This is a test
- 96 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Book details
Book preview
Table of contents
Citations
About This Book
Acne, rosacea, and sebaceous hyperplasia are very common skin problems, which have a significant medical, cosmetic, and often psychological impact on the daily lives of millions of people. This book covers both the medical and cosmetic aspects of these skin disorders including all clinical considerations, etiology, epidemiology, diagnostic challeng
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Acne and Rosacea by David Goldberg, Alexander Berlin in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Theory, Practice & Reference. We have over one million books available in our catalogue for you to explore.
Information
1 ACNE VULGARIS – EPIDEMIOLOGY AND PATHOPHYSIOLOGY
INTRODUCTION
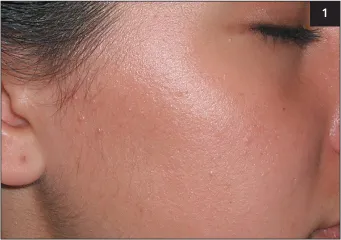
ACNE vulgaris is a common disorder of the pilosebaceous unit affecting millions of people worldwide. Although most frequently encountered in adolescents, acne may persist well into adulthood and lead to significant physical and psychological impairment in those affected. The severity of acne may vary significantly from the mildest comedonal forms (1) to a severe and debilitating condition (2). In addition to the face, the chest, back, and shoulders are also commonly affected (3, 4).
1 Mild comedonal acne on a patient’s face.
2 Severe cystic acne.

3 Acne papules and pustules on the chest.

4 Acne papules associated with extensive postinflammatory hyperpigmentation on a patient’s back.

5 In acné excoriée des jeunes filles, patients frequently manipulate their acne lesions, leading to prolonged healing time and often, scarring.

Numerous factors, both intrinsic and extrinsic (5), may underlie the development and the progression of the disease.
EPIDEMIOLOGY
Acne is the most common cutaneous disorder in the Western world. In the United States, its prevalence has been variably estimated at between 17 and 45 million people (Berson et al. 2003; White 1998). This number is typically based on a landmark publication by Kraning & Odland (1979), which estimated the prevalence of acne in persons aged 12–24 years at 85%.
Several studies have documented that a significant portion of acne sufferers are postadolescent or adult (Collier et al. 2008; Cunliffe & Gould 1979; Goulden et al. 1997; Poli et al. 2001, Stern 1992).A recent study based on 1013 surveys found the overall prevalence of acne in patients 20 years of age and older to be 73.3% (Collier et al. 2008). Among such patients, women are affected at higher rates than men in all age categories. Thus, more recent studies place the incidence of clinically-important adult acne at 12% of women and 3% of men over 25 years of age. If milder, ‘physiologic’ acne is taken into consideration, the prevalence increases to 54% of women and 40% of men (Goulden et al. 1997). Adult acne may present as a continuation of the teenage disease process or may arise de novo. Acne is also encountered in the preadolescent population, including neonates and, less commonly, infants and preteens (Cunliffe et al. 2001; Jansen et al. 1997; Lucky 1998).
The prevalence of acne in individuals with skin of color has, likewise, been investigated in several studies (6, 7). Thus, Halder et al. (1983) reported acne being present in 27.7% of the Black patients and 29.5% of the Caucasian patients. Additional studies of adult patients in the United Kingdom and Singapore have placed the prevalence of adult acne at 13.7% of the Black patients and 10.9% of the Indian and Asian patients (Child et al. 1999; Goh & Akarapanth 1994). It has also been shown that the presence of significant inflammation, resulting in the clinical appearance of nodulocystic acne, is more common in Caucasian and Hispanic patients than in their Black counterparts (Wilkins & Voorhees 1970). More recent evidence indicates that subclinical, microscopic inflammation may be more common in the latter group (Halder et al. 1996).
It has also been suggested that certain non-westernized societies demonstrate significantly lower prevalence of acne (Cordain et al. 2002; Schaefer 1971; Steiner 1946). The cause of such disparity is unclear and although nutritional factors have been suggested as the cause of lower acne rates, this inference has so far not been conclusively substantiated (Bershad 2003).
The issue of nutrition and its influence, or lack thereof, on acne has long been a highly contested one (Adebamowo et al. 2005; Bershad 2003; Bershad 2005; Cordain 2005; Danby 2005; Kaymak et al. 2007; Logan 2003; Smith et al. 2007; Treloar 2003). Proponents of the link between acne and nutrition frequently cite nutritional influence on serum hormone levels, such as insulin-like growth factor (IGF)-1 and IGF binding protein-3, to demonstrate the purported effect on acne. Thus, foods with a low glycemic load–those that cause least elevation of blood glucose and have lowest carbohydrate content–as well as diets high in omega-3 essential fatty acids, have been advocated as beneficial for acne patients (Cordain 2005; Logan 2003; Smith et al. 2007; Treloar et al. 2008). Additionally, milk has been proposed as a potential culprit in acne causation, with arguments being raised as to the presence of various hormones in the consumed product (Adebamowo et al. 2005, Danby 2005). On the other hand, those refuting the link between acne and nutrition may cite two flawed studies from over 30 years ago (Anderson 1971; Fulton et al. 1969). In reality, controlling diet in a study is difficult, especially when it involves teenagers. As it stands now, there are far too few large, well-designed, well-controlled prospective clinical studies to substantiate either point of view. This is in accordance with the current guidelines of care from the American Academy of Dermatology (Strauss et al. 2007).
6 Postinflammatory hyperpigmentation is a common consequence of acne in patients with darker skin tones, such as this Indian patient.

7 Extensive postinflammatory hyperpigmentation in an African-American patient with acne.

Smoking and its influence on acne prevalence and severity has been investigated in several published clinical trials (Chuh et al. 2004; Firooz et al. 2005; Jemec et al. 2002; Klaz et al. 2006; Mills et al. 1993; Rombouts et al. 2007; Schafer et al. 2001). Of these studies, two suggested a positive association between smoking and acne, three proposed a negative one, and two found no association. Thus, the evidence so far is inconclusive; however, taking into consideration other, more serious health risks associated with smoking, cessation should always be encouraged.
Very importantly, acne may arise in a number of genetic and endocrinologic conditions, and the genetic component of acne vulgaris has been well documented. For example, patients with the XYY genotype and those with polycystic ovarian syndrome, hyperandrogenism, and elevated serum cortisol levels have a significantly increased risk of developing acne (Lowenstein 2006; Mann et al. 2007; New & Wilson 1999; Stratakis et al. 1998; The Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group 2004; Voorhees et al. 1972) (8). Additionally, there is a high level of concordance in acne severity between monozygotic twins, while adult acne has been demonstrated to occur with a much higher frequency in those with first-degree relatives suffering from the same condition (Bataille et al. 2002; Evans et al. 2005; Friedman 1984; Goulden et al. 1999; Lee & Cooper 2006).
8 A combination of acne and hirsutism, such as on the neck of this patient, may point to an underlying state of hyperandrogenism.

CLINICAL ASSESSMENT OF ACNE VULGARIS
Acne vulgaris frequently presents with a combination of morphological features, including open and closed comedones, papules, pustules, and nodules (9–11). The mildest form of acne is comedonal acne, characterized by the absence of inflammatory lesions. On the other side of the spectrum is acne conglobata, presenting with large, interconnecting, tender abscesses and irregular scars causing profound disfigurement. More acute and severe in presentation is acne fulminans, a multisystem syndrome of sudden onset, characterized by necrotizing acne abscesses associated with fever, lytic bone lesions, polyarthritis, and laboratory abnormalities (Jansen & Plewig 1998; Seukeran & Cunliffe 1999).
In order to assess the initial severity of acne and to follow patient progress in a clinical setting, as well as to be able to evaluate the efficacy of various therapeutic agents in clinical trials, an objective measurement technique is important. Numerous systems have been developed over the years; however, no clear winner has so far emerged.
9 Extensive open and closed comedones.

10 Extensive acne papules on a patient’s face.

11 Nodulocystic acne.

The first published attempt to measure the severity of disease in acne appeared in a dermatological textbook in 1956 (Pillsbury et al. 1956). This technique assigned grades to acne severity, ranging from 1 to 4, based on the overall type and number of lesions, the predominant lesion, and the extent of involvement. Several modified grading systems have since been introduced, some utilizing reference photographs or polarized light photography (Burke & Cunliffe 1984; Cook et al. 1979; Doshi et al. 1997; James & Tisserand 1958; Phillips et al. 1997).
Developing in parallel with acne grading techniques were the various systems emphasizing lesion counts (Christiansen et al. 1976; Lucky et al. 1996; Michaelson et al. 1977; Witkowski & Simons 1966). This method typically involves counting individual lesions in each morphological category and frequently subdivides the face into separate regions. Lesion counting was recently validated and appears to be more objective than acne grading (Lucky et al. 1996). Still, multiple arguments between acne graders and lesion counters have arisen in the literature (Shalita et al. 1997; Witkowski & Parish 1999), and none of the current methods of acne assessment are entirely perfect. Some systems actually combine lesion counting with overall grading (Plewig & Kligman 1975). In reality, two standardized, validated systems are likely necessary: one that can be easily and rapidly applied in a clinical setting without the need for intricate instrumentation, and a separate, more sensitive approach that can be utilized in clinical research.
PATHOPHYSIOLOGY OF ACNE VULGARIS
Over the last several years, our understanding of the pathogenesis of acne has increased dramatically. The new research findings will likely lead to new advances in acne therapy, as well as the elucidation of pathogenesis of other cutaneous conditions.
The traditional view of the pathogenesis of acne is frequently termed the microcomedone theory. According to this theory, the initial step in the disease process is hyperkeratosis of the follicular lining in the proximal part of the upper portion of the follicle, the infrainfundibulum. This is accompanied by the increased cohesiveness of the corneocytes within this lining and results in a bottleneck effect within the follicle. As the shed keratinocytes and sebum continue to accumulate, they undergo a transformation into whorled lamellar concretions, resulting in a clinical appearance of a comedone. Propionibacterium acnes (P. acnes) bacteria proliferate within an expanding comedone, prompt a host response, and contribute to the production of inflammatory acne, clinically manifesting as papules and pustules. Finally, as the shed keratinocytes and sebum continue to accumulate, internal pressure leads to the rupture of the comedo wall with subsequent marked inflammation and nodule formation. Such intense inflammation may eventually lead to scar...
Table of contents
- Cover Page
- Acne and Rosacea: Epidemiology, Diagnosis and Treatment
- Copyright Page
- CONTENTS
- ABBREVIATIONS
- PREFACE
- 1 ACNE VULGARIS – EPIDEMIOLOGY AND PATHOPHYSIOLOGY
- 2 ACNE VULGARIS – CURRENT MEDICAL THERAPEUTICS
- 3 LASERS AND SIMILAR DEVICES IN THE TREATMENT OF ACNE VULGARIS
- 4 TREATMENT OF ACNE SCARS
- 5 ROSACEA — EPIDEMIOLOGY AND PATHOPHYSIOLOGY
- 6 ROSACEA — CURRENT MEDICAL THERAPEUTICS
- 7 LASERS AND SIMILAR DEVICES IN THE TREATMENT OF ROSACEA
- 8 LASERS AND SIMILAR DEVICES IN THE TREATMENT OF SEBACEOUS HYPERPLASIA
- REFERENCES
- INDEX