eBook - ePub
Mechanics of Human Joints
Physiology: Pathophysiology, and Treatment
This is a test
- 480 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Mechanics of Human Joints
Physiology: Pathophysiology, and Treatment
Book details
Book preview
Table of contents
Citations
About This Book
This reference work brings together the biology, mechanics, neurophysiology and pathophysiology of diseased joints, illustrates available physiologically-based treatments for osteoarthrosis and explains how and when to use them.;Highlighting the most up-to-date biomechanical principles, Mechanics of Human Joints: discusses the functional anatomy of joints; relates the neurophysiology of joints to ligamentous reconstruction; elucidates the pathophysiology of osteoarthrosis; summarizes the latest information on muscle physiology and electromyography; examines the effect of vibration and impulsive loading on joint pathology; and explicates the principles of prosthetic joint replacement.
Frequently asked questions
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes, you can access Mechanics of Human Joints by Verna Wright, Eric L. Radin, Verna Wright, Eric L. Radin in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Theory, Practice & Reference. We have over one million books available in our catalogue for you to explore.
Information
I
Physiology of Joints
1
Biology of Joints
University of Washington
Seattle, Washington
Seattle, Washington
I. Introduction
The musculoskeletal system comprises a family of related tissues that interact with each other to perform work and also serve to support and protect the other organ systems of the body. The functional demands of normal human activities impose a broad spectrum of mechanical problems. In response, each articulation has evolved its own unique arrangement of bones, muscles, ligaments, and associated connective tissues. Each design serves to maximize efficient use of energy, to distribute loading forces, and to provide local stability. All are invested by the integument, supplied by the circulation, and directed by the nervous system. Together these assorted parts comprise a whole that can grow, repair, and renew itself over a lifetime while achieving a remarkable range of tasks.
II. Classification of Joints
A. Synarthroses
Human joints permit motion to occur between adjacent bones (1,2). The nature of this motion relates strongly to the nature of the joint. When motion is glacial, as it is between components of the growing skull, interlocking bones form highly stable suture lines. These joints “sew” together the adjacent bones through joints classified as synarthroses to provide a sturdy helmet around the soft and otherwise vulnerable brain. Here, the principal role of the musculoskeletal system is protective, and motion is significant only to meet the needs of growth over months and years.
The capacity for growth that these joints display is also inherent in more mobile articulations. Thus, the fibrous intervertebral joints progressively increase in diameter throughout the period of skeletal maturation. So, too, do the elbows, the wrists, the hips, the knees, and the many other synovial joints to be considered later. The process of growth in these locations has been little studied, presumably because of the more obvious and more substantial growth at epiphyseal plates and beneath the periosteum. Articular growth is not insignificant, however. A better understanding of this process might help to clarify the capacity for reshaping and remodeling that one sometimes sees and often desires in the anagement of chronically arthritic joints.
B. Amphiarthroses
Fibrous joints, or amphiarthroses, are the second major type of union between adjacent bones. These joints meet a different functional need. They provide a measure of flexibility by bending under load, much as a tree bends in the wind. The interposition of fibrocartilage between the ribs and sternum provides an extremely stable union that readily accommodates the relatively minor stresses of normal respiratory excursions. Perhaps more importantly, they can also adapt to much greater stress when the ribs are spring-loaded by external impact. The motion permitted here may provide a “safety valve” that mitigates against fracture by facilitating energy storage in elastic bone.
A similar role seems likely for the fibrocartilage found in the public symphysis and in the lower two-thirds of the sacroiliac joints. As in the chest wall, these fibrous joints provide a highly stable bond but also confer a protective measure of flexibility. In the special case of childbearing, the pelvic joints are capable of expanding to increase the diameter of the birth canal. This capability is thought to be caused by a pregnancy hormone, relax in. However, the structure of this material and the mechanism of the interesting effects on specific connective tissues have not been definitely established (3).
The intervertebral disks provide the third major example of a fibrocartilaginous joint. Here, however, the structuresare uniquely specialized with a characteristic nucleus pulposus contained within its collagenous anulus fibrosus to comprise each disk (4). True fibrocartilage is found only at the vertebral end plates that separate the nuclear pulposus from the trabecular bone within adjacent vertebral bodies. Intervertebral disks permit rotational as well as bending motions. Although motion at any one disk is modest and entirely consistent with bending, net movement becomes substantial because of the serial structure of the spine. No spinal segment normally moves very much, but no spinal segment moves alone. When all move together, significant motion occurs. Here, as in other fibrocartilaginous unions, the joints provide a highly stable bond while conferring a flexibility that is vital in the balance required for bipedalism and in protection against fracture. These last points are too often reinforced by the misfortune of patients with severe ankylosing spondylitis who suffer excessive fatigue and increased fracture risk as a result of pathological spinal fusion.
C. Diarthroses
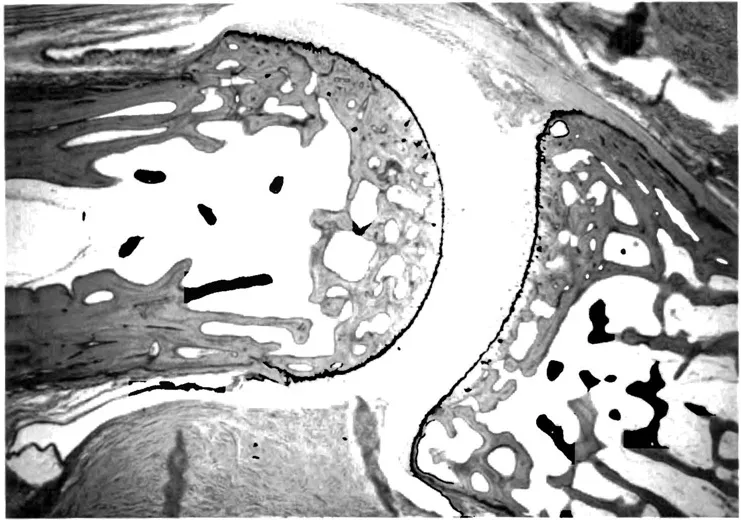
Synovial joints, or diarthroses, are by far the most common form of articulation between adjacent bones (5,6). Within this class of joints, a wide variety of designs accommodate a comparable spectrum of demands. All share, however, the features of a journal bearing: one opposing surface slides across or around its opposing mate. This fundamental feature is well shown in the interphalangeal joint illustrated in Figure 1. Synovial fluid and its requisite supporting synovial tissue are the body’s principal answer to the problem of musculoskeletal friction. Not only in joints, but also in bursae and tendon sheaths, synovial systems serve to enhance stable motion while they minimize friction between adjacent connective tissue components. This highly effective system of lubrication is reviewed in detail in Chapter 5.
A variety of different terms are sometimes used to classify different patterns of articular structure. Some of these (with examples of each) are ball and socket (hip), hinge (proximal interphalangeal). pivot (radiohumeral), plane (patellofemoral), ellipsoid (wrist), and saddle (first carpometacarpal). Each of these represents a different anatomic solution to a specific mechanical problem. In genera], they share the common design of relatively congruent opposing cartilaginous surfaces that slide over or around each other to achieve one or more specific motions and to distribute loading forces.
III. Joint Stability
A. Shape
In each case, several factors interact to maintain stability while the forces of muscle power and or gravity drive the joint through its required range of motion. The simplest of these stabilizing factors is shape (7). In the hip, for instance, not only gravity but also the force of virtually all muscles crossing the joint serve to drive the femoral head “ball” into its acetabular “socket.” This design permits a wide range of motion in three different axes (flexion-extension, abduction-adduction, and rotation), while still ensuring complete stability under virtually any stress. A wide range of variations among other convex-concave articulations serves the goal of enhanced stability. Particularly striking are the ankle mortise, where the adjacent fibula provides lateral stability, and the elbow joint, where a particularly deep ulnar concavity accommodates the distal humerus.
B. Ligaments
The stability of the ankle and humeroulnar joints do not depend solely on their shape. Like other “hinge” joints, these articulations are reinforced on both sides by strong collateral ligaments. These dense bands of collagenous tissue are fixed-length stays between adjacent bones that permit free flexion and extension while preventing significant motion in other axes. In other locations, such as the front of the hip, the back of the knee, and the flexor aspects of interphalangeal joints, broad, strong expansions of the articular capsule serve as ligamentous checks to prevent hyperextension.
Two further examples illustrate the variety of ligamentous stabilizers. The cruciate ligaments of the knee provide one of the more interesting examples. Here, the relatively long surfaces of the femoral condyles must slide across the tibial plateaus while they are loaded by forces equal to several times the total body weight. The cruciate ligaments enhance tracking throughout this course and reinforce both lateral and anterior-posterior stability during flexion and extension of this major weight-bearing joint (8). An entirely different variation is that provided by the transverse ligament of the atlas. Here, a strong ligament runs not between bones, but from one side of the atlas to the other. This unique structure holds the odontoid peg against the anterior ring and thus facilitates rotation while preventing backward subluxation of the odontoid into the spinal cord.
C. Muscles
Although a few ligaments, especially the ligamentum nuchae, contain considerable amounts of elastic tissue, most ligaments are relatively inelastic. They therefore serve to limit articular motion. When a joint is polyaxial, full freedom of motion is required and alternative means of stabilization must be used. Because muscles relax as well as contract, they can provide intermittent stabilization to normal joints. In the shoulder, this role is filled by the rotator cuff. Most muscles provide at least a measure of joint stability as they or their tendons cross the articulations that they drive. The cuff muscles take this role to its fullest. They position the humeral head within the shallow glenoid fossa while the overlying shoulder muscles take the arm through its full repertoire of purposeful motions (9).
D. Synovial Fluid
A final contribution to joint stability is that provided by the synovial fluid. Opposing surfaces of articular cartilage are normally separated by only a film of this “boundary layer” lubricant. This means that the system reduces friction primarily by binding layers of water to the contact surfaces. A well-established property of the boundary layer lubricants is their ability to serve as adhesives (10). They offer little or no resistance to shearing forces, such as those involved in normal joint motion, but they provide a strong defense against distraction. This mechanism seems likely to be an important factor in joint stability, especially in articulations like the hip where contact surfaces are large. The adhesive properties of synovial fluid require a small intraarticular volume. When the amount of synovial fluid increases, as in a pathological effusion, this stabilizing element is lost. This loss may be a significant contributor to the ligamentous laxity that often characterizes the chronically inflamed joint.
IV. Subchondral Bone
For the most part, one articular surface is convex and its mate is concave. This simple principle embodies important mechanical considerations. A convex surface represents, under load, the classic structure of a Roman arch. Loading forces tend to compact the constituent parts, and the load-bearing point, like the keystone of the arch, derives support from adjacent bone. It is for this reason that a convex surface can flex under load and yet can remain strong (11).
In contrast, loading forces inherently tend to distract the constituent parts of concave surfaces. If distraction occurs, the entire structure will fail. Wolfe’s law implies that there should be convex-concave differences in subchondral bone architecture that reflect these different stress patterns. This, in fact, is the case. Concave joint surfaces regularly overlie a thick “subchondral plate” supported by relatively coarse supporting struts of trabecularbone. The opposing convex member has a remarkably thin subchondral plate supported by a finely honeycombed trabecular mat...
Table of contents
- Cover
- Halftitle Page
- Title Page
- Copyright Page
- Foreword
- Preface
- Table of Contents
- Contributors
- Part I: Physiology of Joints
- Part II: Mechanics
- Part III: Neurophysiology
- Part IV: Pathophysiology
- Part V: Treatment
- Index
- About the Editors