eBook - ePub
Introduction to Telemedicine, second edition
This is a test
- 226 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Introduction to Telemedicine, second edition
Book details
Book preview
Table of contents
Citations
About This Book
In rural and sparsely populated countries, telemedicine can be a vital and life-saving link to health care, and in those regions where demands on hospitals are ever increasing, it can provide a safe and comfortable alternative to hospital-based therapy. The second edition of this introductory guide to telemedicine and telecare services is invaluable to new practitioners in this growing field of medicine. The book describes the benefits of telemedicine and highlights the potential problems. The authors provide numerous examples of how telemedicine is used in the United States, Australia, and Scandinavia.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Introduction to Telemedicine, second edition by Richard Wootton, John Craig, Victor Patterson in PDF and/or ePUB format, as well as other popular books in Medicine & Public Health, Administration & Care. We have over one million books available in our catalogue for you to explore.
Information
Section 1: Background
1. Introduction to the practice of telemedicine
John Craig and Victor Patterson
2. Telemedicine systems and telecommunications
Brett Harnett
▸ 1
Introduction to the practice of telemedicine
John Craig and Victor Patterson
Introduction
One of the great challenges facing humankind in the 21st century is to make high-quality health care available to all. Such a vision has been expressed by the World Health Organization (WHO) in its health-for-all strategy in the 21st century.1 Realizing this vision will be difficult, perhaps impossible, because of the burdens imposed on a growing world population by old and new diseases, rising expectations for health, and socioeconomic conditions that have, if anything, increased disparities in health status between and within countries.
Traditionally, part of the difficulty in achieving equitable access to health care has been that the provider and the recipient must be present in the same place and at the same time. Recent advances in information and communication technologies, however, have created unprecedented opportunities for overcoming this by increasing the number of ways that health care can be delivered. This applies both to developing countries with weak or unstable economies and to industrialized countries. The possibilities for using information and communication technologies to improve health-care delivery (‘health telematics’) are increasingly being recognized. The WHO has stated that with regard to its health-for-all strategy it recommends that the WHO and its member states should:
...integrate the appropriate use of health telematics in the overall policy and strategy for the attainment of health for all in the 21st century, thus fulfilling the vision of a world in which the benefits of science, technology and public health development are made equitably available to all people everywhere.2
Such a commitment to improve health-care delivery, by utilizing information and telecommunications technologies, is also being considered by those with the financial means to do so, for example, the participants in various European Commission projects. At the national and subnational level, there is also evidence of governmental interest in the benefits that these technologies might bring to health care. For example, in the UK, information technology including telemedicine is at the heart of the government’s strategy to modernize and improve the NHS.3 Telemedicine, the area where medicine and information and telecommunications technology meet, is probably the part of this revolution that could have the greatest impact on health-care delivery.
What is telemedicine?
Telemedicine is the delivery of health care and the exchange of health-care information across distances. The prefix ‘tele’ derives from the Greek for ‘at a distance’; hence, more simply, telemedicine is medicine at a distance. As such, it encompasses the whole range of medical activities including diagnosis, treatment and prevention of disease, continuing education of health-care providers and consumers, and research and evaluation.
Telecare is a related term and refers to the provision, at a distance, of nursing and community support to a patient. Similarly, telehealth refers to public health services delivered at a distance, to people who are not necessarily unwell, but who wish to remain well and independent. In effect, however, despite repeated discussions about what constitutes telemedicine, telecare and telehealth and what their differences are, all involve the transfer of information about health-related issues between one or more sites, so that the health of individuals and their communities can be advanced. In other words, the information is moved, not the providers or the recipients of health care. Nowadays, the transfer of information is generally facilitated by the use of some kind of telecommunications network. An umbrella term encompassing all health-related activities carried out over a distance by such information and communication technologies is ‘health telematics’. With this in mind, telemedicine, as an integral part of health telematics, might be defined as:
Rapid access to shared and remote medical expertise by means of telecommunications and information technologies, no matter where the patient or the relevant information is located.4
What telemedicine is not
Telemedicine is not a technology or a separate or new branch of medicine, or for that matter even new. It is also not the panacea that will cure all of the world’s health-related problems or a means by which health-care workers can be replaced. It is also not an activity for antiquarians or Luddites, who range from those who are simply not at ease with the use of electronic machinery, right through to those who feel that telemedicine threatens the very fabric of the practice of medicine, and as such should be actively opposed. Equally, however, it is not the sole territory of‘computer nerds’ or ‘technophiles’. In fact, the tendency of these individuals to concentrate on the technical rather than the practical when discussing telemedicine may explain the antipathy of some clinicians towards practising medicine this way. Sensible, practical presentations by those who have actual experience of telemedicine have the potential to change the minds of those health-care workers who feel that telemedicine is not for them, either because it is ‘gimmicky’, industry-driven and therefore ‘less than respectable’, or unfathomable. Finally, and probably most important, for the most part telemedicine is far from being a mature discipline, and much work remains to be done to establish its place in health-care delivery.
Types of telemedicine
The common thread for all telemedicine applications is that a client of some kind (e.g. patient or health-care worker) obtains an opinion from someone with more expertise in the relevant field, when the parties are separated in space, in time or both. Telemedicine episodes may be classified on the basis of:
- the interaction between the client and the expert and
- the type of information being transmitted.
The type of interaction is usually classified as either prerecorded (also called store-and-forward) or realtime (also called synchronous). In the former, information is acquired and stored in some format, before being sent, by an appropriate means, for expert interpretation at some later time. Email is a common method of store-and-forward interaction. In contrast, in realtime interactions, there is no appreciable delay between the information being collected, transmitted and displayed. Interactive communication between individuals at the sites is therefore possible. Videoconferencing is a common method of realtime interaction.
The information transmitted between the two sites can take many forms, including data and text, audio, still images and video pictures. Combining the type of interaction and the type of information to be transmitted allows telemedicine episodes to be classified as in Figure 1.1. In certain applications, such as teleradiology, a technique that involves the transmission of digital radiographs between institutions, it is possible for the interaction to be either prerecorded or realtime; the latter requires that the expert be available to give an opinion as the image is taken and transmitted. Prerecorded and realtime telemedicine applications are discussed in Chapters 3 and 4.
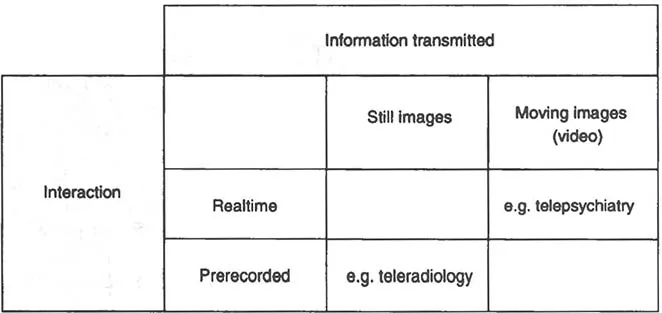
Figure 1.1 Classification system for telemedicine episodes
History of telemedicine
Most telemedicine has clearly occurred in the last 20-30 years, concomitant with advances in information technology. If, however, telemedicine is considered to be any medical activity performed at a distance, irrespective of how the information is transmitted, its history is much older. An early example of medicine at a distance, perhaps one of the first public health surveillance networks, was in the Middle Ages, when information about bubonic plague was transmitted across Europe by such means as bonfires. With developments in national postal services in the mid-19th century, the means by which more personal health-care delivery at a distance could be performed was facilitated, and the practice of physicians providing diagnosis, and directions for a cure, was established.
In the mid-19th century, telegraphy - signalling by wires - also began and was quickly deployed by those providing and planning for medical care. This included its use in the American Civil War to transmit casualty lists and order medical supplies, with later technological developments permitting X-ray images to be transmitted. In much of Europe and the USA, the telegraph was rapidly superseded by the telephone as a general means of communication, but in Australia it survived for much longer because of the enormous distances involved.
The telephone has been used for delivering health services since its invention in the late 19th century, and for 50 or so years remained the mainstay of communication for such purposes. However, it was realized as early as 1910 that the telephone could be used for purposes other than voice communication; amplified sounds from a stethoscope were transmitted through the telephone network and similar devices are still used today. Other uses for the ordinary telephone network have since been realized and include the transmission of electrocardiograms (ECGs) and electroencephalograms (EEGs).
The next development of widespread significance was at the end of the 19th century when communication by radio became possible. This was done initially by Morse code and later by voice. Use of the radio to provide medical advice for seafarers was recognized very quickly, and in 1920 the Seaman’s Church Institute of New York became one of the first organizations to provide medical care using the radio, with at least another five maritime nations establishing radio medical services by 1938. One of these was the International Radio Medical Centre (CIRM), whose headquarters are in Rome, Italy. It was set up in 1935 and in its first 60 years assisted with over 42,000 patients, making it the largest single organization in the world to use telemedicine to provide health care to seafarers.5 Radio medical advice for passengers on long-distance air journeys has also been provided more recently. For in-flight medical incidents that require professional assistance, and which occur at a rate of about 1 in 50,000 passengers carried, assistance can be obtained from on-call health-care workers on the ground.
The birth of modern telemedicine
The recent development of telemedicine has been facilitated on two fronts. First, there are the advances in electronic methods of communication. Initially, analogue methods were used, but now modem digital communication techniques are the mainstay. Second, telemedicine has developed because of the pioneering efforts of a few organizations and individuals. The former generally represented the interest of high-tech ventures, such as the manned space-flight programme of the National Aeronautics and Space Administration (NASA) in the USA. While these were no doubt of great importance in fostering the development of telemedicine and telecommunications generally, the efforts of a few individuals using readily-available commercial equipment have arguably been just as important for the development of telemedicine. It is interesting to note that in the 40 or so years since these individuals initiated their ventures things have changed relatively little, as far as who is doing research of practical value, and how it is being done.
A major influence on the development of telemedicine was the introduction of television. By the late 1950s, developments in closed-circuit television and video communications were made use of by medical personnel, who began to employ them in clinical situations. As early as 1964, a two-way closed-circuit television system was set up between the Nebraska Psychiatric Institute in Omaha and the state mental hospital in Norfolk, 112 miles (180 km) away.6 The system permitted interactive consultations between specialists and general practitioners, and facilitated education and training at the distant site. Another early example of television ...
Table of contents
- Cover Page
- Half title
- Title Page
- Copyright
- List of contributor
- Foreword to the first edition
- Preface to the first edition
- Preface to the second edition
- Section 1: Background
- 1. Introduction to the practice of telemedicine
- 2. Telemedicine systems and telecommunications
- Section 2: Telemedicine Applications
- 3. Prerecorded telemedicine
- 4. Realtime telemedicine
- 5. Tele-education
- Section 3: How to be Successful at Telemedicine
- 6. Defining the needs of a telemedicine service
- 7. Successfully developing a telemedicine system
- 8. Evaluating telemedicine systems and services
- 9. How to do a telemedical consultation
- Section 4: Other Aspects of Telemedicine
- 10. Benefits and drawbacks of telemedicine
- 11. Legal and ethical aspects of telemedicine
- 12. Sources of information on telemedicine
- 13. Telemedicine in the future
- 14. Conclusion
- Index