- 104 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
About this book
Five percent of all accident and emergency admissions are caused by prescribed medicines. This figure rises to an alarming twelve percent in elderly patients. This may be through inappropriate use or dosage, side effects, drug: drug interactions, failing metabolism in the liver and reduced excretion by the kidneys. Also, erratic compliance with drug taking by a large proportion of patients complicates and sometimes worsens iatrogenic harm. This practical guide details the most common errors made in prescribing and is ideal for day-to-day use. The clear, accessible language used throughout makes for quick and easy reference. It clarifies complex scientific issues and presents them in a practical format, indispensable for professional life. It is highly recommended for all prescribers, clinical pharmacists, medical students and Foundation Year doctors. It is also a vital resource in the medication review now required for the Quality and Outcomes Framework for General Practitioners in England.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
1
Treatment failure due to antacids
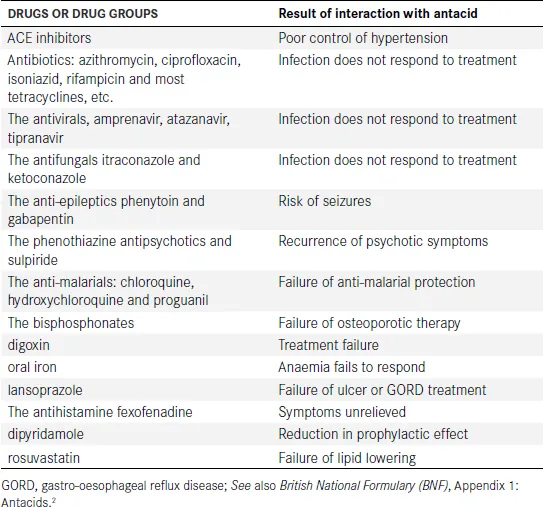
- formation of a chemical complex – complexation
- adsorption of the drug by the antacid
- resin binding
- destruction of a drug’s acid-resistant coating due to the increased pH in the stomach that results from the antacid.
- 1 Is it due to non-compliance?
- 2 Is it due to an antacid?
References
2
Grapefruit juice can cause drug toxicity
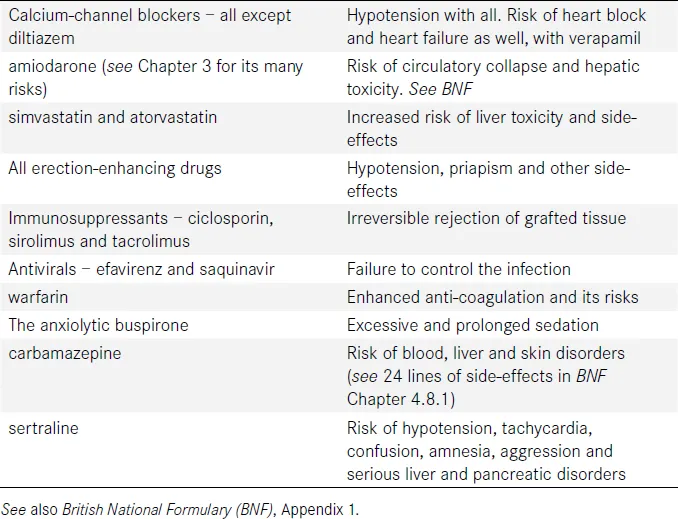
Tactics to Avoid the Risk of Excessive Drug Absorption
- The Easy Way Out (EWO)! The simplest way of avoiding the risks of grapefruit juice is to tell all patients taking short-term or maintenance medication to avoid it. This is no great hardship, and a ‘blunderbuss’ approach makes life a little easier for the prescriber and the dispenser.
- A more subtle tactic. Use your prescribing software to ‘flag up’ a warning message on the counterfoil of the prescription form, whenever one of the drugs listed in Table 2.1 is prescribed. This should always be accompanied by a strong verbal warning, since many patients don’t read counterfoil instructions, let alone those on the patient information leaflet (package insert).Have no illusions – grapefruit juice is a major prescribing pitfall, especially in older patients and those with reduced kidney or liver function.For the curious, the culprit in grapefruit juice has been identified as a furanocoumarol, also found in bitter oranges. This blocks the intestinal P450 enzyme irreversibly. However, the intestinal mucosa generates a fresh population of enzyme, usually within 24 hours.
A footnote: cranberry juice
INTRODUCTION TO CHAPTERS 3, 4 AND 5: THREE EFFECTIVE AND DANGEROUS DRUGS
3
Warfarin
Table of contents
- Cover Page
- Halftitle Page
- Title Page
- Copyright Page
- Dedication
- Contents
- Introduction
- 1 Treatment failure due to antacids
- 2 Grapefruit juice can cause drug toxicity
- 3 Warfarin
- 4 Amiodarone: a candidate for the title ‘riskiest drug’
- 5 The non-steroidal anti-inflammatory drugs (NSAIDs), including the ‘COXIB’ NSAIDs
- 6 Drugs that disrupt the fine equilibrium of renal function
- 7 Sudden cardiac collapse due to often-prescribed drugs causing QTc prolongation
- 8 Some important interactions between drugs at shared sites of action and/or therapeutic effect
- 9 Major prescribing pitfalls due to drug–drug interactions in the liver
- 10 Two serious prescribing pitfalls caused by alcohol use (and abuse)
- 11 Monitoring the effects of drug treatment to avoid pitfalls. Which drugs? Which tests? How often?
- 12 Serious lung diseases caused by prescribed drugs
- 13 Preventable prescription-related illness caused by patient non-compliance
- 14 The scientific basis of prescribing for the elderly
- 15 Clinical quizzes: practical examples from Chapters 1–13
- 16 Answers to clinical quizzes
- Index
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app