eBook - ePub
Vulval Dermatologic Diagnosis
Diagnosis by Clinical Presenting Sign
This is a test
- 212 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Vulval Dermatologic Diagnosis
Diagnosis by Clinical Presenting Sign
Book details
Book preview
Table of contents
Citations
About This Book
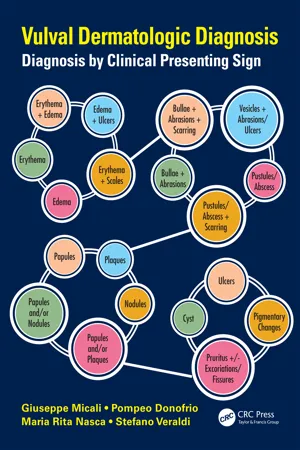
Rather than categorizing vulvar disorders by standard classifications such as neoplastic, inflammatory, or infective, this book describes the disorders by key presenting symptoms-such as erythema, bullae, plaques, cysts, or ulcers. This approach allows clinicians to quickly formulate a correct diagnosis. Vulval Dermatologic Diagnosis: Diagnosis by
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Vulval Dermatologic Diagnosis by Giuseppe Micali, Pompeo Donofrio, Maria Rita Nasca, Stefano Veraldi in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Theory, Practice & Reference. We have over one million books available in our catalogue for you to explore.
Information
1
Anatomy
1.1 General Features
The vulva consists of the mons pubis, labia majora, labia minora, the hymen, the clitoris, the vestibule of the vagina, the urethral orifice, Skene’s glands, Bartholin’s glands, and the vestibular bulbs. The mons pubis, the perineum, and the labia share an ectodermal origin and have a keratinized, stratified, squamous epithelial structure with hair follicles, sebaceous glands, and sweat glands, similar to those of other skin sites. The degree of thickness of the vulvar skin epidermal keratinization progressively decreases from the outer part, the labia majora, to the inner part, the labia minora. The vulvar vestibule, conversely, is nonkeratinized and derived from the endodermal fold.
1.1.1 Mons Pubis
The mons pubis, or mons veneris, is the rounded eminence in front of the pubic symphysis that becomes covered by hair during puberty (A in Figure 1.1). It is characterized by a deep collection of adipose tissue.
1.1.2 Labia Majora
The labia majora are a pair of prominent longitudinal, cutaneous folds of fibro-adipose tissue that are homologous to the scrotum in males (B in Figure 1.1). They form the lateral boundaries of the vulva and are thicker anteriorly, where they join the mons pubis and form the anterior labial commissure (C in Figure 1.1). The posterior ends of the labia and the connecting skin between them form the posterior labial commissure. The labia majora are covered with a varying amount of hair and contain sebaceous, sweat eccrine, and apocrine glands.
1.1.3 Labia Minora
The labia minora are two thin pigmented folds of the vulva composed of a nonkeratinized stratified squamous epithelium (D in Figure 1.1). In a medial position to the labia majora, they are made up of loose connective tissue and blood vessels without any adipose tissue. Anteriorly, the labia minora are split into two parts: one part passes over the clitoris to form the prepuce, while the other joins with the contralateral one under the clitoris and forms the frenulum. Posteriorly, the labia minora blend with the medial surfaces of the labia majora. They are quite small in childhood, grow during puberty, and then become atrophic after menopause. The skin and mucosa are rich in sebaceous glands. Their inner aspect blends into the vulvar vestibule, and the junction of the squamous epithelium and the transitional epithelium forms Hart’s line (black line in Figure 1.1).

FIGURE 1.1 Anatomy of the vulva: (A) mons pubis; (B) labia majora; (C) anterior labial commissure; (D) labia minora; (E) clitoris; (F) vulvar vestibule; (black line) Hart’s line corresponding to the boundary between the keratinized epithelium of the inner surface of the labia minora and the nonkeratinized transitional epithelium of the vulvar vestibule.
1.1.4 Clitoris
The clitoris is the erectile body of the vulva, similar to the corpora cavernosa of the penis. It is located beneath the anterior labial commissure, partially hidden between the anterior segments of the labia minora (E in Figure 1.1). It is composed of a body and a glans. The body consists of two corpora cavernosa covered by their ischiocavernous muscles. The glans is a small mass of erectile tissue that caps the body of the clitoris and is hidden by the prepuce.
1.1.5 Vulvar Vestibule
The vestibule is the cleft located posteriorly to the glans clitoridis and between the labia minora (F in Figure 1.1). It can be visualized by holding the labia minora apart. Hart’s line marks the junction of the nonkeratinized epithelium of the vulvar vestibule and the keratinized epithelium of the inner surface of the labia minora (black line in Figure 1.1). Within the vestibule are the urethral meatus, the opening of Skene’s paraurethral glands, the minor vestibular glands, the Bartholin’s glands duct openings, and the lateral hymenal surface.
1.1.6 Urethral Meatus
The external urethral orifice is 4–6 mm in diameter and is immediately anterior to the vaginal orifice, approximately 2–3 cm beneath the glans clitoridis. The mucosa of the distal third of the urethra is lined by stratified squamous epithelium, whereas the proximal two-thirds are lined by stratified transitional epithelium.
1.1.7 Hymen
The hymen is a thin fold of mucous membrane situated at the entrance to the vagina. The shape of the prepubertal and/or virginal hymen varies, but it is most commonly annular or crescentic. It is very prominent in newborn children, due to maternal estrogens, and it regresses during childhood before the normal pubertal changes. Sexual intercourse and childbirth cause the disappearance of its larger part, leaving only remnants.
1.1.8 Vestibular Glands
The minor vestibular glands are situated around the hymenal ring. Among them, the largest ones are the Bartholin’s glands, deeply located in the musculature.
1.1.9 Neurovascular Supply
The arterial blood supply comes from branches of the external and internal pudendal arteries. Lymph drains from the vulva into the medial group of superficial inguinal nodes on both the ipsilateral and contralateral sides. The sensory nerve system involves the genitofemoral nerve (L1 and L2) and the cutaneous branch of the ilioinguinal nerve (L1) for the anterior vulva, the pudendal nerve for the posterior part of the vulva, and the clitoris and the perineal branch of the posterior cutaneous nerve of the thigh for a small area of the posterior vulva.
Motor innervation of the perineal muscles is enabled by the pudendal nerve.
2
Erythema
2.1 Erythema
2.1.1 Intertrigo
Clinical aspect: Diffuse inguinal reddening and erythema (Figures 2.1.1 and 2.1.2) is a common finding, often more intense at the follicular openings with an overall uniformly “spotted” appearance; edema, oozing, malodorous maceration, and fissuring may ensue in acute stages, whereas lichenification and peripheral postinflammatory hyperpigmentation are typical of longstanding, chronic forms.
Definition: Nonspecific inflammatory eruption of inguinal folds.
Etiology: It can be precipitated by friction, occlusion, sweating, and obesity.
Epidemiology: It is common.
Clinical course: Soreness and itching are common symptoms. Recurrences after therapy are quite frequent in predisposed subjects.
Diagnosis: Clinical diagnosis is usually straightforward. Wood’s light and skin swabs may be helpful for ruling out tinea cruris or erythrasma. A skin biopsy is seldom required in chronic forms to exclude other uncommon conditions, such as Hailey–Hailey disease.
Differential diagnosis: Candidiasis, bacterial infections, eczema (contact, atopic, and seborrheic dermatitis), Hailey–Hailey disease, inverse psoriasis, erythrasma, dermatophytosis, acrodermatitis entheropathica, Darier disease, and extramammary Paget disease.
Therapy: Treatment with a topical barrier and lenitive nongreasy creams and trauma avoidance is usually effective.

FIGURE 2.1.1 Acute intertrigo with prominent erythema of the inguinal folds.

FIGURE 2.1.2 Acute intertrigo of inguinal folds extending to the perineal cleft.
Bibliography
Mistian P, Halm-Walters MV. Prevention and treatment of intertrigo in large skin folds of adults: A systematic review. BMC Nurs 2010;9:12.
Wolf R, Oumeish OY, Parish LC. Intertriginous eruption. Clin Dermatol 2011;29:173–179.
2.1.2 Inverse Psoriasis
Clinical aspect: On the vulva, inverse psoriasis more often appears as sharply demarcated, bright red, nonscaling and glazed patches that may be associated with pronounced vestibular erythema (psoriatic vestibulitis) (Figure 2.1.3). Inverse psoriasis may involve the genitocrural area with confluent, bright red, slightly scaling plaques on the labia majora and the mons pubis, and scattered, well-demarcated erythematous patches on the inner thigh (Figure 2.1.4). Smooth, well-defined erythematous patches involving the inguinal and gluteal folds in the napkin area (napkin psoriasis) as a result of the Koebner’s phenomenon are also common findings in affected children (Figure 2.1.5). Symptoms are highly variable and may range from minimal discomfort to intense itching and/or burning...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Table of Contents
- Editors
- Contributors
- Introduction and Terminology
- 1. Anatomy
- 2. Erythema
- 3. Edema
- 4. Vesicles
- 5. Bullae
- 6. Pustules/Abscess
- 7. Papules
- 8. Plaques
- 9. Nodules
- 10. Cysts
- 11. Ulcers
- 12. Pigmentary Changes
- 13. Pruritus
- 14. Miscellaneous