eBook - ePub
A Practical Manual of Hysteroscopy and Endometrial Ablation Techniques
A Clinical Cookbook
This is a test
- 284 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
A Practical Manual of Hysteroscopy and Endometrial Ablation Techniques
A Clinical Cookbook
Book details
Book preview
Table of contents
Citations
About This Book
Keeping up with the rapid growth in this field, A Practical Manual of Hysteroscopy and Endometrial Ablation: A Clinical Cookbook covers current and emerging endometrial ablation procedures. It provides practical, step-by-step illustrated descriptions of basic and advanced techniques and new methods. The editors, Resad Pasic and Ronald L. Levine, ha
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access A Practical Manual of Hysteroscopy and Endometrial Ablation Techniques by Resad P. Pasic, Ronald Leon Levine in PDF and/or ePUB format, as well as other popular books in Medicina & Teoría, práctica y referencia médicas. We have over one million books available in our catalogue for you to explore.
Information
CHAPTER 1
SALINE INFUSION SONOGRAPHY
Linda D.Bradley, M.D.
The introduction of intracervical fluid during TVUS (Transvaginal Uterine Sonography) constitutes one of the most significant advances in ultrasonography during this past decade. Instillation of saline during ultrasound (SIS) enhances and augments the image of the endometrial cavity, as well as provides valuable information about the uterus and adnexa in patients with abnormal bleeding. Given the disparity between endometrial biopsy results and TVUS evaluation, pathologic reports including: “insufficient tissue,” “atrophic endometrium,” or “scant tissue” on biopsies are no longer sufficient to rule out pathology. SIS provides an exquisite view of the endomyometrial complex that cannot be obtained with TVUS alone. SIS differentiates between focal and global processes and improves the overall sensitivity for detecting abnormalities of the endometrium.
Saline infusion sonography overcomes the limitations of traditional TVUS for evaluating menstrual and postmenopausal bleeding disorders. It offers the advantages of distending the uterine walls to create a threedimensional view of the uterus, and provides a more concentrated visualization of the endometrium and myometrium. This information helps to determine whether endometrial biopsy is needed, select the type of surgical procedure, ascertain the hysteroscopic expertise required to remove the lesions, and judge the resectability of lesions.
Saline infusion sonography is a procedure whereby saline is infused into the endometrial cavity during TVUS to enhance the endometrial view. Although many terms have been used to describe this technique (e.g., echohysteroscopy, hydrosonography, sonohysterography, sonohysterosalpingography, sonoendovaginal ultrasonography) the acronym SIS, saline infusion sonography, was coined by Widrich, Bradley and Collins in 1996, and more clearly defines the technique employed.
In comparison to hysteroscopy, SIS more reliably predicts depth of myometrial involvement of uterine fibroids and their size. For a successful surgical outcome, it is important to identify preoperatively the size, number, location, and depth of intramural extension. Fibroid size and location affect resectability, the number of surgical procedures necessary for complete resection, the duration of surgery, and the potential complications from fluid overload. SIS classification was developed for uterine fibroids, based on the purpose of planning surgery, determining resectability of lesions, and to standardize the comparison of surgical outcomes.
CLINICAL ROLE OF SALINE INFUSION SONOGRAPHY IN THE EVALUATION OF MENSTRUAL DISORDERS
COMMON INDICATIONS FOR PERFORMING SIS:
- EVALUATION OF MENSTRUAL DISORDERS IN THE PREMENOPAUSAL OR POSTMENOPAUSAL PATIENT.
- EVALUATION OF THE ENDOMETRIUM WHEN IT IS POORLY VISUALIZED, THICKENED, IRREGULAR, OR NOT IMAGED WELL BY CONVENTIONAL TVUS, MRI OR CAT SCAN STUDIES.
- EVALUATION OF A BIZARRE, IRREGULAR, OR INHOMOGENEOUS ENDOMETRIUM IN WOMEN ON TAMOXIFEN.
- EVALUATION OF PATIENTS WITH RECURRENT PREGNANCY LOSS OR INFERTILITY.
- POST SURGICAL EVALUATION OF THE ENDOMETRIUM.
- THE NEED TO DIFFERENTIATE BETWEEN SESSILE AND PEDUNCULATED MASSES OF THE ENDOMETRIUM.
- TO EVALUATE THE SURGICAL FEASIBILITY OF HYSTEROSCOPIC MYOMECTOMY.
- TO ASCERTAIN THE CLASSIFICATION OF UTERINE FIBROIDS (SIZE, NUMBER, LOCATION).
- CLARIFY FINDINGS WITH HYSTEROSALPINGOGRAM (HSG).
- EVALUATION OF RECURRENT PREGNANCY LOSS.
- PRESURGICAL EVALUATION OF INTRACAVITARY FIBROIDS, TO DETERMINE THE DEPTH OF MYOMETRIAL INVOLVEMENT AND OPERATIVE HYSTEROSCOPIC RESECTABILITY.
- POST SURGICAL EVALUATION OF THE ENDOMETRIUM.
- TO DETERMINE ENDOMETRIAL CHANGES DUE TO TAMOXIFEN.
SIS TECHNIQUE
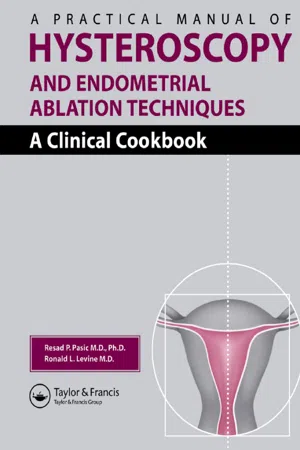
Although SIS can be performed transvaginally or transabdominally, most physicians use the transvaginal approach (Figure 1). No anesthesia or analgesia is required. Most patients are very comfortable. This procedure is best scheduled when the patient is not bleeding. Reproductive aged women ideally should be scheduled during the early proliferative phase—preferably 4–10 days after menses has ended. The risk of interrupting a viable intrauterine pregnancy is lowest at this time. Additionally, fewer false positive results, and fewer artifacts caused by shearing of the endometrial cavity will occur. Visualization of endometrial polyps and fibroids is enhanced during the early proliferative phase.
PREPARATION
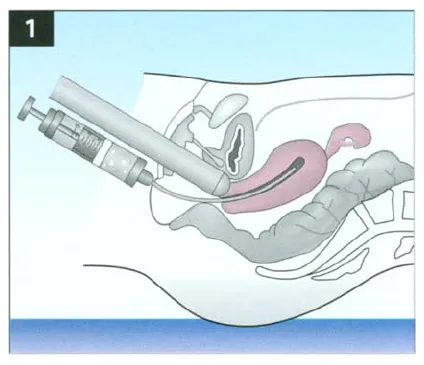
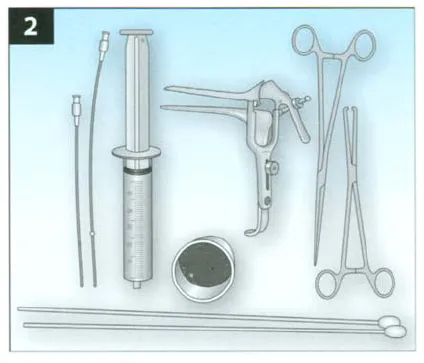
The required instruments are shown in Figure 2. Antibiotics are not routinely given except for patients who have symptoms or signs of pelvic infection, prior history of pelvic inflammatory disease, mitral valve prolapse, cardiac valves, or artificial hips. Patients may elect to use nonsteroidal anti-inflammatory drugs (NSAIDs) one to two hours before the procedure. Thus, SIS requires minimal preparation and no anesthesia. Women with cervical stenosis may benefit from placement of laminaria tents or misoprostol (orally 100 mcg 8 to 12 hours before the procedure or vaginally 200 mcg to 400 mcg 6 to 8 hours before the procedure). Uterine sounding may sufficiently disrupt synechiae. Cervical traction with a single-toothed tenaculum can straighten the uterine axis if marked retroversion is present (Figure 3).
1
2
Voiding before SIS is important. Bladder distention is not required. In fact, it can alter the position of an anteverted uterus to retroverted, making evaluation with a transvaginal probe onerous. After informed consent is obtained, a bimanual examination is performed with the patient in the dorsal lithotomy position. An absorbent towel placed under the patient will minimize fluid accumulation.
Conventional TVUS is performed using a transvaginal probe covered with a condom and gel. Visualization of the cervix is aided by placing an open-sided speculum in the vagina to facilitate introduction of the intrauterine catheter and permit easy removal of that same speculum without displacing the catheter.
3
The cervix is cleansed with an antiseptic solution, such as Betadine or Hibiclens. The intrauterine catheter then is inserted with the assistance of a ring forceps or uterine forceps.
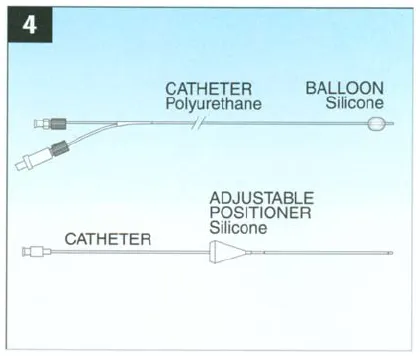
The catheter should be placed to barely touch the fundus. Several flexible intrauterine catheters that provide easy access to the endometrium are currently available. I prefer the 25-cm long, 5.6 F Soules which is a 1.8 mm (Cook Ob/Gyn, Indianapolis, IN) intrauterine insemination catheter. It is inexpensive and easy to use and place within the uterus. Its long length allows extension through the introitus, which permits easy attachment of a sterile syringe. For conditions such as incompetent cervix, Asherman’s syndrome, or patulous cervix, a balloon-type catheter is useful to optimize uterine distention and minimize fluid loss (Figure 4).
Before the catheter is inserted, it is flushed with sterile saline to decrease artifacts caused by bubbles. A straight catheter should be introduced with sterile uterine packing forceps until the fundus is reached. If distention is inadequate, it may be helpful to pull the catheter back. When cervical stenosis is encountered, a tenaculum or uterine sound can be used to assist in placing the catheter.
After the open-sided speculum is removed, the Soules catheter will protrude from the vagina, allowing easy attachment of a 60 mL plastic syringe containing sterile saline. Air bubbles should be evacuated from the syringe also, to prevent artifacts.
SIS is a dynamic procedure, and images are best seen in real time. Excellent images and adequate distension usually are obtained with minimal fluid instillation (5–30 mL). Ideally, 5 to 10 mL/min are infused. If the uterus cannot be distended, placing a balloon-tipped catheter and infusing the saline more slowly may help. Air bubbles may accumulate but rapidly disappear as the injection continues. More fluid can be safely used if the patient is bleeding or has blood clots, or if there is poor visualization.
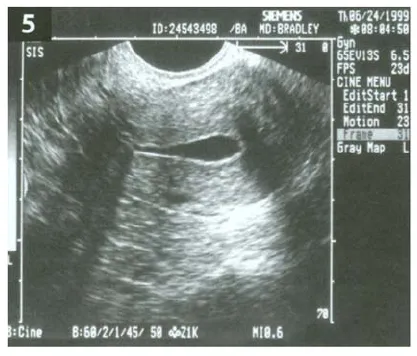
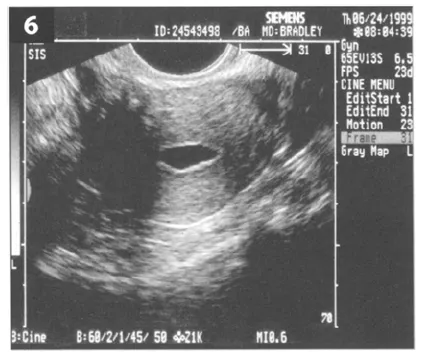
It is essential to employ a systematic technique for viewing the uterus and to watch the video monitor as the scan is performed. As the endometrial cavity unfolds on the screen, it is important to view the uterus as a three-dimensional structure that must continually be recreated as scanning continues. This threedimensional image is achieved by scanning from cornua to cornua in the long axis (sagittal plane) (Figure 5) and then turning the probe 90° and scanning from the endocervix to the fundus in the transverse plane (Figure 6). The sagittal view permits visualization of the uterine cavity and measurement of the endometrial echo. The adnexa are visualized in the semi coronal plane. The cervix and cul-de-sac are viewed as the transducer is withdrawn. Uterine symmetry and myometrial or intracavitary lesions are appreciated best by slowly scanning transversely from the external os to the fundus. Fleischer et al recommend measuring both layers of the endometrial echo (which represent the anterior and posterior uterine wall basal layers) in the sagittal view to obtain the most accurate measurement of the endometrium. The hypoechoic subendometrial halo should not be included because it represents the vascular layer of myometrium. Both TVUS and SIS can be performed in 10–15 minutes in most patients.
4
5
6
FINDINGS
ENDOMETRIAL POLYPS
Endometrial polyps occur frequently in the reproductive and menopausal years. They more commonly occur in women on tamoxifen. Polyps are usually single, falsely widen the endometrial echo when imaged with TVUS alone, do not disrupt the endomyometrial complex and appear homogeneous with microcystic changes (Figure 7). Sometimes cystic spaces within an abnormally thickened endometrium tend to be predictive of polyps.
INTRAUTERINE FIBROIDS
Fibroids are difficult to locate with conventional TVUS because they transmit sound poorly, attenuate the beam, and have ill-defined borders. Fibroids may obscure measurements of the endometrium by creating an irregular endomyometrial interface. They may have varied appearance, including cystic, calcific, hypoechoic, echogenic, isoechoic, and mixed echogenic patterns. Degenerating fibroids often appear cystic. Location of fibroids is improved with SIS. The endometrium adjacent to the fibroid appears echogenic. Additionally, location, size, and degree of intramural extension can be classified with SIS.
The following classification of intracavitary uterine fibroids based on SIS was developed for the purpose of planning surgery. Notice that this classification differs from the hysteroscopic classification described in Chapter 12. SIS Class 1 fib...
Table of contents
- Cover Page
- Title Page
- Copyright Page
- Contributing Authors
- Preface
- Foreword
- Acknowledgements
- Chapter 1: Saline Infusion Sonography
- Chapter 2: Hysteroscopic Instruments
- Chapter 3: Distension Media in Hysteroscopy
- Chapter 4: Choice of Anesthesia
- Chapter 5: Electrosurgery in the Uterus
- Chapter 6: Techniques for Diagnostic Hysteroscopy, Hysteroscopic Resection and Cystoscopy
- Chapter 7: Office Hysteroscopy
- Chapter 8: Hysteroscopy for Infertility
- Chapter 9: Endoscopic Treatment of Uterine Anomalies
- Chapter 10: Cannulation of the Fallopian Tube
- Chapter 11: Hysteroscopic Tubal Sterilization
- Chapter 12: Hysteroscopic Myomectomy
- Endometrial Ablation Techniques
- Chapter 13: Endometrial Resection
- Chapter 14: Thermachoice Balloon Ablation
- Chapter 15: Hydrothermal Ablation (HTA®)
- Chapter 16: Microwave Endometrial Ablation
- Chapter 17: Endometrial Cryoablation
- Chapter 18: Novasure™ Global Endometrial Ablation
- Chapter 19: Repeat Endometrial Ablation
- Chapter 20: Hysteroscopic Surgery: Indications, Contraindications and Complications