![]()
Part 1
The infrastructure of audit
![]()
1
Introduction to clinical audit
Getting started with clinical audit
Audit is a technique used to maintain and improve the quality of care and services provided by an individual or by a practice. It is the method used by ‘health professionals to assess, evaluate, and improve the care of patients in a systematic way, to enhance their health and quality of life’.1 Clinical audit is central to clinical governance because:
• you can use it to review the quality of care you provide for patients with common conditions like asthma or diabetes, on an everyday basis
• it builds on the way that health professionals and others working in the NHS have traditionally reviewed case notes as part of quality improvement
• it provides a systematic approach to reviewing the quality of care and services
• it supplies reliable information to highlight the need for improvements
• it provides an impetus to upgrade the quality of care you provide.
Clinical audit is a quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change. Aspects of the structure, processes and outcomes of care are selected and systematically evaluated against explicit criteria. Where indicated, changes are implemented at an individual team or service level and further monitoring is used to confirm improvement in healthcare delivery.2
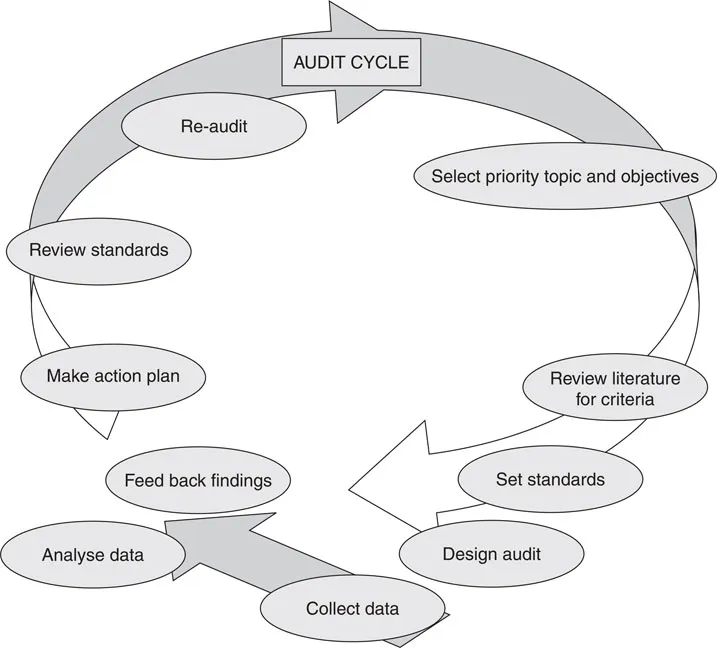
The steps of the audit cycle represented in Figure 1.1 are:
• prioritise and select the topic of your audit, working with others in your team or practice
• set objectives: relating to the reason(s) why the audit is being carried out
• review the literature for that topic and agree the criteria and standards that you think are reasonable
• design the way in which you will do the audit
• collect the data and look at them
• feed back the findings; meet with colleagues or your team to discuss the findings and determine the reasons for the results
• make a timetabled action plan to implement any changes that are needed
• review your standards – should you keep the standards you previously set, are they unrealistic or not challenging enough?
• re-audit – creating successive audit cycles.
Designing your clinical audit
The more time you spend planning and designing the clinical audit, the more likely it is that you can move easily through these various steps of the audit cycle and obtain useful information that everyone owns and agrees to act on. Write down your protocol and share the agreed version so that everyone can see the part they play.
Figure 1.1: Steps in the audit cycle
Who will be involved?
Include those members of the practice team who are directly involved in the task being audited and those who will be collecting the data. Decide who is writing the audit protocol and who will search for evidence to enable you to set standards and criteria. Include in the team those who need to agree solutions or find resources if the audit shows that change is necessary. Appoint a lead if there is no-one in this role already. Link to others relevant to the audit who work in different settings: the local hospital, primary care organisation (PCO), community clinic, social services, etc.
Set simple, measurable, achievable, realistic and timely (SMART) objectives
You should be clear about the reason(s) for doing the audit, and the objective you set should link to that – to define the extent of potential risk areas, for example. The objectives should be relevant and understandable to everyone taking part. Keep in mind that the end result is making improvements to patient care. The quality and nature of the end points of your audit should relate to the objective(s) you set for the audit. You need to have some idea of your endpoint when you set the objective(s). The audit will be most worthwhile if your objective is about:
• assessing whether or not standards are being met
• determining whether standards are improving
• monitoring the level of compliance or concordance with treatment or advice
• improving clinical effectiveness
• changing inadequate current practice.
Box 1.1: Example of objectives of an audit of local services, e.g. management of suspected myocardial infarction
Main objective: to audit the extent to which the following criteria were met and to identify reasons for failure to implement the policy for the management of suspected heart attack:
• the proportion of patients who receive thrombolytic therapy within six hours of the onset of chest pain and within 30 minutes of arrival at hospital
• the length of time patients wait from the onset of symptoms before calling emergency services
• the response time of emergency medical services
• whether aspirin is administered, by whom, and when.
Set criteria
These are items by which you will appraise the indicators of the level of care. The level of performance in your audit results will describe the extent to which these criteria are met. Criteria are explicit statements that define what is being measured; they represent elements of care that can be measured objectively.2
Set standards
Standards are indicators of the level of care that you want to achieve. They may be those that you have agreed as a practice team, are promoted by others such as in the Quality and Outcomes Framework,3 or in other published literature, such as systematic reviews or national clinical guidelines.
Data collection
Decide what information you wish to collect and how to collect it in a reliable way, minimising bias as far as possible. You may need to pilot the collection of data to see how that works out, and solve any problems that arise. Decide if the data collection is retrospective, concurrent or prospective. The data collected must be valid and accurate. The data should be readily available on your computer system or from patient surveys. You will not have time or resources to track down hard-to-locate information.
Define the sample
See page 23 for how you might select your sample of who will be included and excluded from the audit. The number in your sample and the trouble you take to get a representative sample will depend on the accuracy or degree of confidence you need to have in the findings, and the extent to which you are limited by time, funds, staff skills etc.
Data analysis
Decide who will look at the data, how the analysis will be done and how the interpretations will be made.
Feed back the findings
Feedback should be to the people involved in the audit and anyone who will need to make changes. You might be feeding back findings further afield – in your appraisal or in your revalidation or re-registration portfolio, or to the PCO as part of the Quality and Outcomes Framework.
Draw up the action plan
The action plan needs to be timetabled and specific about who does what, how and when – and realistic. The need for any extra resources should be predicted and how they will be identified included in the action plan. If the actions or changes mean new responsibilities for staff, then you need to anticipate their training requirements and organise that training in work or paid time. See Chapter 4 for how you might facilitate the changes necessary.
Convene an implementation group
Everyone concerned in the action plan will need to discuss progress with someone taking the lead. If it is a complex audit or crosses more than one health setting, you will probably need an occasional group meeting to oversee progress and agree on re-auditing.
Re-audit
You will want to re-audit if your initial audit showed gaps in the care you are providing and you have made changes as a consequence, to see if you are now meeting, or approaching, the criteria and standards you have set.
Angle what clinical audit you do on:
• a clear patient focus
• greater multiprofessio...