![]()
1 | Structure and Function of Human Skin |
1.1 Introduction
Human skin is a remarkable barrier between the body and the environment, providing protection against ingress of allergens, chemicals, and microorganisms, regulating the loss of water and nutrients from the body and responding to mitigate the effects of ultraviolet (UV) radiation. The skin has an important role in homeostasis by regulating body temperature and blood pressure and is an important sensory organ for temperature, pressure, and pain. As the largest organ of the human body, providing around 10% of the body mass and covering an area of ~1.8 m2 in the average person, this easily accessible tissue apparently offers ideal multiple sites to administer therapeutic agents for both local and systemic actions, but human skin is a highly efficient self-repairing barrier that has evolved to keep “the insides in and the outside out”.
Skin membranes can be considered at various levels of complexity. In some mathematical treatments of transdermal drug delivery (see Chapter 2), skin can be regarded as a simple physical barrier; more complexity can be introduced by viewing the different tissue layers as multiple barriers in series. Further, drug transport through skin pores provides barriers in parallel. Degrees of complexity also exist when examining basic structures and functions of the membrane. In some extreme cases, it may be that transdermal drug delivery is limited by metabolic activity within the membrane. Alternatively, immunological responses may prevent the clinical use of a formulation that has proven to be optimal during In Vitro studies. A further complication is introduced in clinical situations where topical delivery is intended to treat diseased skin states; here the barrier nature of the membrane may be compromised at the onset of therapy, and still further complexity is introduced if the skin barrier changes through repair during treatment.
This chapter describes the structure and function of healthy human skin, and considers some skin-related factors that can affect transdermal and topical (or “dermal”) drug delivery, such as body site, the overlying skin microbiome, and age-related alterations to the membrane.
1.2 Healthy Skin Structure and Function
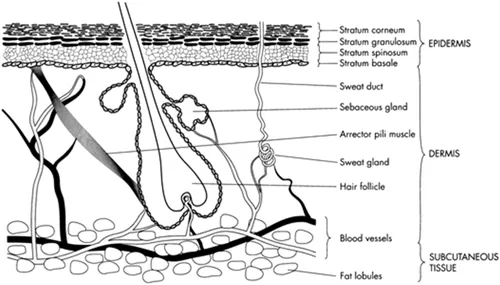
The anatomy of human skin is complex, but for the purpose of transdermal and topical drug delivery, we can examine its structure and function in four main layers: (1) the innermost subcutaneous fat layer (hypodermis), (2) the overlying dermis, (3) the viable epidermis, and (4) the outermost layer of the tissue (a non-viable epidermal layer) the stratum corneum. Nerves, blood, and lymphatic vessels pervade the hypodermis and dermis, and various appendages are supported in the dermis and pass through to the external surface: hair follicles, eccrine glands, and apocrine glands (Figure 1.1).
FIGURE 1.1 A diagrammatical cross-section through human skin. (From Williams, A.C., 2003. Transdermal and Topical Drug Delivery. London, UK: Pharmaceutical Press. With permission.)
It should be noted that, in vivo, skin is in a process of continual regeneration, is metabolically active, has immunological and histological responses to assault (as would be the case if an exogenous chemical, such as a drug, were applied to the surface), and changes due to diseased states. Due to experimental and ethical difficulties, most transdermal and topical drug delivery studies tend to use Ex Vivo (In Vitro) skin which inherently reduces some of the above complexity – regeneration stops, immune responses cease, and metabolic activity is usually lost in these studies. Thus, with In Vitro permeation studies, the skin effectively acts as a physical barrier to drug delivery but it should always be borne in mind that data obtained from excised skin may not translate directly to the in vivo situation.
1.2.1 The Subcutaneous Fat Layer
The subcutaneous fat layer, or hypodermis, is the deepest layer of the skin and houses major blood vessels and nerves. This layer is relatively thick in most areas of the body, typically in the order of several mm. However, there are other areas in which the subcutaneous fat layer is largely absent, such as the eyelids.
The hypodermis is composed of loose, fibrous connective tissue, which contains adipose tissue and fibroblasts. A principal role of the hypodermis is to anchor the skin to the underlying muscles, thus providing mechanical support for the skin. This layer also acts as an insulator, provides mechanical protection against physical shock and serves as a fat store of adipose tissue. The subcutaneous layer is seldom an important barrier to transdermal and topical drug delivery, since it sits below the dermis which contains a rich blood supply; for some regionally acting drugs – for example, those targeting joints or muscles – it is feasible that the subcutaneous layer could provide some resistance to drug delivery.
1.2.2 The Dermis
The dermis (or corium) is the major component of human skin and is typically 3–5 mm thick.
The dermis contains fibroblasts along with adipocytes, some macrophages, and mast cells, but is also heterogeneous and two layers are evident, a lower reticular and an upper papillary layer. The reticular dermis is composed of dense irregular connective tissue, predominantly densely packed collagen fibres (providing mechanical strength) alongside elastic fibres such as elastin (for flexibility) in ground substance, an amorphous gel-like matrix that contains water, glycoproteins, and glycosaminoglycans such as hyaluronan. The reticular layer supports the blood and lymphatic vessels, nerve endings, pilosebaceous units (hair follicles and sebaceous glands), and sweat glands (eccrine and apocrine). The papillary layer overlays the reticular layer and contains more loosely arranged collagen fibres. The layer is named after the dermal papillae that interconnect the dermis with the rete ridges of the epidermis. The papillae contain terminal networks of capillaries and increase the surface area between the dermis and epidermis, which increases exchange of nutrients, waste products, and oxygen between the two layers. This also promotes transdermal drug delivery by removing permeants rapidly from the dermal–epidermal boundary. The interdigitation of the dermal papillae and epidermal rete ridges provides additional “lateral” mechanical strength to skin and the pattern of the ridges determines the patterns of fingerprints. In terms of transdermal drug delivery, the dermis is often viewed as essentially gelled water, thus providing a minimal barrier to delivery of most polar drugs, although the dermal barrier may be significant when delivering highly lipophilic molecules.
The extensive vasculature in the dermis is clearly important in regulating body temperature whilst also delivering oxygen and nutrients to the tissue and removing toxins and waste products. With regard to drug delivery, the rich blood flow, around 0.05 mL/min per mg of skin, is very efficient for the removal of molecules from the dermis to maintain the driving force for diffusion. The lymphatic system also reaches to the dermal–epidermal boundary and, whilst important in regulating interstitial pressure, facilitating immunological responses to microbial assault, and for waste removal, the lymphatic vessels may also remove permeated molecules from the dermis hence maintaining a driving force for permeation. Cross and Roberts (1993) showed that whilst dermal blood flow affected the clearance of relatively small solutes, such as lidocaine, lymphatic flow was a significant determinant for the clearance of larger molecules, such as interferon.
Three main appendages found on the surface of human skin originate in the dermis; the pilosebaceous unit, eccrine glands, and apocrine glands. In terms of transdermal drug delivery, these appendages may offer a potential route by which molecules could enter the lower layers of the skin without having to traverse the intact barrier provided by the stratum corneum. These so-called “shunt routes” may have a role to play in the early time course of the permeation process, for large polar molecules, and also in electrical enhancement of transdermal drug delivery. However, for most permeants, the fractional area offered by these shunt routes is relatively small and so the predominant pathway for molecules to traverse the tissue remains across the bulk of the skin surface. The mechanisms by which molecules traverse human skin, including the influence of shunt route transport, are discussed in Chapter 2 (see Section 2.3).
1.2.2.1 Pilosebaceous Unit
The pilosebaceous unit consists of the hair follicle, the hair shaft, the adjoining arrector pili muscle, and the associated sebaceous gland. As the unit traverses the intact stratum corneum and epidermis, the role of the follicular pore in drug delivery has been investigated. However, as the unit is also associated with skin conditions such as acne vulgaris, folliculitis, and alopecia, the pilosebaceous unit is also a target for locally acting therapeutic agents.
The hair shaft is composed of an inner medulla overlaid with a cortex and then a cuticle. The root sheath has various layers but the outer root sheath is a keratinised layer that is continuous with the epidermis and is therefore of greatest importance with regard to drug diffusion and delivery. The hair follicle can be divided into several regions starting from the skin surface. The infundibulum is the outer part of the hair follicle and extends down to the sebaceous duct. In this area, the hair shaft is not in intimate contact with the skin and can move relatively freely. Due to the loss of epidermal differentiation, the thickness of the stratum corneum decreases deeper in the infundibulum, which results in a lesser barrier to drug diffusion compared to the stratum corneum at the skin surface.
Each hair follicle is associated with one or more sebaceous glands, outgrowths of epithelial cells, and composed of lipid-producing sebocytes lining sebaceous ducts. Non-hair bearing sites including the mouth, the eyelids, the nipples, and the genitals also have sebaceous glands. The greatest density of these glands is on the face and scalp; only the palms and soles, which also have no hair follicles, are completely devoid of sebaceous glands. The glands release lipids through holocrine secretion, and human sebum reaching the surface of the skin consists of a mixture of lipids including cholesterol, squalene, triglycerides, and free fatty acids. Sebum helps to maintain hydration and pliability of the skin’s surface and provides a skin surface pH of about 5.5 which inhibits bacterial and fungal growth.
1.2.2.2 Eccrine (Sweat) Glands
The eccrine glands are simple coiled glands, 500–700 µm in diameter, located in the lower dermis. Found over most of the body surface, typically at a density of 100–200 per cm2 of skin, eccrine glands secrete a dilute salt solution at a pH of about 5 onto the skin surface and so also confer some antimicrobial properties. Sweat secretion is stimulated by temperature-controlling determinants, such as exercise and high environmental temperature, as well as emotional stress through the autonomic (sympathetic) nervous system. Typical eccrine duct diameters are 30–40 µm.
1.2.2.3 Apocrine Glands
The apocrine glands are limited to specific areas of the skin including the axillae, nipples, and anogenital regions. The apocrine gland coil is similar in size to an eccrine gland (~800 µm in diameter), but with a significantly greater duct diameter (80–100 µm). Apocrine gland ducts secrete into the upper regions of the hair follicle, and their lipoidal and “milk” protein secretions provide nutrients for skin bacteria; bacterial decomposition of the secretions is primarily responsible for imparting the odour of sweat.
1.2.3 The Epidermis
Overlying the dermis, the epidermis is a complex multiply layered membrane which varies in thickness from around 0.06 mm on the eyelids to around 0.8 mm on the load-bearing palms and soles of the feet. The epidermis contains five histologically distinct layers, which, from the inside to the outside, are the stratum basale (also called the stratum germinativum, or simply the basal layer), stratum spinosum, stratum granulosum, stratum lucidum, and the stratum corneum (Figure 1.2). The stratum corneum, comprising anucleate (dead) cells, provides the main barrier to transdermal delivery of drugs and hence is often treated as a separate membrane by workers within the field. The term “viable epidermis” is often used to describe the underlying four distinct layers, although the viability of cells within, for example, the stratum granulosum is questionable, as the cell components degrade during differentiation.
FIGURE 1.2 Diagrammatical representation of the epidermal layers and their differentiation. (From Williams, A.C., 2003. Transdermal and Topical Drug Delivery. London, UK: Pharmaceutical Press. With permission.)
1.2.3.1 Basement Membrane
The basement membrane delineates the dermis from the epidermis and, in essence, is the dermal–epider...