![]()
1
The exceptional potential of general practice
In a 1953 essay on science and the modern world, the British mathematician and philosopher A. N. Whitehead wrote,
The leading intellects lack balance. They see this set of circumstances, or that set, but not both sets together. The task of coordination is left to those who lack either the force or the character to succeed in some definite career. In short, the specialised functions of the community are performed better and more progressively, but the generalised function lacks vision. The progressiveness in detail only adds to the danger produced by the feebleness of coordination. We are left with no expansion of wisdom and with greater need for it. (1)
The thesis of this book is that generalism, far from being what’s left for those ‘lacking either the force or the character to succeed in some definite career’, is a very definite career whose time has come but whose exceptional potential is still being realised.
CONSULTATIONS between practitioners and patients who are ill, distressed or who think they are ill are the cornerstone of practice, providing the starting points and turning points of care and involving decisions about the diagnosis and management of diseases from which almost everything else flows.
In 1979, Stott and Davis wrote a seminal paper entitled ‘The exceptional potential in each primary care consultation’, highlighting four components: the management of presenting problems, modification of help-seeking behaviour, management of continuing problems and opportunistic health promotion (2).
Consultations are the building blocks of care, but what needs to be built is a strong and comprehensive health care system. The challenge for clinical generalists is to show that general practices working together are a cost-effective way of improving population health and well-being, reducing fragmentation of care, stemming overuse of emergency services and reducing health inequalities.
The exceptional potential of general practice depends not only on consultations, but also on many other components of care.
CARING involves not only tuning in to patients’ ideas, concerns and expectations, but also being ambitious for their health and health care. As Dr Francis Peabody once said, ‘The secret of the care of the patient is in caring for the patient’ (3). The ‘unworried unwell’, in particular, need a doctor who can use his or her greater knowledge and experience to anticipate and avoid problems. When a patient’s health literacy, confidence and agency are low, self-help and self-management are destinations rather than starting points.
CONTINUITY of care via serial encounters helps to build the shared knowledge and confidence that lead to better outcomes. Julian Tudor Hart described his long-term relationship with a patient as ‘initially face to face, eventually side by side’ (4). For patients with complex problems and situations, seeing a familiar face avoids the time-consuming task of retelling their story to someone new. For practitioners, previous knowledge of and experience with patients means that more can be achieved within short consultations.
COORDINATION or orchestration of care involves bringing all relevant contacts, services and resources into play, with follow-up to assess the outcome.
Population COVERAGE requires universal access to care, a defined patient denominator, information systems that allow the measurement of omission and systematic measures to ensure high coverage rates.
Building CAPACITY requires adequate numbers of staff within the practice team, efficient deployment of their skills and strong working links with other services and resources, including embedded workers whenever possible.
COMMUNITY engagement involves establishing links with resources for health and health care in the community, including the third sector and voluntary groups. Link workers embedded within practices have been adept at developing this role.
CREATIVITY involves a constant search for better ways of doing things. Most local systems develop not from a blueprint or logic plan, but rather by trial and error, pursuing the positive and eliminating the negative.
COMMITMENT to the patients, practice and local community over a period of time provides the continuity and drive needed to overcome obstacles and achieve change.
CONSISTENCY implies that patients receive a similar standard of care wherever they access a general practice.
COLLEGIALITY involves common purpose, collective responsibility and the sharing of experience, views, information, evidence, activity and values so that the best anywhere becomes the standard everywhere.
CAMPAIGNING involves persistent advocacy with clear messages, examples and evidence of how health and health care can be improved.
REFERENCES
1. Whitehead AN. Science and the Modern World. Cambridge, UK: Cambridge University Press, 1953.
2. Stott NCH, Davis RH. The exceptional potential in each primary care consultation. Journal of the Royal College of General Practitioners 1979;29:201–205.
3. Peabody F. The care of the patient. JAMA 1927;88:877–882. doi:10.1001/jama.1927.02680380001001.
4. Hart JT. A New Kind of Doctor. London, UK: Merlin Press, 1988, 187.
Die when I may, I want it said of me
that I always plucked a thistle and planted a flower
where I thought a flower might grow.
Abraham Lincoln
![]()
2
Three horizons of general practice
ANDREW LYON
The twenty-first century finds us living through a period of change in our daily lives and the precepts by which we live. Such periods generally come along every 250 years or so.
Everything, including general practice, is affected by these changes. In the space of a relatively few years, the ideas that guide our efforts, the actions in which we are engaged, our view of the world, our health and our well-being – and all that goes with it – change beyond recognition. How are we to navigate these changes? The old is dying and the new cannot yet be born, causing morbid symptoms of system failure. How can we simultaneously be hospice workers for the dying regime and midwives for the new?” We are deep into the period of diminishing returns in almost all walks of life. Institutions and those who inhabit them are under almost unbearable pressure, and inertia in systems is a challenge in shifting to more sustainable policies and practices. Currently, three unhelpful ‘isms’ dominate (1):
Economism: Economy and profit are paramount.
Materialism: An excessive pursuit of fulfilment through material goods.
Individualism: Over-elevation of the individual as a primary unit of social organisation.
The pursuit of these ‘isms’ is widely embedded in global systems. Significant effort is engaged in identifying the extent of failure in essential systems – climate, food, water, energy, ecological diversity, and so on. There is much talk but insufficient action at the global or even national scale so far. We must learn to do something different.
In this short piece, I want to use the three horizons framework as developed by the International Futures Forum (2) to explore these questions based on my experience as the chair of GPs at the Deep End until 2016 (Section 6.1).
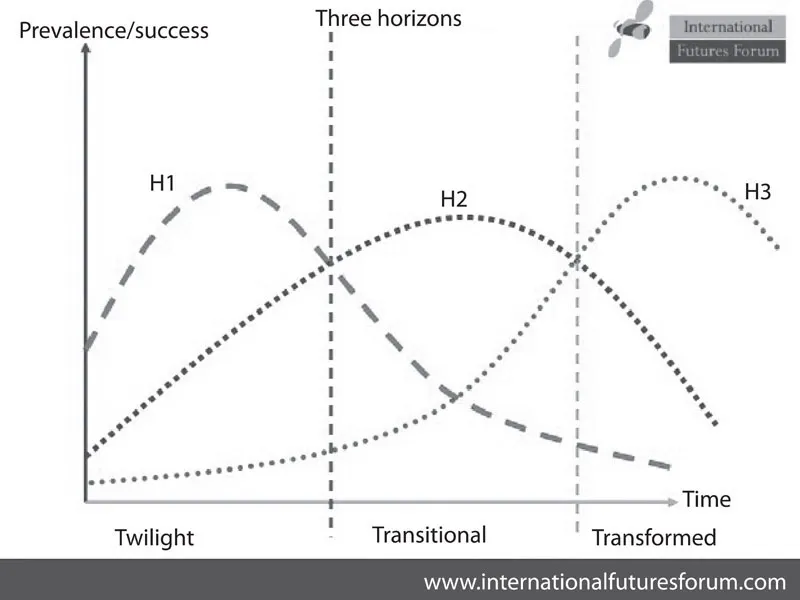
First Horizon: The first horizon (H1 in the chart below), is the here and now. In this horizon, the effort is concentrated upon addressing today’s issues with today’s best ideas and practices. Identifying, understanding, disseminating and improving current approaches are examples of such work.
Second Horizon: In the second, more medium term, horizon (H2), our current way of addressing challenges begins to feel less effective and no longer fit for purpose. Innovative approaches emerge, which hold the promise of more effective action. In H2, research and development functions and training help to realise the full power of new understanding for policy and action and have a key role to play alongside transitional actions, which begin to move us from existing to new frameworks.
Third Horizon: Simultaneously, in the third horizon (H3), innovations are taking place which often look fanciful to those working in the first horizon. It is from this horizon, based on fundamentally different premises, that radical innovation and completely new ways of doing things will emerge. Working in this horizon is more about the exploration of predicament, challenge, new thinking and different perspectives that keep possibilities for the future open.
Each horizon is present and relevant in every time frame Figure 2.1. It is the relationship between the perspectives which changes over time. The three horizons provide a framework not only for understanding but also for action and cooperation between perspectives that is relevant for action today and keeps options open for the future, which otherwise might be missing as new challenges emerge.
In general, a third horizon needs to be based on the principles different from the ‘isms’ outlined above, which means we are heading for system disruption.
Figure 2.1 Three horizons (2).
GPs at the Deep End express their desired future – their third horizon – very clearly: a community-led general practice making a significant contribution to healthier, longer and fulfilling lives for those living at the Deep End.
Three kinds of actions might be taken now to move towards a more desirable future.
1. Action needed to address shortcomings in the system as it exists currently.
2. Actions that can be taken to bridge the gap between the current situation and that we want, including what we want to give up.
3. Actions, at small scale to begin with, which resonate with the future we want.
In taking action, ask:
• What can I do by myself as an individual GP?
• What can my practice do?
• What can the profession do?
• What must the professional work with others to do?
The future does not already exist. It is a place we are making and the making of it has the potential to change...