What Is Osteonecrosis of the Jaws?
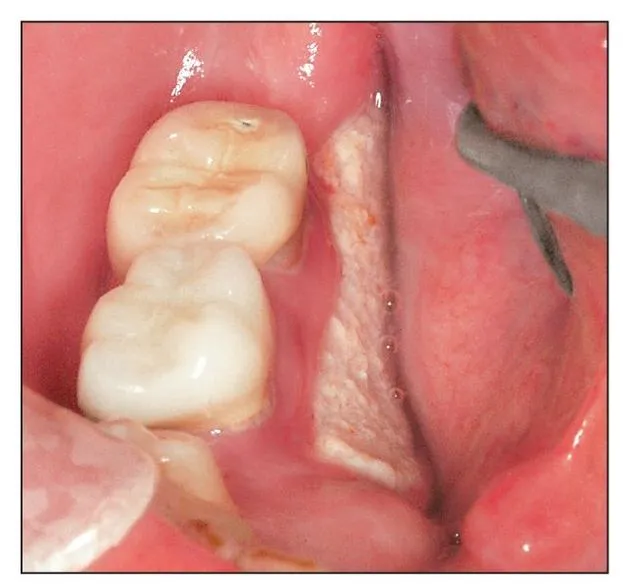
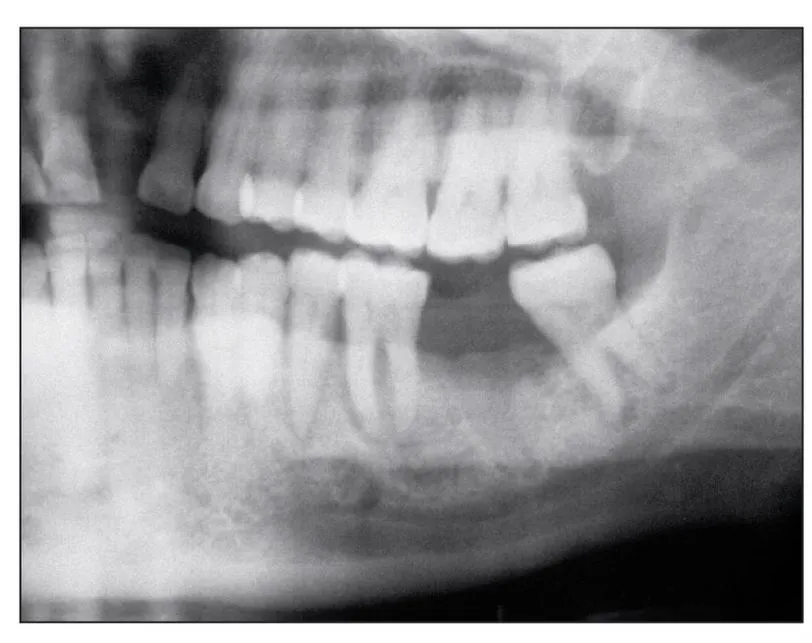
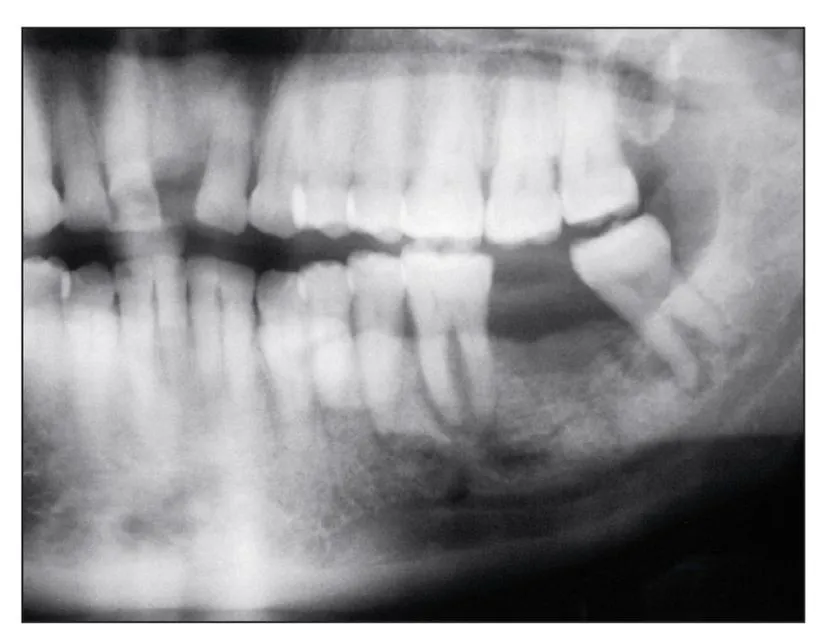
Bisphosphonate-induced osteonecrosis of the jaws refers to a condition characterized by exposure of bone in the mandible or maxilla persisting for more than 8 weeks in a patient who has taken or currently is taking a bisphosphonate and who has no history of radiation therapy to the jaws.1 However, while the exposed bone is indeed dead (osteonecrosis), bone death is actually a secondary result of bisphosphonate bone toxicity, which is similar to the genetic disease osteopetrosis, as explained in chapter 4. Clinically, the disease presents as exposed alveolar bone that occurs spontaneously (Fig 1-1a) or becomes evident following an invasive surgical procedure such as tooth removal (Fig 1-1b), periodontal surgery, apicoectomy, or dental implant placement. The disease manifests mostly in the jaws. To date, it has not been reported in other skeletal sites as exposed bone; however, recent reports have identified femur fractures caused by long-term use (6 years or more) of alendronate (Fosamax, Merck)2,3 (Fig 1-2). Osteonecrosis of the jaws always originates in the alveolar bone and may then extend to the basilar bone or ramus (Figs 1-3 and 1-4). Occasionally, early subclinical radiographic signs—including sclerosis of the lamina dura (Fig 1-5), loss of the lamina dura (Fig 1-6), and/or widening of the periodontal ligament space (Fig 1-7), particularly in association with molars—have been observed.
Fig 1-1a Spontaneous bone exposure of the lingual cortex in the mandibular molar region is a common presentation of bisphosphonate-induced osteonecrosis of the jaws.
Fig 1-1b Nonhealing exposed bone developed after the removal of a maxillary central incisor and the adjacent lateral incisor.
Fig 1-2 Atypical fracture of the femur caused by extended use of alendronate (Fosamax).
Fig 1-3a Radiographic osteosclerosis in the alveolar bone of the mandibular second molar socket.
Fig 1-3b As bisphosphonate-induced osteonecrosis persists, it usually exhibits osteolysis and extends toward the inferior border.
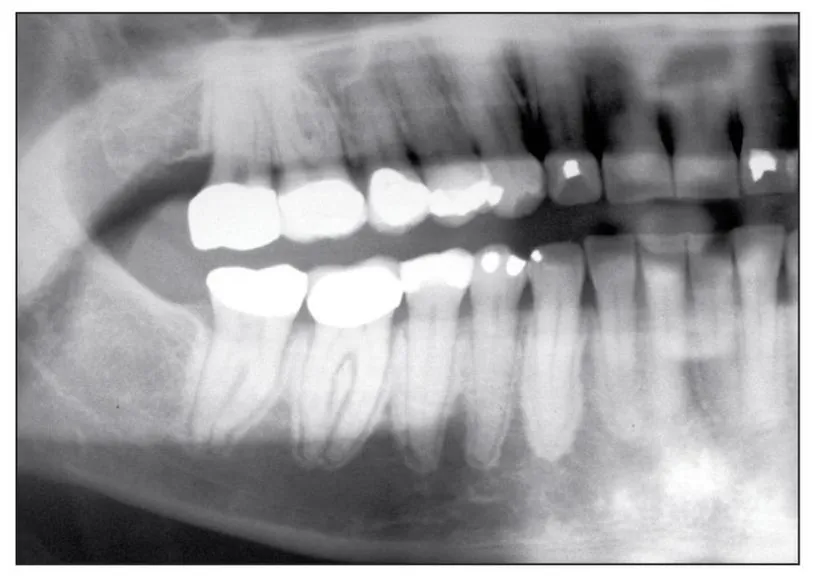
Fig 1-3c Persistent bisphosphonate-induced osteonecrosis. Osteolysis and osteosclerosis become more evident.
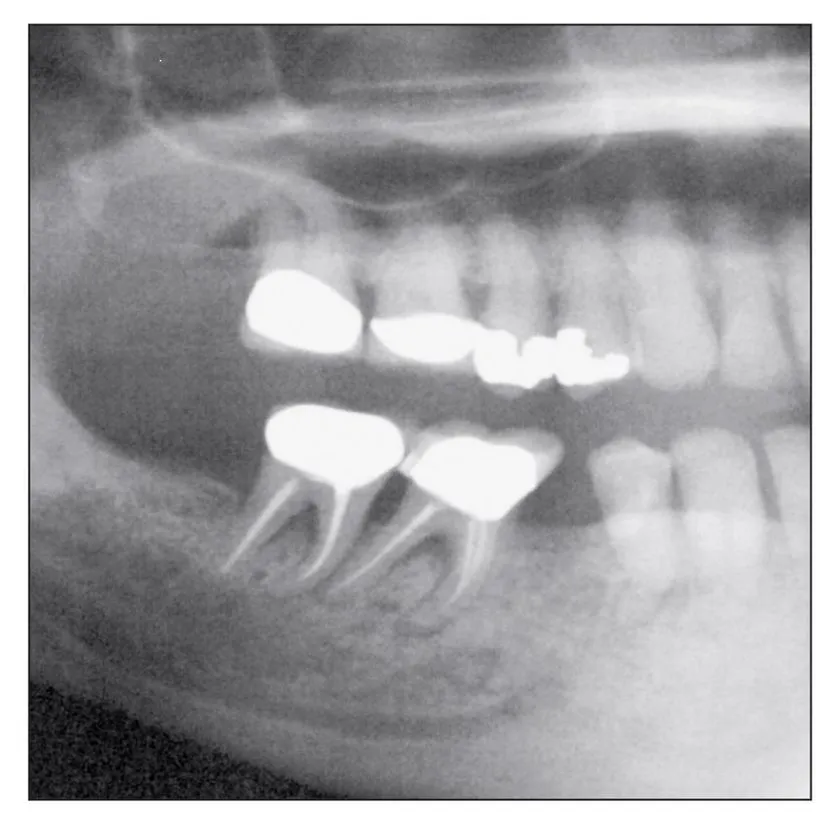
Fig 1-3d Further continuation of the bisphosphonate-induced osteonecrosis accompanied by secondary infection can extend into the inferior border, posing a risk of pathologic fracture.
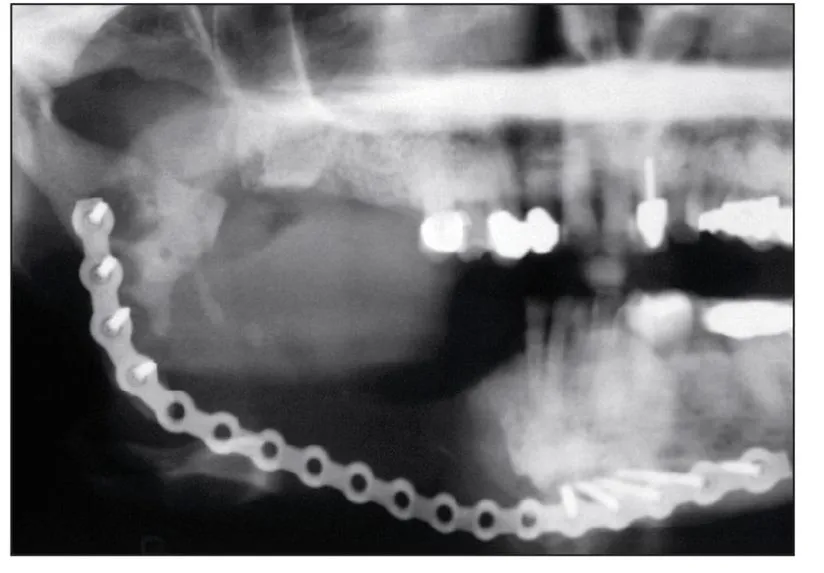
Fig 1-4 Even after a hemimandibular resection, evidence of bisphosphonate-induced osteonecrosis remains in the ramus and condylar neck.
Fig 1-5 Sclerosis of the lamina dura may be seen before exposed bone develops; this is an early sign of bisphosphonate toxicity to the alveolar bone.
Fig 1-6 In some cases, loss of the lamina dura can be an early sign of bisphosphonate toxicity to the alveolar bone.
Fig 1-7 Widening of the periodontal ligament space may be an early or overt sign of bisphosphonate toxicity to the alveolar bone and may also be associated with significant osteolysis.
Early Reports of Bisphosphonate-Induced Osteonecrosis of the Jaws
Bisphosphonate-induced osteonecrosis of the jaws was first described by Marx and Stern in 2002.4 At that time, it was only a curious finding of exposed, nonhealing bone; when debridement was performed, the condition worsened and led to increased amounts of exposed bone. All of the patients described in that report were receiving pamidronate (Aredia, Novartis) for control of malignant tumor deposits in bone. The profession was first formally notified of this drug complication in a medical alert published by the author in 2003 in the Journal of Oral and Maxillofacial Surgery (JOMS), which described 36 cases associated with intravenous bisphosphonates (pamidronate or zoledronate [Zometa, Novartis]).5
Prior to the publication of this medical alert, representatives of Novartis, which produces the two intravenous bisphosphonates (pamidronate and zoledronate) that cause this form of osteonecrosis, were invited to examine 2 of the patients and to discuss the other 34 who were being seen. Although they expressed concern about the plight of these patients, the Novartis representatives denied the possibility that the osteonecrosis was in any way connected with their drugs, because no evidence of bone necrosis was found in their preclinical animal studies or in the more than 3,600 patients enrolled in their human clinical trials. They attributed the bone exposures to the chemotherapy these patients had received and possibly to the dexamethasone that had been given to about 55% of their patients. During that visit, the medical director of Novartis, Dr Peter Tarassoff, was given an advance copy of the medical alert. When it appeared in JOMS, Dr Tarassoff and his Novartis coauthors had already issued a retort strongly denying any causal relationship between the intravenous bisphosphonates produced by Novartis and the osteonecrosis observed in the jaws of these patients.6
The toxicity of chemotherapy was a natural and convenient culprit to blame. Indeed, the very issue of JOMS that carried the medical alert also carried a report by Wang et al of three cases of bone necrosis in the mandible that they too attributed to chemotherapy.7 Yet, it was reported that all three patients had been taking Aredia. Realizing their oversight, these authors later published a retraction article identifying Aredia as the cause of the exposed bone.8 Shortly afterward, compelling findings were reported in the November 2005 issue of JOMS, and three additional reports appeared in the Journal of the American Dental Association in December 2005.9–12 Since the original 2003 publication, more than 1,100 additional reports by over 4,500 authors and at least 14 position papers have been written about what is now accepted as bisphosphonate-induced osteonecrosis of the jaws (BIONJ).
Ironically, the strongest evidence to date of a cause-and-effect relationship between bisphosphonates and osteonecrosis of the jaws is provided by the results of a study Novartis conducted to gain marketing approval by the Food and Drug Administration (FDA). In this study, patients with bone metastasis received either their normal chemotherapy alone or chemotherapy plus a steroid regimen and an intravenous bisphosphonate (either Aredia or Zometa). Patients with the same malignancies but without bone metastasis also received their normal chemotherapy and an identical steroid regimen, but they were not given intravenous bisphosphonates. Interestingly, only those patients who received an intravenous bisphosphonate ever developed exposed bone. This amounted to one of the best randomized, controlled, and truly double-blinded studies in the history of medicine or dentistry.
Flaws in the original study by Novartis are largely the cause of so much disbelief. Their claim that their animal studies failed to show osteonecrosis is likely due to the fact that animal bone physiology is extremely resistant to chemical and physical injury. The profession of oral and maxillofacial surgery has sought to produce a reliable animal model for osteoradionecrosis—its historical nemesis—for four decades. Yet with each attempt, either exposed bone could not be produced or the radiation dose was increased to the point of killing the study animal. In their human clinical trials, Novartis claimed that none of the 3,600+ patients developed exposed bone. This is false; the truth is, they never thought to look for exposed bone in the mouth. Oral examinations before or after intravenous bisphosphonate therapy were never conducted, nor was a dentist or an oral and maxillofacial surgeon...