This is a test
- 248 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Adult Palliative Care for Nursing, Health and Social Care
Book details
Book preview
Table of contents
Citations
About This Book
In this far-ranging textbook on palliative and end of life care, John Costello and a team of palliative care specialists take a patient-centred approach. Discussing palliative and end of life care across a range of diseases and illnesses, each chapter includes real-life case studies that focus on both the patient experience and the experiences of the family members of service users. Original in its approach to palliative and end of life care, Adult Palliative Care focuses on a range of non-cancer conditions. Thoughtfully balancing theory with practice, and interprofessional in its scope, Adult Palliative Care would benefit any health professional dealing with or working in the field of palliative and end of life care.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Adult Palliative Care for Nursing, Health and Social Care by John Costello, John Costello in PDF and/or ePUB format, as well as other popular books in Medicine & Nursing. We have over one million books available in our catalogue for you to explore.
Information
Part I Palliative Care Practice
1 The Experience of Living With Cancer
Learning Outcomes
- Become aware of how a cancer diagnosis impacts on service users/patients and those who are important to them
- Be able to consider the implications of the cancer experience
- Have the opportunity to reflect on their professional relationship with patients who have cancer
- Recognise the importance of empathy in the management of patients with a life-limiting illness
Introduction
There are an increasing number of people surviving cancer (Macmillan, 2013), although evidence suggests that these survivors do not always have their personal needs met by professionals. Moreover, it has been reported that one in three cancer survivors find that many of their needs for cancer treatment and care go unmet (Morgan, 2009). These findings are supported by National Patient Reported Outcomes Measures (PROMs) which found that post cancer treatment patients had poorer quality of life scores when compared to the general population (Glaser et al., 2013). This chapter therefore focuses on the important perspective of the patient, focusing on the author’s personal experience of cancer.
It begins with background information on the incidence, causation and epidemiology of cancer diagnosis in the UK, highlighting the most common cancers. It also looks briefly at some of the causes of cancer while recognising that not all cancers have known causes. The chapter looks at how nurses and others can help and support the patient throughout the treatment as well as post treatment and how the individual can help take control of their life after cancer treatment. Because the chapter reflects on personal experience, use of the first person pronoun ‘I’ will be used throughout as it reflects on the writer’s personal experience from the initial diagnosis, through treatment and then describes coming to terms with the impact cancer had on her life.
Incidence of Cancer
Cancer Research UK (2016a) estimates that, for those born after 1960, one in two will develop cancer at some stage of their life. A common misconception about cancer is that a cancer diagnosis means a terminal illness. However, as the evidence suggests, more and more people are surviving cancer. The cancer charity Macmillan (2013) has stated that in 2013 there were 2.5 million people living with cancer in the UK and this was projected to rise to 4 million by 2030. At the same time, Macmillan’s Recovery Package (2013) identifies positive steps that can be taken to allow patients to return to some ‘normality’. Not only will this help with their mental wellbeing, it will allow them to lead as healthy and active life as possible for as long as possible.
There are over 200 types of cancer but the most common cancers are breast, prostate, lung and bowel which account for 53 per cent of all cancers (Cancer Research UK, 2016a). Figure 1.1 identifies the 20 most common cancers according to Cancer Research UK (2016b).
Causative Factors for Cancer
A cancer diagnosis is more likely as one gets older. The peak age at which cancer occurs is age 85+ while half of cancers are diagnosed in people aged 70 or over. However, Cancer Research UK (2016a) has also noted increases in cancers at younger ages too (see Figure 1.2).
Apart from age there are certain lifestyle factors that increase the risk of cancer. The key ones are smoking, poor diet, being overweight and lack of exercise. Cancer Research UK (2016a) estimates that 42 per cent of cancers are preventable. Ensuring a healthy lifestyle significantly reduces the risk of getting cancer (NHS Choices, 2017). In some cases, however, the cause of the cancer is not known.
Interestingly, in my case the type of cancer I developed was not linked to any of the above factors! I was in my fifties, happily married with three grown-up step daughters. I worked as a GP practice manager, a job I loved. I was very fit. I was a keen cyclist and often went on cycling holidays. I also liked walking and went to keep fit classes. I had never smoked, drank very little alcohol, ate healthily and had never been overweight. However, one day my life was to change when I began my cancer journey.
Figure 1.1 Twenty most common cancers in 2014
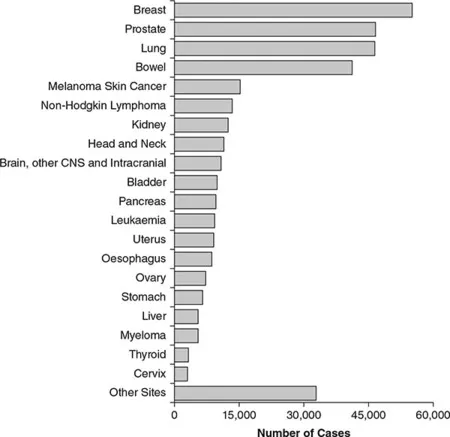
Source: Reproduced with kind permission of Cancer Research UK
Getting Diagnosed: My Experience
In my case it all began one day with a sneeze. One morning as I was about to say goodbye to my husband and head off to work I suddenly gave an almighty sneeze. I immediately said, ‘Oh my back!’ I thought I’d pulled a muscle as a result of the sneeze. I went to work as usual but over the next few days the pain got worse. Thinking I’d pulled a muscle I decided to have physiotherapy. Initially this seemed to help but then the pain got worse.
I was still going to work but because of the pain I couldn’t drive so became reliant on my husband or daughter taking me. I found it impossible to lift things, even a full kettle or my briefcase. I was taking increasing amounts of over the counter pain killers. In the end I had to stop them because they caused severe stomach pains. One day I came out of the physiotherapist in tears as the pain was so bad. I had been for early morning appointments and then going straight to work but that day I knew I couldn’t cope any more and told my daughter to take me home.
Figure 1.2 All cancers (C00-C97 Excl. C44), average number of new cases per year and age-specific incidence rates per 100,000 population, UK, 2013–2015
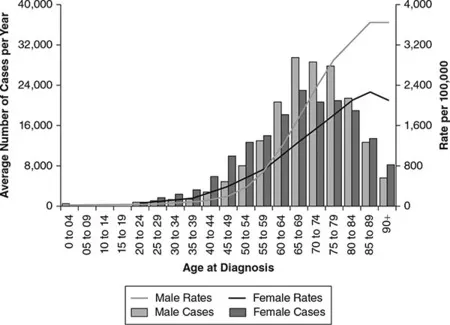
Source: Reproduced with kind permission of Cancer Research UK
I managed to get an emergency appointment with the registrar at the GP practice. She prescribed stronger pain killers and sent me for a back X-ray. Because of the severe pain I decided to see an orthopaedic consultant privately. I went to the GP practice to collect the referral letter and, if possible, a copy of the X-ray report. The X-ray showed that I had two collapsed vertebrae and that my back was ‘highly paretic for a woman of her age’ (i.e. I had developed osteoporosis). The GP asked why I was bothering to see a consultant as he’d probably just put me on calcium tablets!
The following day I saw the orthopaedic consultant who measured my height and I was horrified to discover I had lost 2 inches. He realised that I was in considerable pain and said he wanted to admit me in order to carry out tests. The following morning I received a telephone call from the hospital to ask if I could have an MRSA test prior to admission. A couple of days later I was told it was clear and to come to the hospital the following morning.
After admission I had various tests and scans including a radioisotope scan, an MRI scan, X-rays, etc. The consultant orthopaedic surgeon, I realised afterwards, was looking for a tumour but couldn’t find anything. He brought in the consultant rheumatologist because of the osteoporosis, and he requested a urine sample to undertake a Bence Jones test, but I did not know the significance of this until later. This is a urine sample test for a protein called Bence Jones (or free light chains), where the body produces antibodies that are incomplete. The presence of any Bence Jones protein in urine suggests an abnormality. These free light chains can cause damage to the kidneys, which is why the presence of this protein is an indicator of myeloma.
I spent a month in hospital. During this time I became quite immobile due to the severe back pain. I was fitted with a back brace, which needed to be put on before I could get out of bed. It took two nurses to get me out of bed each morning and to ease me into it at night. I was unable to shower because of the pain and so during this time was given a shower by one of the nurses. I found the experience of being washed by someone extremely embarrassing although I know for nurses it is an everyday occurrence. This was not helped by the fact that while in the shower another nurse came in to discuss her pay slip and left the door ajar while doing so!
On discharge I had real difficulty going up and down stairs and in dressing. When I had a shower I struggled to lift my hands above my head to wash my hair. I found it hard to get in and out of a chair. One day I tried to open a tin of beans for my lunch and didn’t have the strength to use the can opener.
A month after discharge I went to see the consultant rheumatologist. I was doing a little bit at work but was keen to get back to work full time and wanted to know when the treatment for the osteoporosis would allow me to do so. It was then he told me that he’d had the result of the Bence Jones test which showed I had multiple myeloma. I had vaguely heard of myeloma, but knew nothing much about it. My husband had never heard of it. This is not surprising as Myeloma UK estimate that 97 per cent of the population have never heard of myeloma despite it being the second most common form of blood cancer.
The consultant rheumatologist said that I needed to see a haematologist and, as there was a clinic at the hospital that day, he’d ring the haematologist to see if I could be fitted in to the clinic. An hour later I saw the haematologist who said I had light chain myeloma and explained very clearly what it meant.
Multiple Myeloma
Myeloma, also known as multiple myeloma, is a type of cancer arising from plasma cells. Plasma cells form part of the immune system and are found in the bone marrow. Normal plasma cells produce antibodies to fight infection. In myeloma, abnormal plasma cells release one type of antibody which has no useful function (Manier et al., 2017). Myeloma is different from many other cancers as it does not exist as a lump or tumour; instead abnormal plasma cells multiply and expand within the bone marrow. Myeloma affects multiple places in the body, hence the term multiple myeloma. A large majority of myeloma patients will have IgG or IgA myeloma. This is where the body produces too many of one type of heavy chain antibodies. Free light chain myeloma accounts for about 20 per cent of patients and is where the body produces antibodies that are incomplete – the Bence Jones protein.
One of the most important factors in achieving positive outcomes following a diagnosis of cancer is the speed of obtaining a diagnosis and starting treatment. In the case of myeloma, diagnosis is often quite delayed. This is because in many cases the symptoms, such as fatigue and back pain, are vague and could apply to many illnesses. Lyratzopoulos et al. (2012) identified myeloma as the most difficult of all cancers to diagnose. Indeed 10 per cent of patients die within 60 days of diagnosis (Myeloma UK, 2018). Rapid diagnosis is key to ensuring fewer complications, improved quality of life and better survival outcomes.
The time frame from the initial sneeze to getting a diagnosis of myeloma was about three months. This compares favourably to many patients who are subsequently diagnosed with myeloma as 51 per cent o...
Table of contents
- Cover
- Half Title
- Publisher Note
- Title Page
- Copyright Page
- Contents
- About the Editor and Contributors
- Acknowledgements
- Introduction
- Part I Palliative Care Practice
- 1 The Experience of Living With Cancer
- 2 Palliative Care for People With End Stage Pulmonary Disease
- 3 Palliative Care for People with End Stage Heart Failure (ESHF)
- 4 Palliative Care for People with Multiple Sclerosis
- 5 Patients with End Stage Renal Failure
- 6 Palliative Care for People With Advanced Dementia
- Part II Support for Families and Caregivers
- 7 Symptom management: the medical perspective
- 8 Supporting families and lay caregivers on the palliative care journey
- 9 Grief, bereavement and spirituality
- 10 Ethical dilemmas in palliative care
- 11 Hospital palliative care teams
- 12 End of life care in the community
- Conclusion: the case study approach
- References
- Glossary of terms
- Index