disease prevention. Extensive research notwithstanding, variation in the incidence of breast cancer and other hormone-dependent cancers (such as uterine and ovarian cancers) is only to some extent explained by the established risk factors for these diseases. Reproductive steroid hormones are important players in the development and progress of these cancers, and knowledge of a woman’s lifetime exposure to these hormones may help to predict her risk (Figure 1.1).
Levels of hormones are fortunately not set for life. They can be manipulated not only by medical intervention but also by the woman herself, often through relatively simple changes in her lifestyle. Therefore, the risk of hormone-dependent diseases can, theoretically, be manipulated as well. But to do that efficiently, the determinants of hormone levels need to be established and their interactions well understood.
Variations in levels of endogenous hormones—those produced in our body—may be responsible for variations in tolerance of exogenous hormones—those used in contraception, hormone replacement therapies, and medication. Interpopulation variation in response to synthetic, hormonal contraception has been well established (Vitzthum and Ringheim 2005). Gillian Bentley (1994) has suggested that tolerance of high doses of contraceptive steroids may depend on a women’s own endogenous levels, so the recommended standard doses are much too high for women from many non-Western populations. Such high doses are not only unnecessary for the effectiveness of contraception but often are not well tolerated and may be associated with unnecessarily elevated health risks.
Figure 1.1. Most factors that increase the risk of breast cancer contribute to the elevated lifetime levels of ovarian steroid hormones.
The severity of perimenopausal symptoms (hot flashes, sleep problems, anxiety, irritability, and depression occurring before and during the menopausal transition when levels of reproductive hormones substantially decline) varies among women from different countries. Such differences may also be explained by variation in hormone levels produced throughout life in menstrual cycles. Women whose physiology is “used to” high levels of ovarian steroids may experience more severe problems when ovarian production diminishes than women who were never exposed to such high levels during their reproductive years.
Women from Japan and mainland China report some menopausal symptoms—in particular, hot flashes—less frequently than women from Canada and the United States (Kaufert et al. 1986; McKinlay and McKinlay 1986; Lock 1993; Ikeda et al. 2005; Shea 2006). Perhaps cultural customs prohibit Asian women from complaining, and perhaps a diet rich in soy products alleviates these problems, but the role of differences in lifetime hormonal exposure is clearly worth further investigation. In a multiethnic study conducted in the United States, Chinese and Japanese participants had lower serum estradiol concentrations than Caucasian, Hispanic, and African American women (Lasley et al. 2002; Randolph et al. 2003). Women in rural China have lower average estradiol levels than British women in the United Kingdom (Key et al. 1990), and Chinese women from Shanghai have about 20 percent lower estradiol concentrations than white women from Los Angeles (Bernstein et al. 1990). This variation in hormone levels seems to correspond to differences in the severity of some menopausal symptoms observed among these populations.
It is important to note, however, that while there is a great diversity in menopausal symptoms in women from different populations, it is not at all clear that women from industrialized countries experience a higher frequency of such symptoms (Obermeyer 2000). Considerable variation in the frequency of menopausal symptoms can also be observed among different Asian populations. The Pan-Asia Menopause Study, which compared symptoms associated with menopause among women from nine populations, including China, Hong Kong, Indonesia, Korea, Malaysia, Pakistan, Philippines, Singapore, Taiwan, Thailand, and Vietnam, found that hot flashes were reported by only 5 percent of Indonesian women, versus 47 percent of Korean women and 100 percent of Vietnamese women (Haines et al. 2005). These results need further verification because the Pan-Asia Menopause Study had only small sample sizes in some of the investigated populations (which could greatly affect the precision of the estimates of relative frequencies). Further reliable hormonal data for a larger number of populations are needed to test the hypothesis that population variation in menopausal symptoms can, at least partially, be explained by variation in the levels of reproductive steroid hormones in women’s menstrual cycles.
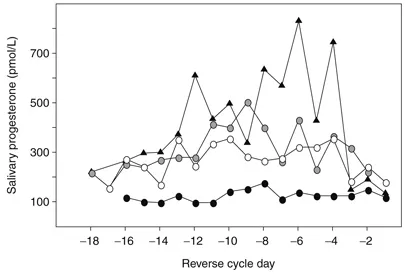
Figure 1.2. Interindividual variation in progesterone profiles: four healthy, regularly menstruating women of comparable age from the same population.
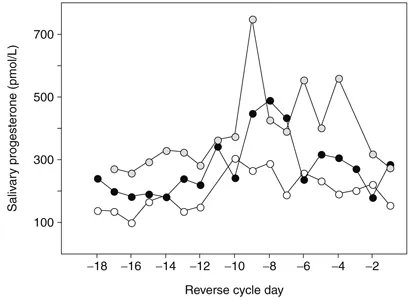
Steroid hormones, especially those produced by the ovaries, are important for many aspects of female health, well-being, and reproduction. High levels of ovarian hormones in menstrual cycles are crucial for successful pregnancy and, as such, are important determinants of female reproductive success. However, not all women have similar levels or high levels of these hormones. There are substantial differences in the mean levels of estradiol and progesterone among populations, among women within a single population, and even among menstrual cycles of a single woman (Jasienska and Jasienski 2008). For example, urban women in the United States have progesterone levels that are on the average 65 percent higher than those of women in the Democratic Republic of Congo (Ellison et al. 1993). In a small village in Poland, we found substantial differences in the progesterone levels among women (Figure 1.2), and also among the cycles of a single woman (Figure 1.3). Such high variation is probably caused, in this population, by the seasonality of agricultural workload; progesterone levels are suppressed during the months with intense energy expenditure in comparison with the months with less intense work. Even in urban women from the United States and Great Britain, where lifestyle is much less influenced by seasons than in agricultural populations, progesterone levels can vary substantially from cycle to cycle (Lenton et al. 1983; Sukalich, Lipson, and Ellison 1994; Gann et al. 2001).
Figure 1.3. Intraindividual variation in progesterone profiles: three consecutive cycles of the same woman.
Production of Reproductive Hormones: The Menstrual Cycle
The major proportion of reproductive hormones that women produce during their lives comes from processes that occur during menstrual cycles. The body also has other ways to produce these hormones: they can be made by the placenta during pregnancy or converted from other hormones by fat tissue. For most women, especially in Western countries, menstrual cycles are the most important in terms of the amount of hormones produced during a lifetime.
I will briefly describe the events that occur during an ovulatory menstrual cycle. It is important to remember that “real life” cycles may differ from this example: not all cycles are ovulatory, and considerable variation exists in the length of the cycle and its phases.
The menstrual cycle lasts twenty-eight days on average and comprises two phases: the follicular phase, which begins with the first day of menstrual bleeding and lasts until ovulation, and the luteal phase, which begins after ovulation and lasts until the last day before menstrual bleeding (Hawkins and Matzuk 2008). During the follicular phase, the main goal is to yield a mature follicle that will be able to release an egg in a process called ovulation. The follicle consists of an egg cell, called the oocyte, and two main types of supporting cells: granulosa cells and theca cells. At the beginning of each cycle, about fifteen to twenty primordial follicles start to grow and develop. Usually only one of them, the dominant follicle, will go through all stages of development and become a fully mature follicle. Primordial follicles, each with an oocyte inside, are produced through divisions of germ cells during fetal development; a human female is born with approximately 7 million of these follicles. After a woman is born, no new follicles will develop in her body, and the supply of follicles gets smaller with time.
The menstrual cycle needs the well-coordinated activity of several physiological partners: the hypothalamus, the pituitary, the ovary, and the endometrium or uterine lining. The hypothalamus, a part of the brain, secretes gonadotropin-releasing hormone (GnRH). The pituitary, an endocrine gland located at the base of the brain, secretes luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Secretion of these two pituitary hormones is stimulated by GnRH. The ovary itself secretes estradiol, progesterone, and inhibins. The endometrium is lining of the uterus, which grows under the stimulation of ovarian hormones in preparation for possible implantation of a fertilized egg.
At the beginning of the cycle, levels of FSH increase and stimulate the maturation of primordial follicles, which develop from primordial germ cells. Each follicle begins to produce steroid hormones. The theca cells in a follicle secrete androgens (under stimulation by LH), which are converted by granulosa cells to estradiol. As already mentioned, the dominant follicle usually grows faster and produces more estradiol than the other follicles. Estradiol exerts a suppressing effect on FSH production, and, in addition, the dominant follicle produces the hormone inhibin, which further lowers FSH production. As the levels of FSH diminish, all nondominant follicles without support of this hormone cannot continue further development and gradually die.
The dominant follicle continues to grow and secretes an increasing amount of estradiol. When the concentration of estradiol reaches a high level, it stimulates the pituitary to produce large amounts of LH (the LH surge). Under stimulation of LH, the follicle undergoes biochemical changes that cause it to rupture and expel the mature egg. The egg begins its journey toward the uterus via a duct called the fallopian tube, where fertilization occurs. The fertilized egg starts to develop immediately, and after a few days it is ready to implant in the uterus. The remains of the dominant follicle form the corpus luteum, which starts to secrete another steroid hormone—progesterone. Progesterone further prepares the lining of the uterus, which has already thickened under stimulation of estradiol, to be ready for implantation.
If fertilization has not occurred, the corpus luteum continues its production of hormones for about two weeks and then dies. Without support from progesterone, the uterus sheds its lining, which causes menstrual bleeding. Low levels of estradiol and progesterone during that time stimulate the hypothalamus and pituitary to produce their hormones, which in turn causes new recruitment of primary follicles, and a new cycle begins.
Hormone Levels and Chances of Conception
Two main reproductive steroid hormones produced during menstrual cycles, 17−β estradiol and progesterone, are involved in processes leading to ovulation, fertilization, and implantation of the fertilized egg. Their levels are important for the successful completion of these processes; as such, they are directly responsible for the establishment of pregnancy. Estradiol levels correlate with follicle size and with oocyte quality, and are related to the morphologic features and thickness of the endometrium (Eissa et al. 1986; Dickey et al. 1993; Lamb et al. 2011). Low levels of estradiol are associated with diminished penetrability of mucus in the female reproductive tract by sperm cells, which in turn contributes to reduced fertility (Roumen, Doesburg, and Rolland 1982; Katz, Slade, and Nakajima 1997). Progesterone is essential for endometrial maturation; the higher levels this hormone reaches, the more complete the transformation of the endometrium in preparation for implantation of a fertilized egg (Santoro et al. 2000). During the first half of the cycle, the follicular phase, progesterone also seems to be important because it controls the proliferation and differentiation of the granulosa cells (Chaffkin, Luciano, and Peluso 1993).
It is understandable that a lack of progesterone production during the luteal phase would make implantation impossible, or that the absence of ovulation means that conception will certainly not occur. However, is more subtle variation in the levels of hormones important? If the cycle is ovulatory and estradiol and progesterone are produced, is the quantity of the produced hormone really that crucial? In the medical world, cycles are often merely classified as ovulatory or nonovulatory, and moderate variation in the hormone levels observable during ovulatory cycles is considered uninteresting and unimportant. We cannot know whether such variation is important until we show that cycles varying in levels of these hormones have corresponding variation in the probability of pregnancy. Only such a finding would prove that variation in hormone levels has functional importance.
In a group of white U.S. women who were attempting to become pregnant, women were more likely to conceive during menstrual cycles with higher levels of follicular estradiol (Lipson and Ellison 1996). In other words, these women could not become pregnant during some of their cycles. When hormones in saliva samples were measured, it became clear that nonconception cycles did indeed have lower levels of estradiol than cycles of the same women that ended in pregnancy. In the women who participated in this study, the average estradiol levels during the menstrual cycle were associated with a 12 percent probability of conception, while a 37 percent rise in estradiol levels led to a threefold increase in the probability of conception (to about 35 percent). In healthy Chinese women who were trying to conceive, cycles characterized by higher levels of estradiol resulted in higher rates of conception (Venners et al. 2006). Progesterone levels, especially during the midluteal phase, are also positively correlated with the chance of successful conception (Lu et al. 1999).
We may conclude that it is a well-established fact that, among women from the same population, lower levels of ovarian hormones lead to a lower chance of concepti...