![]()
1
Ritva Laaksonen and Mervi Ranta
Introduction
Neuropsychotherapy is a form of treatment based on recent advances in the domains of neuroscience, neuropsychological rehabilitation, and models of psychotherapy. It can be considered an alliance between scientific, theoretical and clinical knowledge in these areas (Laaksonen, 2007).
The term neuropsychotherapy has been used in different conceptualizations. In the context of this book, we follow the contextualization indicating that neuropsychotherapy is a name for interventions, which we need for people who suffer from emotional, behavioral, or personality disorders after neurological dysfunction or syndromes. Remediation of cognitive disturbances will also be included in the treatment process. The term neuropsychotherapy has also been used when neuroscientific knowledge has been integrated into psychotherapy (Grawe, 2007), or neuropsychoanalysis (Kaplan-Solms & Solms, 2000).
The concept and procedures are multidisciplinary in nature. The patient groups concerned vary within different types of central nervous system (CNS) involvement. The metatheory for guideline information in the therapeutic remediation procedure needs to be multifarious and must cover several domains of knowledge to serve as a guideline for rehabilitation in practical and ecologically valid settings.
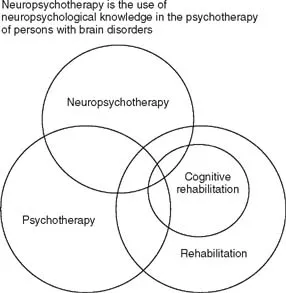
Figure 1.1 What Is Neuropsychotherapy?
Even though psychotherapy is now, according to Coetzer (2007), an approach used within several models of neurorehabilitation, a core theoretical model to guide psychotherapeutic practice is lacking. The aim of this chapter is to open a scope of applicable conceptualizations for further developments in the field of comprehensive, integrated rehabilitation procedures. Judd (1999) has conceptualized the overlap of various forms of rehabilitation of people with brain injuries. His illustration is seen in Figure 1.1.
The overlapping use of knowledge from different cases of people with brain injuries has proved necessary if suitable and efficient treatment procedures are to be designed.
Neuropsychological Rehabilitation and Psychotherapy: Historical Perspectives
Fractured minds (Ogden, 2005), shattered worlds, and grief reactions are not unfamiliar to clinical psychologists, nor to neuropsychologists. Historically, however, psychotherapy has not been considered useful in the rehabilitation of brain-dysfunctional patients (Prigatano, 1991). It has been viewed as having little application in a brain-injured population in the past (Coetzer, 2007), despite the phenomenological necessity.
It should be kept in mind that this doesn't mean that the clinical professionals working in the field would have neglected the injured person's emotions or personality as a whole. What it means is that the writings and explicit ways of describing the interventions have oft en focused on remediation of cognitive functions. In the tacit level, the importance of social adjustment, individuality, and interpersonal problems have been acknowledged and worked at in real life situations by experienced professionals. There are published examples of this line of thinking, for instance, in treating cerebrovascular patients, as early as the 1970s. A historical example of treating post-stroke depression with psychological management is given by Horenstein (1970). His suggestion is a stepwise psychological approach involving structured teamwork and family participation rather than medication. Horenstein points out that depression of mood frequently accompanies isolated and multifocal cerebral vascular lesions as grief which resembles that observed after other major illness. He associates the occurrence and severity of depression also with the person's previous ability for adaptation and other premorbid factors (i.e., personality, self-esteem, intelligence, and experience). The life situation and family support are likewise important in psychosocial recovery. Since family members will also have to go through a process of grief and adaptation, it is important to include them in the comprehensive treatment procedure. Neuropsychological recognition of the deficit and appreciation of its significance in the altered state and life situation are present in depressive reactions of the patient. Knowledge of the patient's premorbid ways of reacting to illness, injury, or bereavement, as well as personality traits, may help in predicting the type and length of depression and adjustment to changes after illness. As one example of slow adjustment, Horenstein mentions premorbid obsessive–compulsive traits, which make the person apt to hostility and blaming others for his anger and disappointment in recovery (Horenstein, 1970).
In Finnish neuropsychology, the pioneer Niilo Mäki (1902–1968) treated war veterans using a holistic orientation. He was well acquainted with the work of Ahhemar Gelb and Kurt Goldstein (Laaksonen, 1987). For Niilo Maki, the whole person was important. This outlook sets more holistic goals for neuropsychologists and improves the methods of treatment interventions. Niilo Mäki's work did not have a direct continuation in civilian hospitals in Finland, but the spirit did continue (Laaksonen, 1987).
In Finnish civilian hospitals, neuropsychological rehabilitation had its roots in the late 1960s. Originally, the focus was in cognitive remediation based on the works and writings of A. R. Luria (Laaksonen, 1987). Later, quality of life was explicitly added to the goals of neuropsychological rehabilitation (Laaksonen, 1994). The core idea of Luria's tradition was that theory and methods of treatment should be continually tested. The theoretical framework included the dynamic, systemic theory of higher cortical functions in relation to localized lesions, which caused specific disturbances with different mechanisms responsible for the neuropsychological sequelae after injury. Restoration of function was to be built on careful analysis of the syndromes and constellation of disturbed functions, with distinction of primary and secondary mechanisms responsible for the disturbance. Thus, the methods of reeducation, or restoration of function, could become specific training programs aimed at reorganization of function. In some disturbed functions, direct rehearsal could also be used (Luria, 1963, 1970, 1973). Luria's theory was the source of inspiration for Finnish neuropsychologists, and continues to be so, as advances in the field build upon it.
Anne-Lise Christensen's work in Denmark has served as a model in the Luria tradition and the holistic approach, and her influence is still strong, as well. In recent writing, she points out that in qualifying the inner structure of psychological processes the method gives insight into the syndromes of difficulties of the patient. This further provides possibilities for the neuropsychologist to initiate feedback process that can be closely linked to the planning of the most effective rehabilitation of the patient's cognitive, social and behavioral way of functioning and thus create strong and valuable connection between diagnosis and treatment experiences (Christensen, 2009). Christiansen's work can function as an important guideline for psychoeducation of treatment methodology, together with updated knowledge about neuroplasticity and functioning of neural networks. The psychotherapeutic aspect must also be interwoven into a comprehensive treatment procedure. This has previously been understood by professionals in the field as a need for double training (i.e., requiring postgraduate studies in both neuropsychology and psychotherapy).
This holistic interest was also reflected in the need for studies on quality of life as early as the 1980s, even though the increased interest and the majority of studies emerged later. One of the early studies on quality of life after vascular brain injury was published by Niemi, Laaksonen, Kotila, & Waltimo (1988). The most important finding indicated that subjective tendency to get depressed was the most important variable that correlated with the deteriorated quality of life four years post-stroke. Another follow-up study with TBI-patients (Koskinen, 1998) indicated that neurobehavioral and emotional disturbances had the most significant effect on strain felt by relatives and on the quality of life of the injured 10 years post-injury. In a multicentered European study, a questionnaire (EBIQ) was created to better understand the subjective experience of cognitive, emotional, and social difficulties of brain-injured patients and their close relatives (Teasdale et al., 1997).
Depression after stroke has been of interest for many years, as we discussed earlier. The prevalence of post-stroke depression and depression of the caregivers has been studied more recently by Berg and collaborators (2001, 2003, and 2005), whose studies indicate the need for therapeutic attention. According to Berg and collaborators, about 50% of stroke patients suffer from depressive symptoms two months after the onset of stroke. The authors point out that depression has a negative effect for prognosis of recovery and quality of life. At the postacute stage, men seem to suffer from depression more oft en than do women. Spouses also showed marked signs of depression.
Despite individual pioneering articles and literature indicating the need for a more comprehensive approach, the research on cognitive neurorehabilitation, or reeducation to overcome the hampering neuropsychological deficits, continued to be overemphasized. This eventually led to a misunderstanding of the importance of only treating cognitive deficits with cognitive exercises.
Experiences in the practice of neuropsychological rehabilitation during the past three decades have finally allowed for the questioning of the emphasis on purely cognitive retraining in treating people with brain injuries. A welcomed critique for purely cognitive treatment has come from Sohlberg, and Mateer (2001), who state about neuropsychological rehabilitation: “The term cognitive rehabilitation was perhaps always too narrow, and focused too heavily on remediating, or compensation for decreased cognitive abilities… . The last 25 years have allowed a richer appreciation for the influence of contextual variables; the personal, emotional, and social impacts of brain injury; and their interactions with cognitive function. All of these factors have been incorporated to an even greater degree into treatment plans and goals” (Sohlberg and Mateer, 2001, p. 1).
Integration of Psychotherapy in the Treatment Models of TBI and ABI Patients
At the turn of the century, we have finally arrived at explicit efforts to integrate psychotherapeutic models and methods with neuropsychological rehabilitation. The term neuropsychotherapy has also emerged, with different conceptual connotations. The reference list directly under this term is still very short. However, the list of articles including cognitive–behavioral, or other theoretical models of psychotherapy needed in treating the brain-injured population, is much longer. In her pioneering work beginning in the 1980s, Barbara A. Wilson used the behavior therapy approach together with neuropsychological knowledge in treating brain-dysfunctional patients (Wilson & Moffat, 1984; Wilson, 1999; Wilson, Herbert, & Shiel, 2003).
One of the landmark studies penetrating the subtleties of the interpersonal process with brain-injury survivors was published by Judd and Wilson (2005). They identified the combination of educational and cognitive strategies that was most effective in addressing the challenges encountered in working with the distress of patients. The aim of therapy in their study was to help a troubled individual reduce his or her distress and enjoy greater life satisfaction through changing the patient's thoughts, feelings, and behavior. They made the argument that psychotherapy is a relational process, regardless of theoretical orientation, in which both the therapist and the client co-constitute and actively participate in the therapeutic encounter. They emphasized the quality of the therapeutic relationship as a key factor. The therapeutic alliance is the core element in this interpersonal process. In clinical practice, we can see the complex interplay between psychological and organic damage. The sequelae after brain injury can be most varying and subtle. It is of utmost importance for the therapist to understand the nature and severity of the brain damage, as well as the meaning the survivor gives to the personal experiences, postinjury identity, and the psychosocial consequences. For a successful outcome, we need to see the person as a unique human being, with deficits and strengths that challenge the therapist to engage in a mutual and sometimes lengthy arduous process of treatment collaboration. The therapeutic alliance has been a theme in a few outcome studies in neurological population. Schönberger and collaborators found correlations with the efficacy of neuropsychological rehabilitation outcomes and the therapeutic alliance, together with patient compliance with psychosocial measures like going back to work and also cognitive functioning in postacute brain injury rehabilitation (Schönberger, Humle, & Teasdale, 2006, and 2007). Sche...