Dermatoscopy in Clinical Practice
Beyond Pigmented Lesions
- 208 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
About This Book
Dermatoscopy has been heavily promoted to dermatologists as the front line in detecting skin cancer early and easily. However, this technology also has other uses in everyday dermatologic practice.
Dermatoscopy in Clinical Practice shows those already using the equipment how they can extend its use beyond pigmented lesions and exploit its full potential. Dermatoscopy and videodermatoscopy can be used for differential diagnosis, prognostic evaluation, and monitoring response to treatment of various disorders including inflammatory diseases, parasitoses, viral and fungal infections, nonpigmented skin lesions, hair abnormalities, and a large variety of other dermatologic conditions as well as cosmetology.
The book focuses on those conditions in which the techniques are most useful, describing the clinical and histopathological correlations associated with the procedure. The book includes color clinical images throughout, making it a handy guide for the dermatologist's daily practice.
Frequently asked questions
Information
1 Equipment for dermatoscopy/videodermatoscopy
DERMATOSCOPY
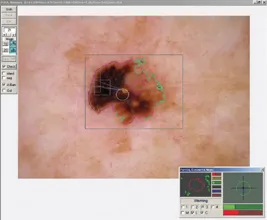
VIDEODERMATOSCOPY
ANALOG VIDEODERMATOSCOPY
DIGITAL VIDEODERMATOSCOPY

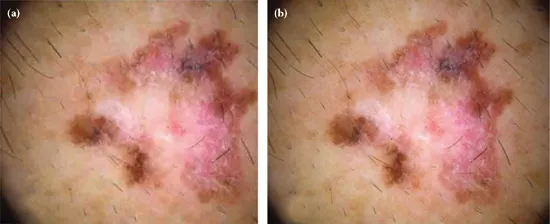
CONTACT, NONCONTACT, AND POLARIZED DERMATOSCOPY
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Table of Contents
- Introduction
- List of contributors
- 1 Equipment for dermatoscopy/videodermatoscopy
- 2 Parasitoses: Scabies
- 3 Parasitoses: Pediculosis
- 4 Parasitoses: Therapeutic monitoring of scabies and pediculosis
- 5 Parasitoses: Tungiasis
- Parasitoses: Cutaneous larva migrans
- 7 Parasitoses: Cutaneous leishmaniasis
- 8 Parasitoses: Trombiculiasis
- 9 Infectious diseases: Cutaneous and genital warts
- 10 Infectious diseases: Molluscum contagiosum
- 11 Infectious diseases: Tinea capitis
- 12 Hair loss and hair shaft disorders
- 13 Inflammatory diseases: Psoriasis
- 14 Inflammatory diseases: Lichen planus
- 15 Inflammatory diseases: Common urticaria and urticarial vasculitis
- 16 Inflammatory diseases: Connective tissue diseases
- 17 Inflammatory diseases: Rosacea
- 18 Inflammatory diseases: Pigmented purpuric dermatoses
- 19 Inflammatory diseases: Pityriasis lichenoides
- 20 Inflammatory diseases: Granulomatous skin disorders and Wolf’s isotopic response lesions
- 21 Nonpigmented skin lesions: Clear cell acanthoma
- 22 Nonpigmented skin lesions: Pyogenic granuloma
- 23 Nonpigmented skin lesions: Angiokeratoma
- 24 Nonpigmented skin lesions: Sebaceous hyperplasia
- 25 Nonpigmented skin lesions: Xanthomatous lesions
- 26 Nonpigmented skin lesions: Porokeratosis
- 27 Nonpigmented skin lesions: Apocrine hidrocystoma
- 28 Nonpigmented skin lesions: Bowen’s disease
- 29 Nonpigmented skin lesions: Actinic keratosis and squamous cell carcinoma
- 30 Capillary malformations
- 31 Miscellaneous disorders
- 32 Photodamaged and aged skin
- Index