![]()
Section 1
Non-cardiac chest pain and biopsychosocial approaches
![]()
Introduction
Why is this book needed?
Chest pain is common. It is usually distressing because of its association with heart disease, and it can become chronic if untreated (Marks et al., 2014). However, chest pain is most frequently benign. Non-cardiac causes are approximately four times more common than coronary disease or other dangerous conditions. Understandably, because missing coronary disease can lead to myocardial infarction or death, the main focus is on detecting coronary disease. There are detailed protocols to enable health professionals to do this that were drawn up by professional bodies, including the European Cardiac Society and the American Heart Association (Gibbons et al., 2007; Montalescot et al., 2013).
Once coronary disease has been excluded, the modern medical management process typically runs out of momentum. There are no international guidelines to manage non-cardiac chest pain (NCCP). Patients with NCCP generally remain unassured by negative cardiac investigations and have a high level of pain and psychological distress (Chambers et al., 2013; Marks et al., 2014), high unemployment rates and heavy use of health-care resources (Eslick and Talley, 2004; Fagring et al., 2010; Christoph et al., 2014). The causation and maintenance of NCCP may be complex given the interaction of organic and psychological processes. However, treatment can be effectively delivered at a relatively low cost. In this book, we aim to describe a biopsychosocial approach that can be used to understand NCCP and help patients manage it.
A biopsychosocial approach
Health emerges from an interactive network of biological, psychological and social factors. The cause and maintenance of NCCP often involves a complex interaction of organic and psychological processes (Chambers et al., 2013). To fully understand each individual with NCCP, all of these factors must be considered. This requires a full medical assessment to identify any organic factors and a thorough psychosocial assessment to identify the cognitive, emotional, behavioural and social influences on pain. An alternative biopsychosocial explanation can then be developed with an individualized treatment plan. This may include an effective medical or physical treatment, as well as specific psychological management strategies.
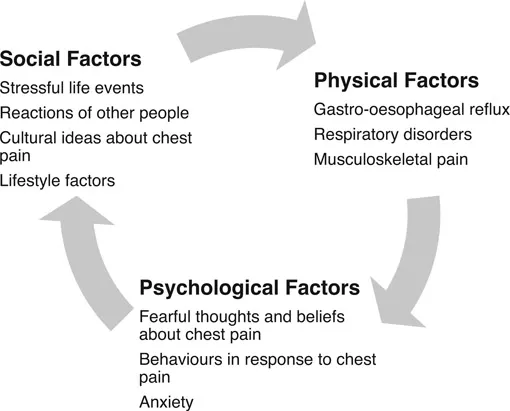
Once heart disease has been excluded, it is possible to identify alternative physical causes (such as gastro-oesophageal reflux or musculoskeletal disorder). There may be psychological factors influencing NCCP (such as anxiety, behavioural changes and fearful beliefs about the meaning of chest pain) and important social and lifestyle factors (such as stressful life events and the responses of other people, including health-care professionals). These factors can influence and exacerbate chest pain in a vicious cycle (see Figure I.1), which explains how and why NCCP persists. We explore these various factors in more detail in Chapter 4.
This book offers an overview of the epidemiology of NCCP, followed by an explanation of how to assess patients with NCCP. It then offers a treatment strategy based on cognitive behavioural therapy (CBT) that identifies potential solutions and effective coping strategies for NCCP. CBT has been identified as the most effective and reliable treatment for NCCP in recent Cochrane Reviews (Kisely et al., 2010; 2012). Studies have found that an important part of successful treatment is an initial, comprehensive and therapeutic assessment. This involves investigation of the multiple factors affecting chest pain followed by unambiguous reassurance and written information (Mayou et al., 1999). Of those patients who remain distressed, many can benefit from further support using ‘low-intensity’ CBT delivered in the format of guided self-help, whilst others may require a ‘high-intensity’ CBT intervention in the context of extreme distress or complicating factors (Chambers et al., 2014).
Figure I.1 The biopsychosocial model of chest pain indicating the types of biological, psychological and social factors that may be important in NCCP.
This book is based on our biopsychosocial chest pain clinic run by a cardiologist, cardiac nurses and psychologists. It has been found to lead to significant benefits for many people with persistent chest pain (Chambers et al., 2014; Marks et al., 2016). The clinic team developed this book as an evidence-based guide based on their experiences and knowledge of working with chest pain. It can be used by a range of health-care professionals working with people who have NCCP, such as cardiologists, nurses, psychologists, CBT therapists, psychological well-being practitioners and general practitioners.
Chapter 1 begins by offering an overview of NCCP and its prevalence, prognosis and impact on people’s quality of life. In Chapter 2, we describe how to differentiate NCCP from chest pain caused by cardiac disease. It is important that coronary artery disease is excluded before you and the person with chest pain feel confident in engaging in this treatment approach. Chapter 3 offers an overview of the historical and sociocultural perspectives of chest pain and how these shape a person’s reactions to NCCP. In Chapter 4, we look at biopsychosocial approaches to pain in general, and in Chapter 5 we look at the biological and psychosocial factors specific to NCCP. Chapter 6 provides an overview of CBT and how this is used within a biopsychosocial approach to NCCP. In Chapter 7 we draw this information together in a way that will support the clinician in conducting comprehensive, therapeutic assessments. This includes a structured assessment protocol.
The second part of the book is a workbook that guides treatment. It gives detailed information to allow the treating clinician to provide guided self-help (sometimes known as low-intensity CBT) to patients with persistent NCCP. This workbook does not train the clinician to become a CBT practitioner and does not qualify them to deliver standard (or high intensity) CBT. Rather, as seen in other forms of ‘low intensity’ CBT, it offers a standardized intervention grounded in CBT principles that includes a variety of strategies known to be helpful in NCCP. It is appropriate for delivery by a clinician who has had some training in CBT preferably closely supervised by a CBT practitioner. For example, delivery by a cardiac nurse who has completed a short training in the basics of CBT and who with their CBT supervisor regularly. The treating clinician should follow the workbook closely, session by session, taking any issues not covered by the manual to the supervising CBT specialist. The workbook includes handouts and audio resources for the patient, and all of these are available in the appendices or can be downloaded at www.routledge.com/9781138119017. In the third part of the book, there is a list of other resources that may support the clinician in this work and which may also be of use to patients.
All of the information in this book is based on our biopsychosocial chest pain clinic, which has already helped many people struggling with NCCP. We hope that the ideas and strategies suggested in the book will offer similar support and help to other people who continue to struggle with this chronic and disabling condition and to the clinicians working with them.
References
Chambers, J.B., Marks, E.M., Knisley, L., & Hunter, M. (2013). Non-cardiac chest pain: Time to extend the rapid access chest pain clinic? Int J Clin Pract 67: 303–6.
Chambers, J.B., Marks, E.M., Russell, V., & Hunter, M.S. (2014). A multi-disciplinary, biopsychosocial treatment for non-cardiac chest pain. Int J Clin Practice 69(9): 922–7. doi:10.1111/ijcp.12533
Christoph, M., Christoph, A., Dannemmann, S., Poitz, D., Pfluecke, C., Strasser, R.H., Wunderlich, C., Koellner, V., & Ibrahim, K. (2014). Mental symptoms in patients with cardiac symptoms and normal coronary arteries. Openheart 1: e000093. doi:10.1136/openrt-2014-000093.
Eslick, G.D., & Talley, N.J. (2004). Non-cardiac chest pain: Predictors of health care seeking, the types of health care professional consulted, work absenteeism and interruption of daily activities. Aliment Pharmacol Ther 20: 909–15.
Fagring, A.J., Lappas, G., Kjellgren, K.I., Welin, C., Manhem, K., & Rosen-gren, A. (2010). Twenty-year trends in incidence and 1-year mortality in Swedish patients hospitalised with non-AMI chest pain. Data from 1987–2006 from the Swedish hospital and death registries. Heart 96: 1043–9.
Gibbons, R.J., Abrams, J., & Chatterjee, K. et al. (2007). Chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. Circulation 116: 2762–72.
Kisley, S.R., Campbell, L.A., Yelland, M.J., & Paydar, A. (2012). Psychological interventions for symptomatic management of non-specific chest pain in patients with normal coronary anatomy. Cochrane Database Systematic Review 13(6).
Marks, E.M., Chambers, J.B., Russell, V., & Hunter, M.S. (2014). The rapid access chest pain clinic: Unmet distress and disability. Q J Med 107(6): 429–34.
Marks, E.M., Chambers, J.B., Russell, V., & Hunter, M.S. (2016). A novel cognitive behavioural stepped-care intervention for patients with non-cardiac chest pain. Health Psychol Behav Med 4(1): 15–28.
Mayou, R.A., Bass, C.M., & Bryant, B.M. (1999). Management of non-cardiac chest pain: From research to clinical practice. Heart 81(4): 387–92.
Montalescot, G., Sechtem, U., Achenbach, S., Andreotti, F., Arden, C., Budaj, A., Bugiardini, R., Crea, F., Cuisset, T., Di Mario, C., & Ferreira, J.R. (2013). ESC guidelines on the management of stable coronary artery disease: The task force on the management of stable coronary artery disease of the European Society of Cardiology. Europ Heart J 34: 2949–3003.
![]()
Chapter 1
What is non-cardiac chest pain?
Chest pain is an almost universal experience. Most people have experienced chest pain at times without being concerned by it. However, people seek advice for a variety of reasons, such as if they have severe or recurrent pain, a family history of coronary disease, anxiety about health in general or concerns as a result of health-care advertisements or public health campaigns (Figure 1.1). The prime reason for help-seeking tends to be an understandable concern, or i...