1
The Use of Ovarian Markers
Neena Malhotra and Siladitya Bhattacharya
Introduction
Ovarian reserve is a term used to describe a woman’s reproductive potential and is a reflection of her pool of primordial follicles or, more specifically, the number and quality of oocytes in her ovaries (1). Each woman is born with approximately 2 million primordial follicles, but this number drops to 400,000 around menarche as a consequence of follicular atresia (2). Follicle numbers fall further with age, and the rate of decline is faster when women are in their mid-30s. This decline in fertility potential is specific for an individual woman and is influenced by race as well as genetic and environmental factors.
The ideal ovarian reserve test should be convenient, reproducible, display little if any intracycle and intercycle variability, and demonstrate high specificity to minimize the risk of false diagnoses. At the same time, the test should be able to identify women with an abundance of ovarian reserve and those who are likely to respond vigorously to ovarian stimulation in the context of fertility treatment. A number of biomarkers have been used over the last few decades to predict ovarian response and pregnancy outcomes, including live birth in women undergoing in vitro fertilization (IVF). These include hormonal assessments and ultrasound parameters.
Hormonal biomarkers include serum early follicular (basal) levels of follicle-stimulating hormone (FSH), estradiol (E2), inhibin B, and anti-Müllerian hormone (AMH), as well as dynamic tests that measure gonadotropins and estradiol levels in response to stimulation, like the clomiphene citrate challenge test (CCCT), GnRH-agonist stimulation test (GAST), or exogenous FSH ovarian reserve test (EFORT).
Ultrasonographic assessments include antral follicle count (AFC) and ovarian volume. The number of antral follicles reflects the size of the remaining follicular pool and correlates with the number of oocytes retrieved following stimulation. Ovarian volume declines with advancing age and is a potential indicator of ovarian reserve.
This chapter considers the basic principles governing the use of diagnostic tests and reviews common tests of ovarian reserve including their role in predicting fertility with and without assisted reproduction treatment.
Understanding Diagnostic Tests
As diagnostic tests are seldom 100% accurate, tests need to be validated by comparing them with an ideal test or a gold standard in a suitable population of patients. A valid test is able to identify most people with a particular condition and exclude most people without that condition such that a positive test result means that the disorder in question is present (3). Conventionally, four terms are used to qualify the validity of a test—sensitivity, specificity, positive predictive value, and negative predictive value (Figure 1.1). Sensitivity is the true positive rate that expresses how good the test is for correctly identifying those with the condition. In contrast, specificity is the true negative rate that tells us how good a test is for correctly excluding people without the condition.
Figure 1.1 Calculation of test validity. (With permission from Grimes D, Schulz K. Lancet. 2002;359[9309]:881–4.)
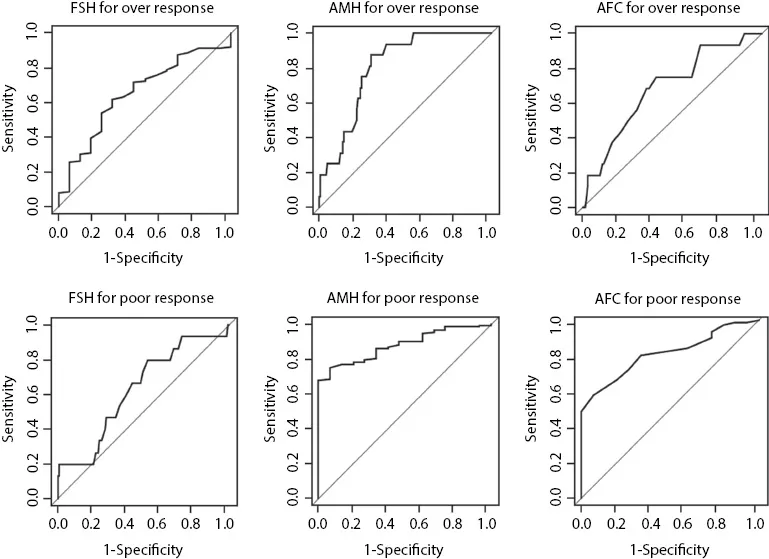
As both sensitivity and specificity represent a retrospective analysis of results that have already been collected, their clinical use is limited. In real life, clinicians need to know the predictive value of the test, i.e., whether a patient who tests positive actually has the disease or condition in question. Positive predictive value is the posttest probability of a positive test. It tells the clinician what the probability of having that condition is if the patient tests positive. Negative predictive value tells the clinician the probability of a patient not having a condition if the patient tests negative. It is customary to express the validity of the test by plotting sensitivity against one minus specificity and measure the area under the curve (AUC). AUC is an effective way to summarize the overall diagnostic accuracy of the test by plotting values between 0 and 1 (Figure 1.2), where a value of 0 indicates a totally inaccurate test and a value of 1 a perfectly accurate test. An AUC of 0.5 indicates an inability to diagnose patients with and without a particular condition, while 0.8–1.0 is considered excellent (6).
Figure 1.2 Receiver operating characteristic curves and area under the curve for a number of common ovarian reserve tests. (With permission from Nardo L et al. Fertil Steril. 2009;92[5]:1586–93.)
The prevalence of disease in a population affects the performance of screening tests. Even excellent tests have poor predictive value positives in low-prevalence settings. For example, a valid test of ovarian reserve will have a better positive predictive value in women attending a fertility clinic than in a general population of asymptomatic women. Hence, knowledge of the approximate prevalence of disease is a prerequisite to interpreting screening test results. Inappropriate application or interpretation of screening tests can rob people of their perceived health, initiate harmful diagnostic testing, and squander health-care resources. From a clinical perspective, key questions about tests include the following: Is it relevant, i.e., can the test be used in the relevant patient group? Is it affordable, acceptable, and better than the test normally used? And crucially, Will it inform the choice of treatment?
Early Follicular Follicle-Stimulating Hormone
Levels of basal FSH in the early follicular phase have been used as a biomarker for the prediction of response to ovarian stimulation during in vitro fertilization (IVF) (7,8). The test is based on the feedback inhibition of FSH pituitary secretion by ovarian hormones. Women with normal ovarian activity should produce sufficient levels of ovarian hormones at this early stage of the menstrual cycle to suppress FSH levels within a normal range. Elevated serum FSH levels suggest poor production of ovarian estrogen by a smaller follicular pool consistent with diminished ovarian reserve (DOR). However, basal FSH testing has several major limitations, including significant intercycle and intracycle variability (9,10) and limited sensitivity when used in isolation. Measurement of both FSH and estradiol on cycle day 3 may therefore help decrease the incidence of false-negative testing. Despite its limitations, FSH is commonly used as an ovarian reserve test, and high values have been associated with both poor ovarian response and failure to achieve pregnancy (11). FSH has relatively high specificity (45%–100%) for poor response to ovarian stimulation (usually defined as less than four retrieved oocytes) using cutoff points beyond 10 IU/L (10–20 IU/L), but its sensitivity is generally poor (11%–86%) (11,12). In terms of predicting lack of conception, FSH testing is still specific (50%–100%) but much less sensitive (3%–65%) using similar cutoffs (11,12). This test is still clinically useful since an abnormally ele...