![]()
1 Patterns of Recovery in Neurologically Impaired Individuals
1.1 INTRODUCTORY REMARKS
In general terms neuropsychologists working in the field of rehabilitation are interested in conditions in which, to some degree, recovery is predicted. It is, of course, quite feasible to use cognitive retraining techniques with patients who suffer from degenerative conditions such as Alzheimer’s disease or multifocal/degenerative states such as multiple sclerosis or multiinfarct dementia. Reality Orientation (Holden & Woods, 1982) is one such example of a cognitive retraining technique which has largely been used with groups of patients suffering from degenerative conditions. However, when dealing with degenerative conditions it is usually necessary to employ a broad psychological approach to treatment and it may turn out that facilitation of adjustment processes for the patient and the carers is the most important role for the clinical neuropsychologist. In addition, in degenerative conditions evaluation is often extremely difficult due to the severity of impairment and alterations of mood state.
It is therefore proposed that the main emphasis of this chapter will be upon conditions such as head injury, stroke and encephalitic illnesses in which continuing deterioration of higher mental functioning is not predicted. The patient population investigated in the Newcastle Cognitive Retraining study was composed of patients suffering severe head injury, stroke or herpes simplex encephalitis, and many of the ideas, particularly the models of rehabilitation which are described fully in later chapters, have been generated with reference to the aforementioned groups of neurologically impaired individuals. Thus, cognitive retraining with groups of patients or individuals suffering from degenerative neurological conditions or less common non-degenerative neurological conditions (e.g. anoxic states, endocrine disorders, or nutritional deficiencies) needs to be the subject of further investigation and is beyond the scope of this volume.
1.2 RECOVERY FROM HEAD INJURY
The degree of spontaneous recovery in head injury varies depending upon the severity of the head injury. Some patients may merely be concussed for a few minutes but others may be in coma for several weeks before signs of a recovery process can be seen. The difference in rate of recovery is associated with severity of the injury. A mild concussive injury leads to temporary disruption of coordinated brain activity but a severe head injury produces coma, structural damage, and a significant degree of brain swelling (cerebral oedema).
There is considerable debate about the mechanism of recovery in head injury. Is it due to a relearning process, whereby the system makes use of preserved neuronal capacity and alternative pathways? Or is it due to restoration and recovery of damaged structures? It is well recognised that elderly patients have reduced neuronal capacity and also recover less well from severe head injury. However, unless some restoration or recovery of the damaged structures occurs, elderly people would presumably show little sign of recovery from a head injury. This would tend to imply that relearning and the establishment of alternative pathways takes place in conjunction with restoration and recovery of damaged structures.
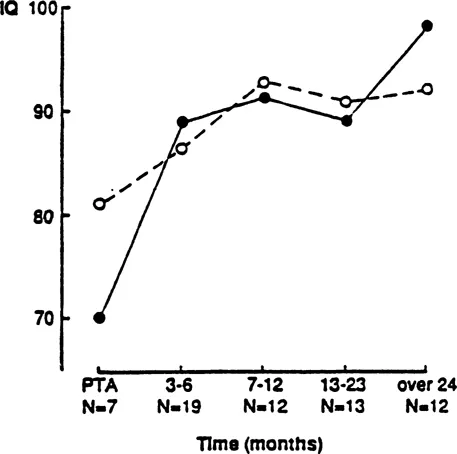
The shape of the recovery curve in severe head injury is determined by a slow, progressive restoration of cerebral function which may or may not lead to the patient functioning at a level equivalent to that enjoyed in their premorbid state. The recovery process has been noted to continue for 10 years after trauma occurs (Thomsen, 1981). However, the majority of recovery tends to occur within the first 6 months after the onset of a severe head injury (Bond & Brooks, 1976). They showed that it was possible to produce recovery curves for specific functions such as verbal or non-verbal intelligence. They used the Mill Hill vocabulary scale and the Raven’s Progressive Matrices to demonstrate this. The recovery curve measured by the scores on the Raven’s Matrices shows a sharp rise during the first 6 months, followed by a period of relative plateau with another sharp rise at the 2-year stage (Fig. 1.1). The scores on the Mill Hill vocabulary test changed less over time and gave rise to a less steep recovery curve but they started at a higher point initially. These curves reflect the differential effect upon verbal and non-verbal functioning of a severe closed head injury. However, some care needs to be exercised in interpreting this figure as it is from a longitudinal study with different numbers of patients at each time interval.
FIG 1.1. Examples of recovery curves in head injury. Changes in verbal and non-verbal intelligence in severely brain-damaged men up to 2 years after injury. —•— Raven’s progressive Matrices —o— Mill Hill Vocabulary Scale (Reproduced from Bond & Brooks, 1976 with permission).
Stages of Recovery
Rosenthal and Bond (1990) suggested that recovery has three stages: (1) neurological recovery; (2) a more general adaptive process; (3) a social process involving the interaction of the injured with those closest to them and any resulting changes of social status.
Changes which occur in the steepness of the recovery curve appeared to be linked to the different stages of the recovery process and from that predictions can be made about final outcome.
Assessing the Changes in Functions
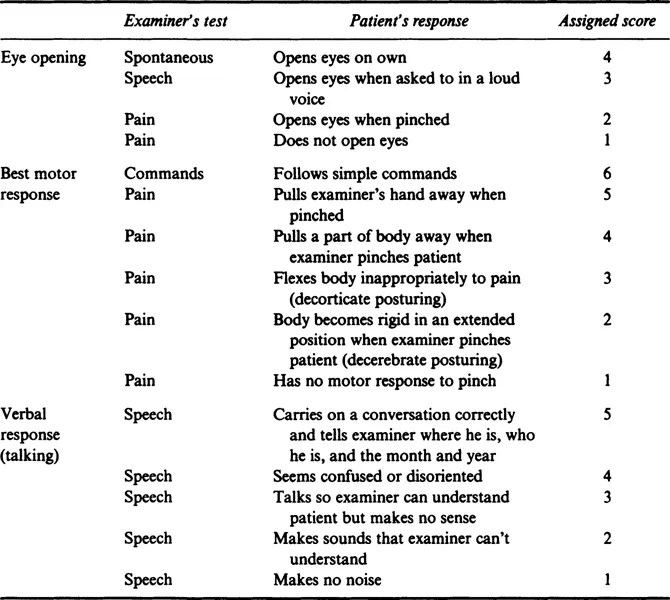
The assessment of changes which occur in the patient’s capacity to function following a closed head injury can be investigated in various ways. One of the best indications of recovery in the early stages is the motor response and early evaluation of the patient status can be ascertained by using the Glasgow Coma Scale (Teasdale & Jennett, 1974). The scale consists of three elements: eye opening, limb movement, and verbal response (see Table 1.1).
TABLE 1.1
Glasgow Coma Scale
Once a patient has passed through the early stages of coma, semiconsciousness, partial confusion, and poor orientation, it is then possible to use a standard neuropsychological assessment in order to measure more subtle changes in behaviour and cognitive functions. In order to investigate the recovery curve, an appropriately sensitive measure of cognitive functioning needs to be used. General intellect, as measured by traditional IQ tests, is not always affected greatly by severe head injury (Newcombe & Fortuny, 1979). However, memory and information processing speed are frequently shown to be impaired, and in order to establish the pattern of natural recovery they should be assessed in some detail.
Memory. It has been pointed out that difficulties arise in serial assessment as it is sometimes not possible to separate out practice effects from actual recovery of functioning. However, Brooks (1987) suggested use of a retested control group design, or a fully cross-sectional design with no control group, or use of a measure not susceptible to practice, or use of alternate forms of test materials and titration of the change against the severity of injury in order to control for practice effects. Conkey (1938), using a multibaseline test-retest design noted that behaviours involving memory seemed to lag behind other behaviours in both rate of recovery and final outcome. In Conkey’s studies, most patients were first assessed when they were still in post-traumatic amnesia but by the second assessment, which was generally about 40 days after the injury, it was possible to note considerable improvement. Recovery of memory functioning has also been reported in studies by Brooks and Aughton (1979) and Bond and Brooks (1976). Patients were assessed at 1, 3,6 and 12 months after the injury. At the 12-months stage the head injured were still significantly worse than controls on word learning. Brooks (1984) suggested using measures of short-term memory or immediate memory span (e.g. digit span) in order to measure recovery. His results suggested marked recovery within 3 years or less of the injury, often up to the normal level. This contrasts with studies of new verbal learning which have shown slow recovery and marked deficits at least one year after the injury and often a failure to reach the premorbid level of functioning.
Language, Disturbances of speech are relatively uncommon after closed head injury, and on balance they appear to recover quite well (Thomsen, 1975). Heilman, Safran, and Geschwind (1971) noted that of the 750 head-injured patients admitted to a Boston Hospital during one year, only 2% were judged to have a residual aphasia. However, others such as Groher (1983) have pointed out that communication is a more complex process involving cognitive processes other than speech, and head injuries do result in impairments of perception, reasoning, judgement, and memory, all of which could affect language processes. Thus in its broadest terms, communication problems might arise in as many as 25% of the severe head injured population (Bond, 1986). It would appear that recovery from aphasia will usually take place within the first six to nine months (Newcombe & Fortuny, 1979). Najenson (1978) demonstrated that visual and auditory comprehension skills tend to return first, followed by expressive abilities and writing. However, whilst the abilities that are normally measured by an aphasia battery (e.g. repetition, word recognition, writing) seemed to recover in a number of months, those language functions which required memory for auditory or written information, abstract reasoning ability or the switching from one topic of conversation to another, still appear to be impaired some two years after the injury (Kertesz & McCabe, 1977).
Perception. A number of studies have reported changes in perceptual functioning following head injury using tests such as Elithorns Mazes, Raven’s Matrices, and Block Design (Roberts, 1979; Smith, 1974). On the whole, it is difficult to find evidence of a distinctive pattern of recovery associated with perceptual functioning. One exception to this might be auditory discrimination functions which consistently appear to show subtle deficits for at least one year following head injury (Bergman, Hirsch, & Nagenson, 1977).
Attention. Studies of attention have presented evidence to suggest that head-injured patients do not suffer from a selective attention deficit and are just as capable of filtering out a distractor as control subjects (Denker & Lofving, 1958; Gronwall & Sampson, 1974). Van Zomeren, Brouwer, and Deelman (1984) did report that head-injured patients have more difficulties than matched controls in dealing with distractions on a number of tasks such as card sorting or mirror drawing. The head-injured subjects were clearly slower in dealing with interference from irrelevant stimulation. Van Zomeren concluded that the difference between head-injured and non-head-injured subjects is in their mental slowness when processing such information, although alertness when attending to a stimulus is also a significant factor but its role has not been researched fully.
Although very little has been written about the recovery of attentional impairments, van Zomeren, Brouwer, & Deelman (1984), in particular, would seem to suggest that distractions can occur which result in subtle dysfunction of cognitive processes, involving decision-making time and response discrimination, which can last up to, and beyond, two years following the head injury.
Recovery of Personality. It is well reported that behavioural disturbance and psychiatric illness can create more disruption to family life and working life than physical problems (Bond, 1975; Oddy, Humphrey, & Uttley 1978).
Levin, Grossman, Rose, and Teasdale (1979) summarised the types of personality problem resulting from head injury as follows:
1. Thinking disturbance with conceptual disorganisation and unusual thought content.
2. Hostility, suspiciousness and uncooperativeness.
3. Withdrawal/retardation. Emotional withdrawal and motor retardation with blunted affect.
4. Anxiety with depression, anxiety with guilt feelings and depression.
Lezak (1978) characterised personality changes in head-injured patients according to five categories of emotional change, impaired social perceptiveness, impaired self-control, increased dependency, and behavioural rigidity. Longitudinal studies relating to behaviour changes following head injury have come from work at Glasgow University from, amongst others, Brooks and McKinlay (e.g. Brooks et al., 1987). They suggested that the most frequently reported changes are slowness, tiredness, irritability, and poor memory. Emotional changes such as poor temper control, irritability, and loss of mood stability are also reported relatively frequently. The Glasgow group found that some personality characteristics such as irritability actually increased in prominence over the first year and by the fifth year 64% of the relatives continued to report irritability as a problem. This research suggested that not only is behavioural disturbance liable to worsen in many cases within the first 12 months after a head injury, but thereafter it may become a permanent disability.
The pattern of recovery in closed head injury is by no means consistent and well defined. It depends upon factors such as age, severity, and site of injury as well as the underlying cognitive function which is being measured. The Coma Scale (Teasdale & Jennett, 1974) or the Outcome Scale (Bond, 1975), which are used regularly in neurosurgical and neurological practice, do not give information of sufficient detail to reflect the subtle cognitive deficits and changes in personality which still seem to be present some two or more years after the insult. If it is possible at all to generalise from the available evidence it could be said that the majority of spontaneous recovery of function in severe head injury occurs with respect to:
1. Confusion in 2 to 3 months.
2. Aphasia in 6 to 9 months.
3. Auditory perceptual discrimination in 12 months.
4. Selective attention, distraction, information processing speed, new verbal learning, verbal and non-verbal recall, abstract reasoning, and conceptual shifting in approximately 2 years.
5. Personality dimensions, such as irritability and lack of drive/initiative, in as many as 5 to 7 years.
1.3 RECOVERY FROM STROKE
In the discussion of rehabilitation from stroke Wade, Langton-Hewer, Skilbeck, and David (1985a) and Wade et al., (1985b) make the useful distinction between adaptive recovery and intrinsic recovery. Adaptive recovery refers to a process of learning to use unaffected areas of functioning in new ways and intrinsic recovery means ...