eBook - ePub
Measurement of Cardiac Function
Approaches, Techniques, and Troubleshooting
This is a test
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Book details
Book preview
Table of contents
Citations
About This Book
This book presents detailed descriptions of how to set up and use several classical cardiac preparations from scratch, including whole heart, atrial, ventricular, and papillary muscles and in vivo small animal preparations. It describes methods for monitoring contraction and contractility.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Measurement of Cardiac Function by John H. McNeill in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Theory, Practice & Reference. We have over one million books available in our catalogue for you to explore.
Information
Chapter | 1 |
The Langendorff Heart | |
Contents
1. Introduction
2. Applications
3. Methods
3.1. The Langendorff Apparatus
3.2. Buffers
3.3. Preparation of the Heart
3.4. Measurement of Cardiac Performance
4. Potential Problems
4.1. Inadequate Heparinization
4.2. Air Bubble Accumulation
4.3. Quality of Perfusion Buffer
4.4. Experimental Variations
References
1. Introduction
The Langendorff heart preparation is one of the earliest models of an isolated organ, used by physiologists and pharmacologists to investigate function and the effect of different agents on an isolated tissue. This preparation was first described by O. Langendorff in 1895.1 The procedure is based on perfusing an isolated heart through the aorta (retrograde) with an oxygenated physiological buffer. The resulting retrograde perfusion pressure closes the aortic valve, facilitating the perfusion of the coronary blood vessels located at the base of the aorta. As the heart is a highly vascularized organ, the physiological buffer eventually gains access to all cells within the heart. Since the heart requires a steady supply of oxygen and metabolic energy for its normal functioning, it is crucial to rapidly extract the organ from the chest cavity without an episode of ischemia, prevent occlusion of the coronary arteries with blood clots, and rapidly supply the organ with a highly oxygenated physiological buffer.
Through a century of utilization of the Langendorff heart, there have been numerous modifications of the original Langendorff apparatus, an evolution which was inevitable as advances in technology enhanced our ability to build better and more reliable devices. In this chapter, the basic principles and methods required for preparing a reliable Langendorff heart are described.
2. Applications
Considering that ventricular muscle is highly vascularized, inotropic agents perfused into the heart rapidly gain access to all ventricular muscle cells, leading to a greater sensitivity of the preparation to perfused agents. Hence, the Langendorff heart preparation is ideal for studying the concentrationdependent effects of positive and negative inotropic agents on cardiac contractility.2 Agents that increase the force of ventricular muscle contraction (positive inotropic agents) increase intraventricular pressure and the contractility index +dP/dtmax, while agents that reduce the force of contraction (negative inotropic agents) reduce intraventricular pressure and +dP/dtmax. An example of the effect of such agents on the guinea pig heart is shown in Figure 1.3 Additionally, as some inotropic agents alter heart rate and coronary flow, the Langendorff heart preparation described here eliminates limitations induced by these factors. For example, as negative inotropic agents reduce ventricular function, aortic perfusion pressure is diminished, leading to cessation of coronary flow and heart failure due to ischemia. In the Langendorff heart, coronary perfusion pressure and coronary flow are independent of ventricular muscle function. This is in contrast to the working heart model, where aortic perfusion pressure is dependent on left ventricular function.4 Finally, a fixed balloon size in the present preparation ensures measurement of isometric tension at an optimal muscle fiber length.
In addition to the above-described physiological and pharmacological measurements, the Langendorff heart preparation has also been widely used in the study of metabolic changes brought about by ventricular contraction and relaxation.5 Additionally, the effect of ischemia and hypoxia on cardiac metabolism and function has also been studied using the Langendorff isolated heart.6,7 The preparation could also be utilized for evaluating the effect of different agents which act on coronary blood vessels. For this purpose, the heart is perfused under a constant pressure from a buffer reservoir placed at a constant height above the heart, and coronary flow is monitored by measuring buffer flow rate through the heart.8 Alternatively, the heart is perfused with buffer at a constant flow rate and aortic perfusion pressure is used as an index of constriction or dilatation of coronary blood vessels.9
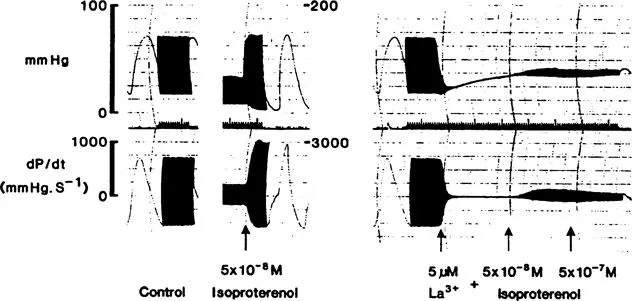
Effect of isoproterenol and lanthanum on contractility of the guinea pig heart. The figure shows original tracings of a Langendorff preparation of an adult guinea pig heart perfused with Hepes buffer containing 1.8 mM calcium. The upper part of the tracing shows intraventricular pressure of the left ventricle and the bottom part shows the first derivative of the pressure curve (dP/dt) recorded simultaneously. Following 45 min equilibration with Hepes buffer, the heart was perfused with the maximum effective concentration of isoproterenol (5 x 10-8 M). Note that sensitivity of the recording was altered to fully record the increase in intraventricular pressure and dP/dt induced by isoproterenol treatment. Isoproterenol was rapidly washed out and perfusion was continued with Hepes buffer for 45 min. Following washout with buffer, basal contractility returned to its initial control level. The heart was then perfused with 5 μM lanthanum followed by the same concentration of lanthanum plus 5 x 10-8 and 5 x 10-7 M isoproterenol. (From Fawzi, A.B. and McNeill, J.H., Can. J. Physiol. Pharmacol., 63, 1106, 1985. With permission.)
3. Methods
3.1. The Langendorff Apparatus
The key elements for successful operation of a Langendorff heart are (a) uniform flow of buffer at a constant pressure; (b) constant temperature of the perfused buffer; and (c) continous oxygenation of the buffer. Figure 2 shows the basic design of the apparatus. To supply buffer to the heart, one can simply place the buffer container at a height to provide a 60 mm Hg pressure to the base of the aorta. An alternative method is to use a peristaltic pump (Pharmacia Biotech Pump P-1) such that buffer flow is adjusted to provide the desired perfusion pressure (8 to 9 ml/min). Buffer should reach the heart at a constant temperature ranging from 30 to 37°C (Proportional Temperature Controller YSI Model 72; Fisher Scientific). Some investigators prefer perfusing the heart at 37°C. However, a lower temperature of 30°C allows for a longer operation of the heart with a consistent heart function. A constant temperature is achieved by passing the buffer through a jacketed water bath (diameter 7 cm; height 17 cm) just before it enters the heart. The temperature is set at around 2°C higher than the desired temperature, which is measured by placing a thermometer at the end of the aortic cannula. The buffer should be aerated continuously with 95% O2 to 5% CO2. To avoid the transmission of air bubbles into the coronary blood vessels, a bubble trap should be placed above the heart. Hence, buffer leaving the jacketed coil flows into the bubble trap before reaching the heart. The trap is connected to a pressure transducer to monitor perfusion pressure of the buffer before it enters the heart. It also contains a release valve to release excess air bubbles in the trap.
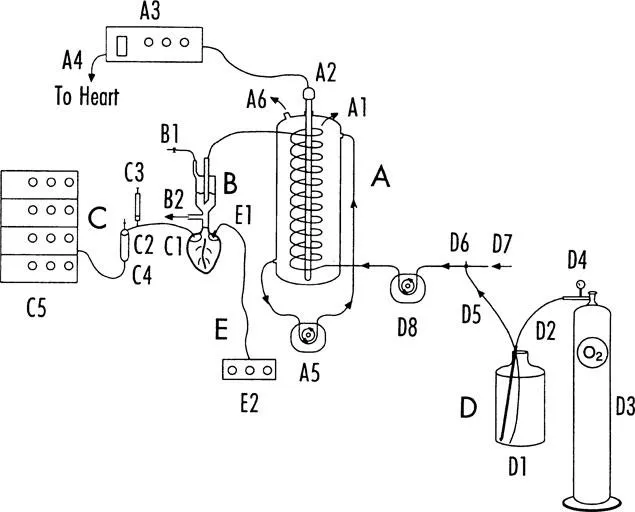
The figure shows a schematic model of the Langendorff apparatus. The major parts of the apparatus are labeled alphabetically, whereas components are marked with an alphabet letter followed by a number. A. Jacketed glass water bath. Buffer is pumped into the bath through a coiled glass tube (A1). A porcelain heating element (A2) is placed in the center of the bath to maintain the water in the bath at the desired temperature. The heating element is connected to a regulated proportional power supply (A3). Amount of power supplied to the heating element is determined by the set point on the power supply and the feedback obtained from temperature of the heart detected by a flexible temperature probe (A4). The probe can either be placed inside the right atrium or water bath (via inlet A6). To ensure an even temperature throughout the bath, distilled water inside the bath is circulated by a peristaltic pump (A5). A large volume of water in the bath (500 to 700 ml) is required to prevent temperature fluctuations. B. Air bubble trap. This device, made of glass, plays a crucial role in preventing air bubbles from entering the heart. It is supplied with two outlets: B1, connected to a Tygon tube and a two-way valve to release excess air and regulate buffer level in the trap, and B2, which is connected to a pressure transducer for monitoring buffer pressure. C. Latex balloon. The balloon, which is inserted into the heart, is connected to the end of a polyethylene tube (C1) attached to a three-way valve (C2), a 2-ml syringe (C3), a pressure transducer (C4), and polygraph (C5). D. Physiological buffer and peristaltic pump. Buffer is placed in a suitable container (D1) and is continuously supplied with 95% CO2/5%O2 through an aerator (D2) connected to gas tank (D3) and a regulator (D4). Buffer is drawn from the container through a Tygon tube (D5) connected to a three-way valve (D6). The valve is connected to a second Tygon tube (D7) for perfusion of buffer containing the test compound. A regulated peristaltic pump (D8) is used to pump the buffer to the heart through the jacketed bath. E. Stimulator and electrode. The heart is stimulated at double its threshold voltage through platinum electrodes (E1) placed on the surface of the right atria. Pulse stimulation is provided by a stimulator (E2).
For monitoring ventricular pressure, some investigators insert a needle connected to a pressure transducer (GRASS Instruments) into the base of the left ventricle. To monitor isometric tension developed by the left ventricle, a small latex balloon filled with saline and connected to a pressure transducer is inserted into the left ventricle via a small incision made in the left atrium. The balloon is made from thin latex material such as the tip of a nonlubricated condom. The balloon is connected to a 1- or 2-ml syringe filled with saline to adjust its size. The balloon is deflated prior to insertion into the left ventricle. Following careful insertion, the balloon is gradually inflated with saline so that it fills the left ventricular cavity. In this manner, the left ventricle is stretche...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Dedication
- Preface
- The Editor
- Contributors
- Contributors
- Table of Contents
- Chapter 1. The Langendorff Heart
- Chapter 2. The Working Rat Heart Preparation
- Chapter 3. Isolated Papillary Muscle Preparation
- Chapter 4. Isolated Atrial Preparations
- Chapter 5. In Vivo Cardiac Measurements in the Conscious Rat
- Chapter 6. The Isolated, Coronary-Perfused, Right Ventricular Wall Preparation
- Index