![]()
Chapter 1
The Rise of Third-Party Payors: Functional and Systemic Impacts
WHAT IS MANAGED CARE?
A good way to start the process of working effectively within the managed care system is by seeking to understand that system as well as possible. Understanding can begin by answering the question, “What is managed care?” In one regard this entire book concerns itself with answering that question. Depending on the perspective from which it is observed, managed care can be seen as a redefinition of behavioral health care on functional, systemic, conceptual, and operational levels. It is
1. Functionally, a mechanism for increasing accountability and cost containment.
2. Systemically, a business and financial revolution, based on a shift in the financing of behavioral health care.
3. Conceptually, a series of conceptual shifts in the provision of behavioral health care.
4. Operationally, a sweeping revision of the processes of providing behavioral health care.
This chapter addresses the first two of these perspectives. Chapters 2 and 3 discuss the third perspective, regarding conceptual shifts, by looking at 11 concepts that redefine the provision of behavioral health care.
The fourth perspective, which addresses the operational redefinition and speaks to managed care-driven changes in how behavioral health care is provided, constitutes the focus of the rest of this book. I will discuss those changes in the provision of care in terms of both operational and clinical pathways.
Managed Care Is a Mechanism for Increasing Accountability and Cost Containment
In other words, managed care is a mechanism for containing costs by restricting the following:
1. Who will be paid to provide care. This is determined by networks of clinics staffed by in-house clinicians hired by health maintenance organizations or by networks of preferred providers, who subcontract to preferred provider organizations and agree to
a. Accept a specific (usually reduced) fee.
b. Accept clinical management.
2. What care will be provided. This is determined by
a. Requiring preauthorization for payment.
b. Requiring clinical justification before authorization is given.
Both 1b (accept clinical management) and 2b (clinical justification required before treatment or payment authorization) constitute the mechanisms by which therapist accountability is achieved. The importance of all of this can best be understood by contrasting it with the predominant payment mechanism that preceded it in the marketplace: indemnity insurance. Most clinicians fondly remember that indemnity insurance was used by the large insurance plans under which many patients were covered during most of the 1980s. Those plans usually provided for payment of 80% of the charges (up to certain maximums) to any licensed therapist for nearly any treatment of a covered diagnosis as long as the total charges did not exceed the maximum in the patient’s benefit contract. There was essentially no management of the benefit.
Managed Care Is a Business and Financial Revolution
The second part of the definition of managed care is that it is a business and financial revolution in the field of behavioral health care. As noted in the introduction (and in daily newspapers as this book goes to print) managed care is using its position as financier of behavioral health care to restructure behavioral health care along corporate business lines.
Although the broad outlines of this shift to managed care are now well known, I believe that the context of this book can benefit from a reexamination of the details and implications of that shift. Let us look at the changes from approximately 1987 to 1997. In the late 1980s chemical dependency treatment was nearly exclusively centered around 45-day in-patient programs with rare aftercare extensions. Only a few formal quality control programs existed. And only fragmentary efforts to diversify treatment service products or to provide truly differentiated levels of care were apparent. Inpatient mental health care was often isolated from outpatient care and frequently exhausted the patient’s benefits. In many cases it was extremely expensive; yet recidivism was rampant. These high costs with sometimes marginal benefits were the original impetus for the development of managed care as a cost-containment mechanism. Now, whenever behavioral heath care costs are thought to be too high, managed care is nearly always seen as the solution.
Outpatient care in the early 1980s could be described as a trade or a craft as opposed to a business in the modern sense. Frequently practitioners worked part time, with little or no consultation. Bookkeeping was limited to insurance billing and IRS requirements. Little attention was devoted to such things as profit versus loss, niches, levels of care, or cost containment. Although many therapists worked hard to provide a high quality of care, and some would argue that more quality existed in the overall system than has been apparent so far in managed care, there were few efforts to institute widespread quality measurement or continuous quality improvement programs.
Under managed care this picture is rapidly being replaced by one in which behavioral health care is emerging as a major business segment of the multibillion dollar health care industry—and a segment that is increasingly recognized as having a major part to play in health care costs—because of its effect on such issues as acuity of medical health (medical offsets), psychosomatic-oriented primary practice physicians’ visits, and compliance.
The shift to managed behavioral health care is being forcefully driven by the decision of third-party payors (primarily corporate benefits departments and insurance companies) to use their purchasing power actively and thoughtfully. With their indemnity products, insurance companies exerted little management over expenses, essentially providing unquestioned reimbursement for most therapists’ bills that fell within reasonable guidelines. The insurance companies’ decision to exert far more control (through management) brought to behavioral health care the large and ever-quickening task of shifting into a business orientation.
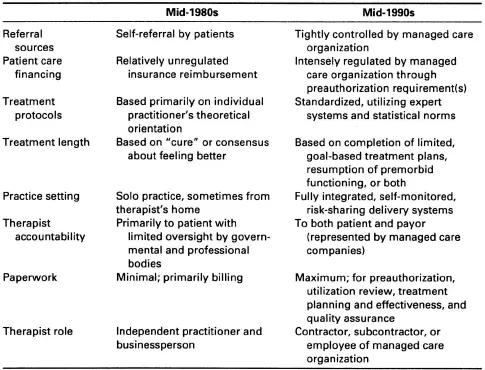
If one looks at where the behavioral health care field has been and where managed care (as well as other forces such as national health care) has been taking it, some revolutionary shifts begin to emerge. A few of those include (see also Table 1–1):
1. Patient referral sources have moved from self-referral to tightly controlled managed care company referral.
2. Patient care financing has shifted from a combination of private pay and unregulated insurance reimbursement to primarily preferred provider managed care, which promises to evolve further in the near future to include increasing numbers of therapist risk-sharing contracts.
3. Treatment protocols that were previously based primarily on the individual practitioner’s theoretical orientation are increasingly becoming standardized, based on expert systems and outliers (see chapter 7).
4. The basis of treatment length is shifting from a concept of “cure” or consensus on “feeling better” to one of limited, goal-based treatment plans (see chapters 6 and 7).
5. Therapists are moving from solo practice into large (sometimes even regional), fully integrated, self-monitoring systems of care that offer shared-risk, defined-risk, and even performance-based financing options within tight financial, managerial, and treatment constraints.
6. Accountability is becoming a buzzword as therapists are increasingly required to prove themselves. As the average treatment length is reduced, managed care companies need fewer providers. They are culling their lists through profiling (monitoring) their providers and then using only the most efficient and effective.
7. Substantially increased amounts of paperwork are becoming a part of managed care providers’ practices, as therapists are being asked to provide the raw data for utilization review, quality assurance, financial and legal reviews, customer satisfaction surveys, and treatment effectiveness studies.
Table 1–1 The Industrialization of Behavioral Health Care
8. Therapists are becoming the customer-contact agents in large, aggressive, market-oriented managed care organizations, which are constantly merging, expanding, cutting staff, and reinventing themselves in order to reposition effectively for survival in a marketplace that is growing more and more competitive. This means that therapists are being asked to maintain a customer-friendly attitude while adjusting efficiently to numerous changes in forms, financing, and management personnel. Although therapists are trained to be flexible in working with clients, sometimes these tasks can stretch their capabilities.
Some observers have used the terms “industrialization” or “commodification” to describe the changes that have begun to occur throughout health care, including behavioral health. If units of care can be somewhat standardized so that a certain number of encounters (visits of any kind) can be expected for a given episode of care, then this can be packaged as a service product that can more easily be bought, sold, built into business plans, insured, or otherwise negotiated in the marketplace. Observing this shift, many therapists feel that care is too frequently deemphasized in favor of management in managed care. Others note that the widespread availability of behavioral health care would no longer exist if managed care had not reigned in the large cost escalations of the 1980s. In this book, I want to acknowledge the fact that a large part of behavioral health care is financed and delivered through managed care and to help the reader find ethical, effective ways to provide service within that context. I will defer to other thoughtful and concerned writers who are beginning to generate a growing body of literature and comment regarding the values and ethics associated with the changes managed care has brought to the field.
CONCLUSION
This chapter cites four perspectives to begin to explain managed behavioral health care: functional, systemic, conceptual, and operational. Managed care functions as a mechanism for increasing accountability and cost containment and represents a systemic change in behavioral health care delivery based on a shift in financing. With the relatively simple shift to payment only for preauthorized care, managed care companies have restructured the entire behavioral health care field into a major business segment of the multibillion dollar health care industry. The next two chapters review the concepts that have enabled managed care organizations to implement this dramatic restructuring.
![]()
Chapter 2
The Defining Concepts of Managed Care: Set I
CONCEPTUAL SHIFTS IN THE PROVISION OF BEHAVIORAL HEALTH CARE
The third element of the definition of managed care is that it constitutes a series of conceptual shifts in the provision of behavioral health care. This chapter and the next one will discuss 11 concepts that, together, form a conceptual framework for understanding managed care and operating well within it. They emerge out of the history and the rationale for managed care. And because both the rationale and the scope of business are constantly building, these concepts are growing apace. The 11 concepts are as follows:
1. Treatment to functioning restoration.
2. Substance abuse sensitivity.
3. Actuarial-based financing.
4. Continuous quality improvement.
5. Utilization management.
6. Medical necessity.
7. Symptom-based treatment.
8. Appropriate level of care.
9. Brief therapy.
10. Clinically integrated paperwork.
11. Provider efficiency.
This chapter covers the first six of the above concepts, which emerge from common historical and functional roots. The functional and historical context of each concept will be discussed, so that its rationale can be better understood.
Managed care emerged from two forces in the marketplace: employee assistance programs (EAPs) and medical insurance programs. Current EAPs grew out of alcoholism programs. Soon after the formation of Alcoholics Anonymous a few top executives of major corporations around the United States began to sponsor alcoholism awareness and abatement programs in their company based on their own substantially increased productivity. These work-based programs were usually run by recovering alcoholics who focused on work-based functioning or lack of it (such as absenteeism) to break through the denial of alcoholics, and then helped those employees to obtain the most appropriate treatment by acting as a care intermediary. By focusing o...