eBook - ePub
Sleep Disorders Handbook
A Handbook for Clinicians
This is a test
- 196 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Book details
Book preview
Table of contents
Citations
About This Book
Recent years have seen the rapid development of sleep medicine as a new medical subspecialty. It is estimated that at least 30% of the adult population suffer at least once from some sort of sleep disturbance. Patients with sleep disorders are frequently among the most difficult to treat and account for a high percentage of absenteeism in the workp
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Sleep Disorders Handbook by Peretz Lavie, Giora Pillar, Atul Malhotra in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Theory, Practice & Reference. We have over one million books available in our catalogue for you to explore.
Information
chapter 1
History of sleep medicine
Sleep and dreams have been popular throughout time for writers, researchers and physicians alike. However, most of our modern knowledge of sleep medicine was achieved only in the last four decades. There have been several breakthrough discoveries that paved the way to the scientific investigation of sleep (Table 1).
To date, the understanding of why we sleep and the precise sleep control mechanisms of the brain are far from being completely elucidated. Previously, it was believed that sleep is a time of quiescence and tranquillity, a time when the body and mind relax to recuperate from the day’s activity, a time when relatively little happens. These assumptions are partially incorrect because sleep is, in fact, an active process. At the start of the nineteenth century, the major sleep theory was that of the hypnotoxins. This theory posited that when we are awake there is an accumulation of poisonous hypnotoxin which drives sleepiness. Hypnotoxins were thought to be detoxified only during sleep. The discovery that serum from sleep-deprived dogs injected into alert dogs caused them to fall asleep (Legendre and Pieron) provided strong support for this theory.
Table 1 Hallmarks of sleep research
Currently, several mediators, such as adenosine, interleukins, tumournecrosing factor, prostaglandins, lipopolysaccharides and δ-producing proteins, have been proposed to mediate the homoeostatic drive for sleep. Sleep, however, is not regulated by just homoeostatic principles. The discovery by Kleitman that, even with on-going sleep deprivation, one can be less sleepy the following morning suggested that additional factors control the drive for sleep. Indeed, the current agreement among sleep researchers is that sleep is regulated by two factors: the duration of wakefulness (homoeostatic drive to sleep) and the time of day (circadian drive to sleep). The absolute drive to sleep at any point in time is therefore the combination of these two drives.
The discovery of the electroencephalogram in 1928 by Berger provided a quantum leap for sleep research. Applying the new methods to measure EEG activity in sleeping people, or animals, revealed that the transition from wakefulness to sleep is accompanied by specific and well-characterized changes in brain wave activity (Table 2 and Figure 1). Electrocephalography (EEG) has allowed widespread investigations of brain mechanisms controlling sleep and wakefulness by several investgators, including Frederick Bremer, Moruzzi and Magoun, Michele Jouvet and others. There is still an on-going effort for further understanding of the brain circuitry participating in sleep regulation.
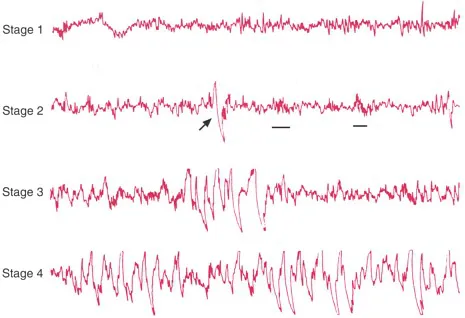
Figure 1 EEG examples from the various sleep stages. (See text for further explanation.)
Table 2 Physiological characteristics of the various stages of sleep
Normal sleep
During sleep there are periods of physiological and autonomic activation reaching waking levels. EEG and other physiological recordings during sleep define two distinct states of sleep: rapid eye movement (REM) sleep and non-REM (NREM) sleep. The latter is divided into four different stages: stage 1 (light sleep), stage 2 (consolidated sleep), and stages 3 and 4 (deep, or slow wave sleep). Division of sleep into these stages relies on three physiological variables: EEG, electromyography (EMG) and electro-oculography (EOG) as demonstrated in Table 2 and Figure 1.
The different EEG patterns that are characteristic of non-REM sleep stages are shown in Figure 1. Stage 1 is characterized by relatively low-amplitude θ activity intermixed with episodes of a activity. In stage 2 there are K-complexes (marked with an arrow) and sleep spindles (marked by underlining), whereas stages 3 and 4 are dominated by increasing amounts of slow-wave high-amplitude (δ) activity.
During normal sleep, these stages tend to occur in succession, forming a unique ‘sleep architecture’ (see Chapter 2). Generally, from wakefulness an individual falls into stage 1 sleep, followed by stages 2, 3 and 4 and REM sleep. This succession of sleep stages, culminating in REM sleep, forms a ‘sleep cycle’. The length and content of sleep cycles change throughout the night as well as with age. The relative percentage of deep sleep is highest in the first sleep cycle and decreases as the night progresses, whereas the relative length of REM sleep episodes increases throughout the course of the night. When totalling the various sleep stages through the night in normal young adults, stage 1 occupies up to 5% of the night, stage 2, 50%, and REM sleep and slow wave sleep (SWS) 20–25% each. These relative percentages change with age, as does the cycle length. In infants the normal cycle of sleep lasts about an hour, whereas in adults it lasts about 1.5 hours. Table 3 demonstrates the percentages of different sleep stages and sleep length at different ages.
Brief body movements, which may be accompanied by arousals, mark transitions to and from REM sleep. These four to eight brief awakenings, which are too short to be registered in the memory, are not considered abnormal or sleep disruption. This point is important to keep in mind when dealing with complaints about sleep. It is the difficulty in falling back to sleep, once brief awakening has occurred, rather than the awakenings themselves that may need to be treated. In some sleep disturbances, however, there is a large increase in the number of brief arousals from sleep, which indeed needs medical attention.
Table 3 Changes in sleep content and length with age
Sleep needs and the function of sleep
One of the most popular questions that almost every sleep expert is faced with is ‘How many hours do I need to sleep?’. As presented in Table 3, total hours of sleep are age dependent. Within each age group, however, there are large individual differences in sleep need. Of individuals in the general adult population, 97% sleep between 6 and 9 hours per day. When young adults were instructed to remain in bed for 16 hours in darkness per day for a 1-month period, their total sleep time stabilized at 8.5 h. This may represent the true sleep need. Sleeping less than 6 hours a night generally results in symptoms of sleep deprivation (see below). Interestingly, sleeping excessively may also result in non-refreshing sleep and daytime fatigue.
Thus, one cannot prepare a ‘sleep bank’ for future needs. There have been several well-publicized studies examining the limits of sleep needs, and whether these can be modified. In one such study, conducted by the US Navy, it was suggested that people who sleep regularly for 8 hours per night are able to reduce their sleep time gradually to 7 or 7.5 hours, without experiencing symptoms of sleep deprivation. This conclusion has, however, been refuted in most modern studies. It has been shown that even moderate sleep curtailment, when experienced for several days, impairs daytime alertness and performance. On the other hand, increasing sleep even from 7 to 8 hours improves quality of life as well as daytime cognitive functioning. Thus, total sleep time should be adequately assessed in the differential diagnosis of daytime sleepiness and chronic fatigue.
The first step in the approach to find out the causes of excessive sleepiness is to eliminate partial sleep deprivation as a possible cause. It should be remembered that, for some individuals, sleep need is as high as 9–10 hours a night, whereas they may sleep no more than 7 h per night. If sleepiness disappears after an adequate amount of sleep is achieved, as frequently happens at weekends, then sleepiness was most probably caused by partial sleep deprivation rather than disturbance in the sleep itself.
Several theories have been proposed concerning the function of sleep. The fact that every living creature sleeps clearly points to sleep being a necessity of life. Indeed when total sleep deprivation is experimentally induced in animals, it results in death within approximately 10 days. In humans, there is a very rare prion disease resulting in gradually increasing sleep loss which culminates in a total loss of sleep and death within a few months (fatal familial insomnia, see later). The exact function of sleep is, however, yet to be determined. Table 4 lists several theories regarding the function of sleep.
As mentioned earlier, sleep has been perceived as a period during which hypnotoxins accumulating during wakefulness are detoxified. Constantin Von Economo, the celebrated discoverer of encephalitis lethargica, postulated that sleep starts once the levels of hypnotoxins reach a critical level, which affects a specific brain centre that is susceptible to these hypnotoxins. Once this brain centre is affected, sleep spreads across the brain by pavlovian inhibition. Once detoxification of hypnotoxins is complete, sleep ends. The two-process sleep theory that relied on this assumption has put major emphasis on slow-wave sleep (SWS), as reflecting the brain process responsible for this detoxification. The fact that SWS linearly increases with the duration of previous wakefulness, and exponentially decreases during sleep, supports this position.
Table 4 The possible function of sleep
Behavioural adaptation sleep theory posits that sleep evolved in order to enforce behavioural quiescence during the dark periods, when organisms may be exposed to better equipped predators. The Benington/ Heler theory suggests that sleep fulfils energy conservation purposes. This theory is supported by the findings that during wakefulness the levels of energy in the brain decrease (ATP, glycogen, adenosine), and re-increase during sleep. During sleep itself, the energy expenditure is reduced by 15–20%, and oxygen consumption decreases.
The restorative theory suggests that sleep is a time of restoration and growth for the body and brain. The finding that sleep increases after rigorous exercise supports this theory, as does the observation that growth hormone is mainly released during sleep, especially during deep sleep. Others suggested that sleep is essential for brain processing and organizing the large amounts of input gathered during the day, in a fashion that will allow recollection and use of these data in the future. REM sleep may play a specific role in this regard (see later).
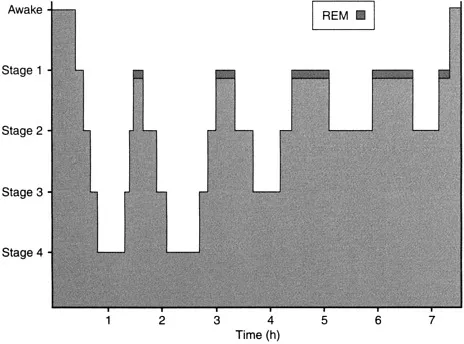
Figure 2 The characteristics of sleep architecture over a 7.5-hour sleep period.
Experimental data suggest that sleep may also be related to temperature regulation and immune defence mechanisms.
The multiplicity of sleep theories most probably indicates that sleep does not have a single function. To cite Kleitman’s now famous dictum, when asked what is the function of sleep, his response was: ‘Tell me first what is the function of wakefulness and then I will tell you what is the function of sleep.’ Most probably as yet unknown functions of sleep still await discovery.
Sleep architecture
The ultradian organization of sleep is in cycles, each of which lasts approximately 1 hour in infants and small children, and 1.5 hours in adults. Every cycle consists of various stages of sleep, usually progressing from stage 1 to 3–4 and culminating in REM sleep. The relative quantity of each of the sleep stages changes as the night progresses. Figure 2 demonstrates a typical ‘hypnogram’ over a 7.5-hour sleep period. As can be seen, the percentage of SWS is highest in the first sleep cycle, whereas most of the REM sleep is seen towards the morning. The relative part of REM sleep in each sleep cycle increases as the night progresses. Moreover, the density of eye movements in each REM sleep, which most probably reflects the intensity of activation of an endogenous REM sleep generator, also increased as the night progresses.
In reality the sleep cycles are not always complete and frequently in some cycles not all sleep stages occur. Commonly, there are short awakenings between sleep cycles, and it is also not unusual to experience some brief arousals within the sleep cycles themselves. When summarizing the relative portion of each of the sleep stages across the night (see Table 3), the following picture emerges: SWS and REM sleep each account for 20% of the total sleep time, and the rest is made up of stages 2 and 1. These percentages change with various conditions such as age (see Table 3), after sleep deprivation, stress, exercise, mood changes and various pathological conditions (see later).
REM sleep—characteristics and function
Rapid eye movement sleep is a unique state of consciousness. It was discovered by Eugene Aserinsky and Nathaniel Kleitman (1953) at the University of Chicago, and has been the subject of extensive research ever since. Its unique physiological and psychological characteristics have led investigators to call it by different names. As EEG activity during REM sleep resembles that of wakefulness it has been called desynchronized sleep, or paradoxical sleep, and because it is associated with dreaming in humans it is often called dreaming sleep. The most commonly used name, however, has remained REM sleep. Indeed the prolific rapid eye movements are the hallmark of this sleep stage. The main characteristics of REM sleep are shown in Table 5.
The confluence of physiological events during REM sleep is rather unique. First, as mentioned before, the EEG is very similar to that of wakefulness, with low-amplitude fast activity, and eye movement activity that is indistinguishable from that in wakefulness. Second, there is evidence of an increased energy expenditure by the brain. Third, in sharp contrast to brain wave and eye movement activation, skeletal muscles are atonic, which is thought to be a protective mechanism to prevent acting out dreams (as may happen in REM behavioural disorder, see Chapter 9). The eye movements probably reflect visualization of dreams, as best indicated by their absence in congenitally blind people as opposed to their presence in acquired blindness. REM sleep is also characterized by penile erection in men and vaginal blood engorgement in women, making the meaning of a ‘unique’ state become clear.
Table 5 Characteristics of REM sleep
In contrast with the non-REM sleep stages, which are characterized by parasympathetic dominance, REM sleep is associated with intense sympathetic activation. This is manifested by an increase in heart and respiratory rates, as well as in their variability, and an increase in peripheral vasoconstriction and systemic blood pressure. Furthermore, the sensitivity of the respiratory control mechanisms to hypercapnia and hypoxia in this stage is diminished, resulting in prolonged apnoeic events and profound arterial oxygen desaturation in sleep apnoea patients (see later). Penile erection, mediated by parasympathetic activation, stands out during REM sleep, on the background of sympathetic dominance. The penile erection seen in REM sleep has important clinical implications because it can distinguish between psychogenic and organic impotence. The existence of REM-related penile erection rules out organic causes of impotence.
Despite extensive research spanning almost half a century, the exact function of REM is far from being understood. Table 6 lists several theories regarding the function of REM sleep.
The main findings from studies (of animals and humans) address...
Table of contents
- Cover Page
- Title Page
- Copyright Page
- Preface
- Chapter 1: History of Sleep Medicine
- Chapter 2: Systemic Function During Normal Sleep
- Chapter 3: Hypersomnia: An Introduction
- Chapter 4: Sleep Apnoea Syndrome
- Chapter 5: Periodic Limb Movement Disorder
- Chapter 6: Primary and Other Forms of Hypersomnia
- Chapter 7: Hypersomnia: Summary and Patient Approach
- Chapter 8: Insomnia
- Chapter 9: Parasomnias
- Appendix International Classification of Sleep Disorders
- References