The primary purpose of professional regulation of doctors is to ensure patient safety. Revalidation is the professional regulatory mechanism that should allow doctors throughout the UK to demonstrate that they remain up to date and fit to practise. How the medical revalidation process is set up and runs will reflect the nature and level of risks to patient safety from the scope of practice of the medical profession.
We expected revalidation to start several years ago, once appraisal for consultants and GPs had bedded in. But now it looks as if revalidation will be launched for all doctors in the UK in 2010 after further piloting and refinements.1 It is likely that a fifth of doctors will undergo revalidation each year, with a five yearly relicensure cycle for every medic.
❱ ensure that individual doctors provide minimally acceptable standards of care in terms of the safety and quality of care given
❱ reassure patients and the public that medical professionals deserve their trust; sustain their confidence by the demonstrable impartiality of the regulatory system
❱ improve the quality of patient care through striving for best practice by: sustaining improvements in performance via measurement and feedback and by identifying and addressing poor practice or bad behaviour.2,3
The public’s expectations of doctors and their need to trust in the proficiency of doctors were illustrated by the results of a recent MORI survey; see Box 1.1. They expect doctors to undergo periodic checks to show that they are fit to practise.
The new look revalidation system
The main driver for the new look revalidation process for UK doctors was the review of medical regulation by the Chief Medical Officer of England.5 The recommendations of that review are to:
❱ strengthen procedures for assuring the safety of patients in situations where a doctor’s performance or conduct poses a risk to patient safety or the effective functioning of services
❱ ensure the operation of an effective system of revalidation
❱ modify the role, structure and functions of the GMC
❱ use clinically valid information as a tool for feedback on doctors’ performance and for public information
❱ continue to maintain public confidence and the trust of patients in doctors, with underpinning systems of quality and safety assurance6
❱ create a more devolved, less authoritarian system of medical regulation with more practical links to local practice settings.
We expect that there will be a similar approach to the revalidation of doctors across all four countries of the UK as far as possible. All four countries are committed to the professional regulation of doctors and other health professions including those professions new to regulation. But there are significant operational variations in the way that the systems for doctors’ appraisals are conducted in Scotland, Wales, Northern Ireland and England to take into account. There are also other differences in health practice, governance and regulation in the Devolved Administrations of Scotland, Wales and Northern Ireland. So, the new systems for revalidation will be piloted, and revised and then adopted or adapted to suit the different structures and systems in the four countries of the UK. Ways will need to be found to relicense doctors who practise in more than one country.
BOX 1.2 Main functions of the General Medical Council
As the medical profession’s regulator, the main functions of the GMC are to:
■ keep up-to-date registers of qualified doctors
■ set standards for good medical practice – ensuring Good Medical Practice 7 (a GMC publication) is part of everyday working practice
■ promote high standards of medical education
■ handle complaints and concerns about doctors’ fitness to practise: working with local management to identify problems.8
There are changes afoot to the membership of the GMC. At present 40% of the GMC are lay members. The government intends that the GMC and all other councils of healthcare regulators in the UK will be reconstituted so that lay members are in the majority and the public have a stronger voice in professional regulation.6 The Council for Healthcare Regulatory Excellence (CHRE) is the overarching UK body that promotes best practice and consistency in the regulation of healthcare professionals. The umbrella organisation covers nine separate regulatory bodies, of which one is the GMC. The main functions of the GMC are given in Box 1.2.
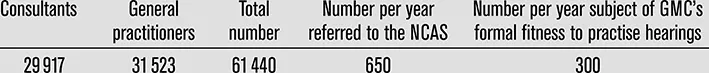
It is likely that the increased scrutiny of doctors’ practice through the revalidation process will reveal more doctors who are underperforming. The statistics in Box 1.3 describe the frequency of referrals of doctors about whom there are concerns, to the National Clinical Assessment Service (NCAS) and GMC. These put the extent of significant concerns about doctors’ poor performance into context. The rate of referral of doctors to the NCAS increases with age and rises steeply after 60 years for GPs, but not for secondary care doctors. Referral rates are lower for women doctors than their male counterparts.9
BOX 1.3 Numbers of doctors working in the NHS in England and referral rates to the GMC and NCAS9
International estimates give a 5% prevalence rate of hospital doctors with signifi-cant performance or conduct problems over a five year period. Taking into account the figures in Box 1.3, it has been calculated that each year in England around 4000 doctors will be identified for whom early intervention without further action is sufficient to address concerns about performance or behaviour. In addition, 1200 doctors might have a recorded concern and appropriate action be needed and there may be 380 doctors who need to be referred to the GMC. There will be proportionately similar numbers of doctors about whom there are concerns in Scotland, Wales and Northern Ireland. The proposed network of GMC Affiliates will see that appropriate action has been taken in individual cases; they will strengthen local governance systems to support relicensure. The revised roles suggested for medical directors and clinical governance leads in trusts will address the workload generated by this level and frequency of concerns about doctors’ performance, and intervene early as appropriate.3
It is mooted that the GMC Affiliates will provide advice, support and guidance to NHS organisations and their senior personnel on local action and investigations they should take to address concerns about doctors. They should monitor the investigations and decisions subsequently taken. They might assist employers and others in agreeing, developing and delivering packages of assessment, treatment, rehabilitation, remediation, retraining or supervised practice. These packages will be designed for doctors who need assistance in preventing their emerging difficulties from becoming a regulatory matter or who require support or rehabilitation following NCAS or GMC involvement. They may also organise random sampling of the local relicensing process as part of a quality assurance role.3
The GMC is working with NCAS to review the various assessment tools both organisations use as part of the NCAS formative assessment service and the GMC’s review of a doctor’s fitness to continuing to practise. The two organisations are harmonising many of the instruments both use in work based assessment, in order to be able to share information if a doctor moves from a NCAS assessment to a GMC review. Some medical Royal Colleges are working on knowledge and skills assessments that relate to the GMC’s Good Medical Practice describing the duties of a doctor 7 and helping with developments in the GMC’s clinical assessment centre.
The recent revision of Good Medical Practice 7 and the supplementary guidance Maintaining Boundaries 10 includes new emphases on the following.
❱ Your duty as a doctor to maintain a folder of information and evidence about medical practice and to reflect on professional practice, in anticipation of relicensing and revalidation.
❱ Your duty to ‘be familiar with’ your GMC reference number.
❱ Your duty to work contractual notice periods ‘unless the employer has reasonable time to make other arrangements’.
❱ Your duty to ensure that ‘your conduct at all times justifies your patients’ trust in you and the public’s trust in the profession’.
❱ Warnings against misrepresenting experience, qualifications or position, particularly when you are applying for a new post.
❱ The doctor-patient partners...