![]()
Contents
Dedication
Acknowledgment
Foreword
Preface
Chapter 1 Introduction: Probiotics and Psychopathology
Derek Larkin and Colin R Martin
Chapter 2 Probiotics and Chronic Fatigue Syndrome
Derek Larkin and Colin R Martin
Chapter 3 The Gut Microbiota, Health and Exercise
Marie Clare Grant and Julien S Baker
Chapter 4 Impact of Probiotics on Communication between the Brain-Gut: Implications for the Treatment of the Psychological Effects of Digestive Disease States
Melanie G Gareau, Colin Reardon, Kim E Barrett and Philip M Sherman
Chapter 5 Probiotics and their Effect on Maternal and Neonatal Health
Caroline J Hollins Martin and Colin R Martin
Chapter 6 Mechanisms of Action of Probiotics in Psychopathology
Moira S Lewitt
Chapter 7 Probiotics and Eating Disorders
Ursula Philpot
Chapter 8 Probiotics and Obsessive- Compulsive Disorder
Derek Larkin and Colin R Martin
Chapter 9 Probiotics and Depression
Derek Larkin and Colin R Martin
Chapter 10 Probiotics and Alcohol Dependency
Derek Larkin and Colin R Martin
Chapter 11 Probiotics and their Potential Effects on Schizophrenia Symptoms
Mick P Fleming and Colin R Martin
Chapter 12 Probiotics and Alzheimer’s Disease
Derek Larkin and Colin R Martin
Chapter 13 Probiotics and Autistic Spectrum Disorder
Derek Larkin and Colin R Martin
Chapter 14 The Probiotics Evidence-base Improving Quality through Innovation in Research Methodologies
Colin R Martin and Derek Larkin
Index
Editors Biography
![]()
Chapter 1
Introduction:
Probiotics and Psychopathology
Derek Larkin1,* and Colin R Martin2
1 Edge Hill University, St Helens Road, Ormsirk, Lancashire, L39 4QP.
2 Faculty of Society and Health, Buckinghamshire New University, Uxbridge Campus, 106 Oxford Road, Uxbridge, Middlesex, UB8 1NA, UK.
* Corresponding author
Introduction
As you will read throughout the proceeding chapters Probiotics and Psychopathology are fascinating topics in their own right, but when combined they illustrate a complete and intriguing link between our gastrointestinal bacteria and the nervous system.
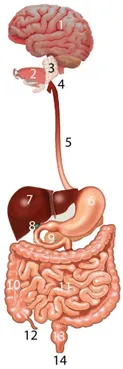
The concept that the gut and brain are intricately linked, and their interactions are to a large extent intuitive, are millennia old and are deeply rooted in our language (Mayer, 2011). Terms such as “heartache” and “gut wrenching” are more than mere metaphor, we feel the ache of love and loss in our chest and abdomen. We experience an orchestral repertoire of emotions in our hearts and stomachs in the form of muscle tightness, or increased heart rate, or abnormal contractions of the stomach— the emotional areas of our brain are inextricably connected to pain regions. The interlink or crosstalk between the gut and brain has revealed a complex bidirectional communication system that appears to help not only maintain gastrointestinal homoeostasis, but is also likely to affect our mental and emotional wellbeing (Emery and Coan, 2010).
The pathway linking the nervous system and the digestive system was first discovered in the nineteenth century and was subsequently labelled the enteric nervous system (Furness, 2008; Furness and Costa, 1987). The enteric nervous system is considered the third branch of the autonomic nervous system, and has been termed the ‘second brain’ (Gershon, 1998; Mayer, 2011). It shares a similar size, complexity, and similarity in neurotransmitter, and signalling molecules with the brain (Gershon, 1998; Mayer, 2011).
The interaction between the brain and the digestive system and their relationship with health and disease has been recognised for many centuries, and studied by ancient cultures, and in modern times by psychologists and physiologists (Mayer and Brunnhuber, 2012). There has been a long-term appreciation that there is an association between several chronic gastrointestinal tract disorders and psychiatric symptoms. While different theories have been proposed, the direction of causality and the precise nature of the underlying pathophysiology remains incomplete (Mayer and Brunnhuber, 2012). Nevertheless, recent scientific advances in the emerging fields of ‘enteric neuroscience’ and ‘emotional neuroscience’ have been instrumental in understanding the bidirectional brain-gut interaction (Mayer, 2011; Mayer and Brunnhuber, 2012). According to Mayer and Brunnhuber (2012) many clinicians continue to adhere to Cartesian dualism when treating patients with chronic gastrointestinal disorders. This idea implies that many gastroenterologists refrain from acknowledging the significant role played by the central nervous system in many disorders, which may include inflammatory bowel disease, or chronic oesophageal disorder. They dismiss psychological and psychiatric factors in the manifestation and maintenance of the disease process as neurotic hysterical behaviours which are only peripheral to the condition. In contrast psychologists and psychiatrics tend to embrace the concept of somatization; the manifestation of psychological distress by the presentation of bodily symptoms (Rhee et al., 2009). There is however still a rudimentary understanding of the involvement of the enteric microbiota including the commensal bacterial flora present within the gastrointestinal tract, which is part of the normal function of the gut. Consequently, the role of the enteric microbiota in the bidirectional gut-brain interaction in relation to general health and disease has received little empirical enquiry (Rhee et al., 2009).
The human digestive system is thought to be home to 400-1000 different species of bacteria, which make up an intricate network of cohabiting organisms (Mazmanian et al., 2008). The enteric microbiota can influence gut homeostasis by the regulation of bowel motility, modulation of intestinal pain, immune response, and nutrient processing (Ait-Belgnaoui et al., 2006; Husebye et al., 2001; Rhee et al., 2005; Rhee et al., 2009). There is a growing school of thought and mounting empirical research that is increasingly examining the symbiotic relationship between the enteric microbiota and their human host. This school of thought is driving afresh, an understanding of the importance of the two systems in maintaining homeostasis health (Turnbaugh et al., 2007).
Tremendous progress has been made in characterizing the bidirectional interactions between the central nervous system, the enteric nervous system, and the gastrointestinal tract. There is growing evidence of the fact that gut microbiota has a powerful influence on gut-brain interactions. There is also growing evidence of gut microbiota influence and development of emotional behaviour as well as stress and pain modulation, and brain neurotransmitter systems (Mayer et al., 2015). Pre- and probiotics have been used to modulate gut microbiota to measure multiple biological systems that may ultimately influence behaviour via the autonomic nervous system, but there is limited information as to how these findings may translate to human health or the disease state, involving the brain or the gut-brain axis. But evidence is mounting which suggests the symbiotic bidirectional brain-gut relationship has other important features that relate to not only our physical well-being but also our psychopathology, outlined in each of the preceding chapters.
Probiotics
The word ‘probiotics’ was derived many thousands of years after it was known that certain food supplements had beneficial effects. The etymology of ‘probiotic’ is derived from the meaning ‘for life’ in Greek, but has had several meanings over the years. Probiotic is in essence described as a substance that is secreted by one microorganism which stimulates the growth of another (Fuller, 2012). However, a more complete definition that was commonly accepted was first used by Parker (1974), organisms and substances which contribute to intestinal microbiota balance. Nevertheless, this definition was thought to have included all microbial substances including ‘antibiotics’ as such Fuller (19...